Adriana Geremias Toni; Marcello Novoa Colombo Barboza; Guilherme Novoa Colombo Barboza
DOI: 10.17545/eoftalmo/2019.0016
ABSTRACT
Infectious keratitis is a leading cause of preventable visual loss worldwide and is a major challenge for ophthalmologists because of its limited prognosis. The objective of this study was to report the outcome of a patient with fungal keratitis who did not respond well to clinical pharmacological treatment and progressed to therapeutic corneal transplantation. Because of the limited response to treatment of fungal keratitis, each case should be analyzed separately, taking into account clinical and epidemiological criteria, to avoid possible irreversible complications.
Keywords: Keratitis; Corneal Ulcer; Corneal Injuries; Corneal Transplantation.
RESUMO
Ceratite infecciosa é uma das principais causas de perda visual evitável no mundo e a ceratite fúngica é um grande desafio para o oftalmologista, devido ao seu prognóstico limitado. O estudo objetivou relatar o desfecho de um paciente que cursou com ceratite fúngica e não respondeu bem ao tratamento clínico farmacológico evoluindo para transplante terapêutico de córnea. Devido à limitação que temos em relação à resposta ao tratamento da ceratite fúngica, deve-se analisar cada caso isoladamente, levando em consideração critérios clínicos e epidemiológicos, para que se possa evitar possíveis complicações irreversíveis.
Palavras-chave: Ceratite; Úlcera da Córnea; Lesões da Córnea; Transplante de Córnea.
RESUMEN
La queratitis infecciosa es una de las principales causas de pérdida visual evitable en el mundo y la queratitis fúngica es un gran desafío para el oftalmólogo, debido a su pronóstico limitado. El estudio buscó relatar el caso de un paciente que ingresó con queratitis fúngica y no respondió bien al tratamiento clínico farmacológico, evolucionando a un trasplante terapéutico de córnea. Debido a la limitación que tenemos con relación a la respuesta al tratamiento de la queratitis fúngica, se debe analizar cada caso de manera aislada, considerando criterios clínicos y epidemiológicos, para que se puedan evitar posibles complicaciones irreversibles.
Palabras-clave: Queratitis; Úlcera de la Córnea; Lesiones de la Cornea; Trasplante de Córnea.
INTRODUCTION
Infectious keratitis is one of the leading causes of preventable visual loss worldwide1. The incidence of infectious keratitis is variable; however, the disease is more common in hot climates and is associated with trauma and the use of corticosteroids, antibiotics, and contact lenses2,3. The initial diagnosis is clinical and based on clinical history, physical examination of the eye, development of a diagnostic hypothesis, and drug treatment2. However, the gold-standard diagnosis is the laboratory analysis of corneal culture and isolation of the pathogenic agent4. Another approach is the use of molecular biology techniques, including polymerase chain reaction, which allows obtaining faster results5,6. In vivo confocal microscopy has gained attention because of its high sensitivity in detecting larger organisms, such as filamentous fungi and bacteria Acanthamoeba and Nocardia7-11. Additionally, optical coherence tomography of the anterior segment can provide an objective measurement of the corneal infiltrate, scar size, and degree of corneal thinning12,13.
Bacteria are the most common causative agents of infectious keratitis, including Staphylococcus aureus, coagulase-negative staphylococci, Streptococcus sp., and Pseudomonas aeruginosa14. Fungi are responsible for 5% to 25% of all cases of infectious keratitis, with Aspergillus sp. and Fusarium sp. being the most commonly diagnosed agents6,15. The clinical picture of keratitis cases caused by fungal infections is usually similar to that of bacterial infections. Nonetheless, a fungal etiology may be considered when the patient has a history of trauma involving plant matter and insidious evolution. Another cause of keratitis is infection with Acanthamoeba, and the main risk factor is the use of contact lenses 16. Viral keratitis is caused primarily by herpes simplex and varicellazoster viruses17.
Fungal keratitis is a major challenge for ophthalmologists because of its limited prognosis. Fungi usually do not penetrate an intact cornea, but can penetrate ruptured epithelium. Some of the risk factors most strongly associated with fungal infections of the eye are trauma, use of contact lenses, systemic diseases, and immunodepression14,18.
The objective of this study is to report the outcome of a patient with fungal keratitis that did not respond well to pharmacological treatment, requiring corneal transplantation with good postoperative results.
CASE REPORT
This case involved a 52-year-old Caucasian male patient working as a merchant.
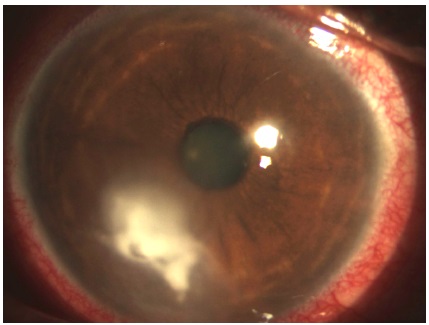
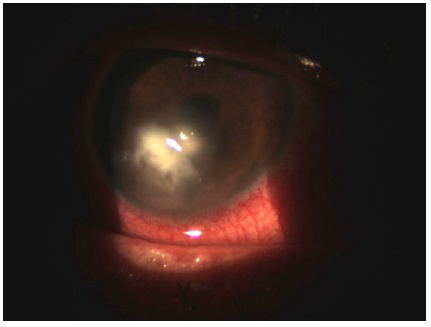
The patient complained of intense right eye (RE) pain lasting 15 days. He reported that sawdust fell on the RE 15 days prior. He sought medical care after 3 days, when the foreign body was removed and a topical antibiotic (gatifloxacin 0.5%, every 2 hours) and a topical association of an antibiotic and an anti-inflammatory agent (moxifloxacin 0.5% and dexamethasone 0.1%, every 6 hours) were prescribed. However, the clinical status progressively worsened, leading to ocular redness, intense pain, photophobia, and a white spot on the cornea. The patient had no comorbidities, but underwent vasectomy surgery. There was no significant family history. On physical examination, the best corrected visual acuity was 20/200 and 20/25. Intraocular pressure was 16 mmHg in both eyes. Biomicroscopy of the RE showed conjunctival hyperemia (grade 2+ to 4+), an ulcerative lesion in the inferior quadrant of the cornea with an underlying dense infiltrate (6 × 4 mm), irregular edges, and corneal thinning (2 × 2 mm) (Figure 1). Examination of the left eye was unremarkable.
Therapeutic management included 1) interruption of topical corticosteroid treatment; 2) substitution of topical gatifloxacin 0.05% with topical fortified cephalothin 50 mg/mL and fortified gentamicin 14 mg/mL, both every 2 hours; 3) corneal culture; and 4) orientation for daily returns.
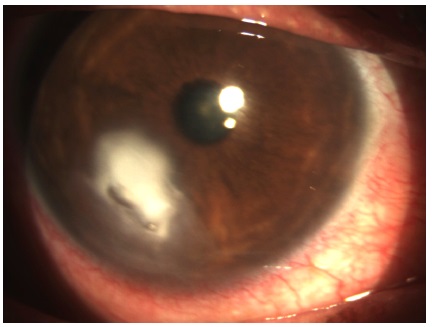
On day 5 of follow-up, the microbial culture was positive for Streptococcus sp. and negative for fungal infection, and the antibiogram indicated sensitivity to common antibiotics. The patient reported improvement of the pain. Biomicroscopy of the RE revealed an infiltrate in the central cornea and a decrease in the inflammatory halo (Figure 2). The drug treatment was maintained with daily returns.
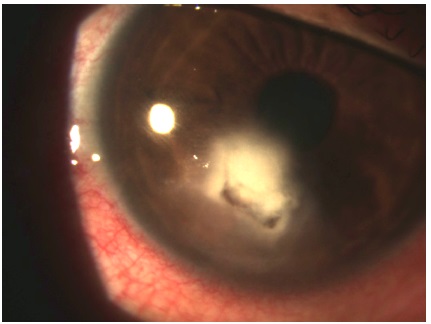
On day 11 of follow-up, the patient reported increased photophobia, worsening of pain, and persistence of white spots. Biomicroscopy of the RE showed a concentration of dense infiltrate, corneal thinning, and an infectious inflammatory halo in the inferior cornea (Figure 3). This suggested a worsening of the condition and a lack of response to the previous drug treatment. The hypothesis of fungal keratitis was then considered because of the patient’s clinical history. Therapeutic management consisted of prescription of topical natamycin 5% every 4 hours and oral ketoconazole 400 mg and maintainance of other drugs with daily returns.
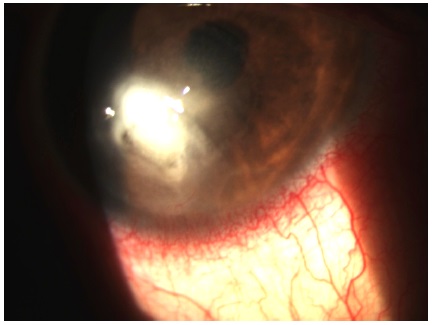
On day 20 of follow-up, the patient returned with an improvement in pain. On biomicroscopy, the RE presented a dense infiltrate and a circular inflammatory halo 5 mm in diameter in the superior cornea (Figure 4). The medication and daily returns were maintained.
On day 30 of follow-up, biomicroscopy examination of the RE indicated the presence of anterior chamber reaction (cells 2+), Descemet’s membrane folds (grade 2+), thinning of the inferior cornea by 2/3 of normal thickness, and satellite lesions in the superior region of the dense inflammatory halo (Figure 5). Therapeutic management included a new microbial culture, interruption of drug treatment with natamycin, initiation of topical amphotericin B 0.15% every 3 hours, and maintenance of other medications and dosages.
On day 32 of follow-up, the patient reported an improvement in pain. All microbial cultures were negative. The dosage of antibiotics was reduced (topical cephalothin 50 mg/mL and topical gentamicin 14 mg/mL every 4 hours), while amphotericin B 0.15% frequency of administration was increased from every 3 hours to every hour.
On day 35 of follow-up, the patient was anxious, reported having poor sleep, and refused to continue with the drug therapy. Biomicroscopy of the RE showed hypopyon, severe corneal thinning (thickness less than 2/3 of normal), and a dense infiltrate in the posterior cornea (endothelium). The chosen therapeutic intervention was corneal transplantation.
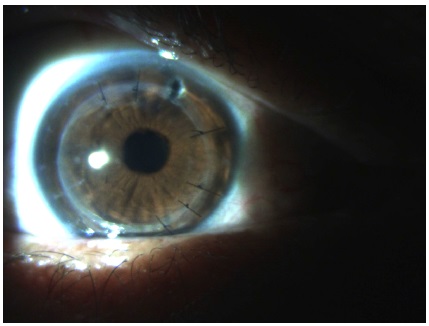
The patient progressed well after transplantation, with total regression of the infectious disease (Figure 6). Amphotericin B 0.15% was administered during the surgical procedure. The patient presented no further infiltrative lesions. Topical amphotericin B 0.15% (every 3 hours) was maintained until day 10 after surgery, and a topical corticosteroid (prednisolone acetate 1.0% every 3 hours) was started after 30 days of the procedure. Histopathological examination of the transplanted corneal bud revealed the presence of fungal hyphae, chlamydospores, and rare Gram-positive cocci, while corneal culture on Sabouraud dextrose agar revealed the presence of the fungus Fusarium solani.
DISCUSSION
Based on the most common causative agents, the appropriate empirical treatment in the present case was broad-spectrum antibiotic therapy to eradicate the leading bacterial pathogens causing keratitis, including Staphylococcus aureus, coagulase-negative staphylococci, Streptococcus sp., and Pseudomonas aeruginosa14. Although the study patient had a history of trauma involving plant matter, the main hypothesis was bacterial keratitis because of its high prevalence relative to other agents4,5,14. In addition to the introduction of broadspectrum antibiotics, the immediate therapeutic conduct was interrupting the corticosteroid therapy previously prescribed to the patient, because the use of corticosteroids is associated with worsening of fungal keratitis19. Drug therapy was maintained because of the favorable outcome in the first few days of follow-up. However, on day 11 of follow-up, the symptoms worsened, and biomicroscopy showed a 5-mm inflammatory halo in the inferior cornea, suggesting worsening of the clinical status.
Despite the negative culture for fungal isolates, topical natamycin 5% every 4 hours was prescribed to treat filamentous fungi (Fusarium spp and Aspergillus spp), which are the primary causative agents of fungal keratitis, as well as ketoconazole 400 mg orally to treat yeast infections (Candida spp. and Cryptococcus spp.). Sequential corneal epithelial scrapings were performed at the edges of the lesion, outside the thinned area, to improve the dermal penetration of natamycin.
On day 30 of follow-up, corneal thinning of 2/3 of the normal thickness in the inferior cornea and a satellite lesion were observed, which are highly suggestive of fungal infection. Based on the results of eye physical examination, natamycin 5% was interrupted and topical amphotericin B 0.15% (every 3 hours) was introduced. After 2 days, the patient reported an improvement in ocular pain, and the frequency of amphotericin B 0.15% was increased from every 3 hours to every hour. On day 35 of follow-up, clinical worsening became evident with the appearance of hypopyon, severe corneal thinning (considered severe in cases in which ulcers with a diameter ≥ 4 mm or deeper than 2/3 of the normal thickness are observed in the central cornea) and a dense infiltrate in the posterior cornea. On the basis of this diagnosis, the patient became anxious and did not agree with the continuation of drug therapy. Therefore, corneal transplantation was performed.
Most antifungal agents are fungistatic, and patients are required to undergo prolonged treatment and have preserved immunity. Treatment may be extended for weeks or even months10. Clinical improvement may not be evident for several days. However, because of the difficult disease management, it is often necessary to resort to surgical treatment to avoid possible endophthalmitis and more severe consequences, such as evisceration or enucleation. The timing of transplantation indication is essential for visual prognosis.
Based on the present case, some topics on ophthalmological practice need to be addressed, including the importance of microbial culture for correct therapeutic management and the ideal time to decide for corneal transplantation. The results of the present case indicate that no rules can be generalized. The outcome of fungal keratitis is a major challenge in clinical practice. The ophthalmologist should evaluate and interpret epidemiological and clinical data for timely decision-making, because many cases may progress to a rapidly spreading infection and blindness.
REFERENCES
1. Whitcher JP, Srinivasan M, Upadhyay MP. Corneal blindness: a global perspective. Bull World Health Organ. 2001;79(3):214-21.
2. Mabon M. Fungal keratitis. Int Ophthalmol Clin. 1998 fall;38(4):115-23.
3. Wilhelmus KR, Robinson NM, Font RA, Hamill MB, Jones DB. Fungal Keratitis in contact lens wearers. Am J Ophthalmol. 1988 dec;106(6):708-14.
4. McLeod SD, Kolahdouz-Isfahani A, Rostamian K, Flowers CW, Lee PP, McDonnell PJ. The role of smears, cultures, and antibiotic sensitivity testing in the management of suspected infectious keratitis. Ophthalmology. 1996 jan;103(1):23-8.
5. Austin A, Lietman T, Rose-Nussbaumer J. Update on the Management of Infectious Keratitis. Ophthalmology. 2017 nov;124(11):1678-1689.
6. Chang HY, Chodosh J. Diagnostic and therapeutic considerations in fungal keratitis. Int Ophthalmol Clin. 2011 fall;51(4):33-42.
7. Nielsen E, Heegaard S, Prause JU, Ivarsen A, Mortensen KL, Hjortdal J. Fungal keratitis - improving diagnostics by confocal microscopy. Case Rep Ophthalmol. 2013 sep/dec;4(3):303-310.
8. Avunduk AM, Beuerman RW, Varnell ED, Kaufman HE. Confocal microscopy of Aspergillus fumigatus keratitis. Br J Ophthalmol. 2003 apr;87(4):409- 410.
9. Das S, Samant M, Garg P, Vaddavalli PK, Vemuganti GK. Role of confocal microscopy in deep fungal keratitis. Cornea. 2009 jan;28(1):11-3.
10. Kanavi MR, Javadi M, Yazdani S, Mirdehghanm S. Sensitivity and specificity of confocal scan in the diagnosis of infectious keratitis. Cornea. 2007 aug;26(7):782-6.
11. Vaddavalli PK, Garg P, Sharma S, Sangwan VS, Rao GN, Thomas R. Role of confocal microscopy in the diagnosis of fungal and acanthamoeba keratitis. Ophthalmology. 2011 jan;118(1):29-35.
12. Konstantopoulos A, Kuo J, Anderson D, Hossain P. Assessment of the use of anterior segment optical coherence tomography in microbial keratitis. Am J Ophthalmol. 2008 oct;146(4):534-542.
13. Martone G, Pichierri P, Franceschini R et al. In vivo confocal microscopy and anterior segment optical coherence tomography in a case of alternaria keratitis. Cornea. 2011 apr;30(4):449-53.
14. Green M, Apel A, Stapleton F. Risk factors and causative organisms in microbial keratitis. Cornea. 2008 jan;27(1):22-7.
15. Mabon M. Fungal keratitis. Int Ophthalmol Clin. 1998 fall;38(4):115-23.
16. Alvarenga LS, Freitas D, Hofling-Lima AL. Ceratite por Acanthamoeba. Arq Bras Oftalmol. 2000 apr;63(2):155-159.
17. Freitas D, Alvarenga L, Lima ALH. Ceratite herpética. Arq Bras Oftalmol. 2001;64:81-6.
18. Wilhelmus KR, Robinson NM, Font RA, Hamill MB, Jones DB. Fungal Keratitis in contact lens wearers. Am J Ophthalmol. 1988;106:708-14.
19. Oliveira PR, Resende SM, Oliveira FC, Oliveira AC. Fungal keratitis. Arq Bras Oftalmol. 2001;64:75-9.



Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 4, 2018.
Accepted on:
April 10, 2019.