Juliana Moreira de Santana1; Cristina Baracuhy de Melo2; Maria Isabel Lynch Gaete3; Gabriel Sales Lima de Carvalho4
DOI: 10.17545/eoftalmo/2019.0015
ABSTRACT
IgG4-related disease, a recently described systemic inflammatory disease, should be considered during the assessment of patients with nonspecific orbital inflammation. For this condition, orbital biopsy is necessary to establish a diagnosis, and it usually shows lymphoplasmacytic infiltration, fibrosis, and varying degrees of eosinophilia.
Keywords: Orbit; Inflammation; Immunosuprression.
RESUMO
A doença relacionada a IgG4 é uma doença inflamatória sistêmica recentemente descrita que deve ser considerada na avaliação de pacientes com inflamação orbital inespecífica. A biópsia da órbita é necessária para estabelecer um diagnóstico e normalmente demonstra infiltração linfoplasmocitária, fibrose e graus variáveis de eosinofilia.
Palavras-chave: Órbita; Inflamação; Imunossupressão.
RESUMEN
La enfermedad relacionada con IgG4 es una enfermedad inflamatoria sistémica que ha sido descrita recientemente y debe ser considerada en la evaluación de pacientes con inflamación orbital inespecífica. La biopsia de la órbita se hace necesaria para establecer un diagnóstico y, normalmente, demuestra infiltración linfoplasmocitaria, fibrosis y grados variables de eosinofilia.
Palabras-clave: Órbita; Inflamation; Inmunosupresión.
INTRODUCTION
IgG4-related disease is a recently recognized systemic inflammatory disease. It can affect ≥1 organs, causing tumefactive lesions or fibrosis with many clinical manifestations depending on the organ/system involved. The orbit may be involved in 4%–34% of cases1,2. At present, its pathogenesis remains partially understood, with autoimmunity and infectious agents being the potential immunologic triggers. Several cytokines contribute to the increase in the production of IgG4 and, to a lesser extent, of IgE and eosinophilia as well as fibrosis progression—all of which are the characteristics of the disease3. Here, we report the case of a patient with orbital inflammation as the primary manifestation of this disease.
METHODS
In this descriptive study classified as a case report, data were collected from the anamnesis and additional examinations of the patient conducted at Hospital das Clínicas of the Federal University of Pernambuco.
RESULT
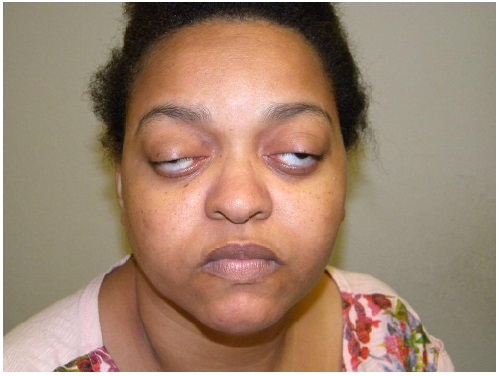
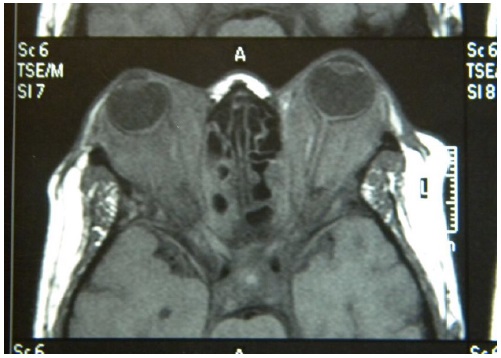
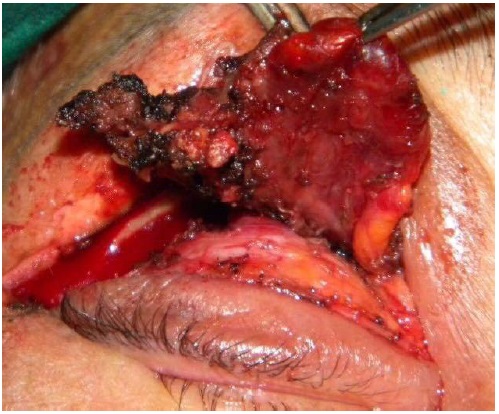
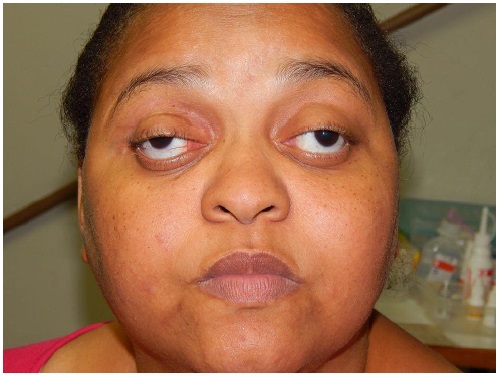
A 33-year-old woman named E.N.S. from Recife (Pernambuco, Brazil) with recent gradual vision impairment in the left eye associated with ptosis and restricted movement of both eyes visited our outpatient clinic. She had a history of loss of vision in the right eye for 3 years but reported no systemic disease. Ophthalmologic examination showed OD amaurosis and OS hand movement, total restricted eye movements, marked proptosis, and severe ptosis in both eyes (Figure 1) as well as impaired pupillary reflexes. Orbital magnetic resonance imaging showed bilateral proptosis with a diffuse infiltrative solid lesion, intraconal and extraconal involvement, optic nerve compression, and affected extraocular muscles (Figure 2). Laboratory tests showed increased serum CRP, ESR, and IgG levels. Orbital incisional biopsy (Figure 3) revealed histopathological evidence of fibrosis and nonspecific chronic inflammatory infiltrates, with no signs of lymphoproliferative or granulomatous disorders. Immunohistochemical analysis showed positive results for IgG4, thereby confirming the diagnosis of IgG4-related disease. Treatment with 60 mg/day prednisone was initiated without a satisfactory response. Therefore, rituximab was subsequently administered, resulting in an improvement of the patient’s medical condition (Figure 4).
DISCUSSION
IgG4-related disease is characterized by varying degrees of fibrosis and diffuse lymphoplasmacytic infiltration of IgG4. This underlying pattern is modified by the tissue microstructure and lesion age. Lymphoplasmacytic infiltrates tend to be more intense in early lesions and are composed of polyclonal T lymphocytes, IgG4 plasma cells, and diffuse eosinophils4,5.
Development of nodules and masses, focal or diffuse, found on physical or radiological examination is the main clinical sign of the disease. Painless eyelid edema is the symptom observed in the majority of cases. Proptosis with/without diplopia is also common. Visual acuity is generally not impaired, but compression of the optic nerve causing blindness has been reported6.
In IgG4-related disease, ophthalmologic involvement is common and can affect nearly the whole anatomical structure of the orbit. Diagnosis can be achieved using the newly defined criteria based on the biopsy of orbital or extraorbital disease. IgG4-related disease can be definitively diagnosed in patients with (1) organ enlargement or dysfunction, (2) serum IgG4 concentration above 135 mg/dl, and (3) histopathological findings of >10 IgG4 cells/ high-power field and IgG4/IgG ratio of >40%7. Patients who cannot be diagnosed based on these criteria can be re-diagnosed using specific criteria for each organ. Histopathology is the key component and indispensable for the diagnosis of IgG4-related disease. The diagnosis is strongly based on biopsy results showing infiltration rich in plasma cells positive for IgG4, storiform fibrosis, obliterative phlebitis, and moderate eosinophilia, all of which are frequently observed in the tissues of these patients8,9. The precise diagnosis of IgG4-related disease has important implications for its prognosis and treatment, particularly with the discovery of rituximab as an effective steroid-sparing agent10. Idiopathic orbital inflammation has long posed a management challenge, with recurrences in up to 50% of the cases11. Identifying cases of IgG4-related disease is important because the lesions can be highly responsive to biological therapy12.
REFERENCES
1. Souza VS, Cruz PM, Marques VB, Sampaio LR. Doença inflamatória da órbita relacionada à IgG4. Rev Bras de Reumato. 2017 aug;57(Suppl 1):S265.
2. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012 feb;366(6):539-51.
3. Kumar V, Abbas AK, Aster JC. Doenças do sistema imunológico. In: Kumar V, Abbas AK, Aster JC. Robbins & Cotran Patologia: Bases patológicas das doenças. 8a ed. Rio de Janeiro: Elsevier; 2010. p.234.
4. Smyrk TC. Pathological features of IgG4-related sclerosing disease. Curr Opin Rheumatol. 2011;23:74–79.
5. Deshpande V, Zen Y, Chan JK et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol. 2012 sep;25(9):1181-92.
6. Cheuk W, Yuen HK, Chan JK. Chronic sclerosing dacryoadenitis: part of the spectrum of IgG4-related Sclerosing disease?. Am J Surg Pathol. 2017 apr;31(4):643-5.
7. Aggarwal R, Ringold S, Khanna D, Neogi T, Johnson SR, Miller A et al. Distinctions between diagnostic and classification criteria?. Arthritis Care Res (Hoboken). 2015 jul;67(7):891-7.
8. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med. 2012 feb;366(6):539-51.
9. Umehara H, Okazaki K, Stone JH, Kawa S, Kawano M. Comprehensive diagnostic criteria for IgG4-related disease. In: Umehara H et al. (Eds.). IgG4- -related disease. Tokyo: Springer Japan; 2013. p.35-39.
10. Wallace ZS, Deshpande V, Stone JH. Ophthalmic manifestations of IgG4-related disease: single-center experience and literature review. Semin Arthritis Rheum. 2014 jun;43(6):806-817. Available from: https://doi.org/10.1016/j.semarthrit.2013.11.008
11. Lindfield D, Attfield K, McElvanney A. Systemic immunoglobulin G4 (IgG4) disease and idiopathic orbital inflammation; removing ‘idiopathic’ from the nomenclature?. Eye (Lond). 2012 may;26(5):623-629.
12. Khosroshahi A, Carruthers MN, Deshpande V, Unizony S, Bloch DB, Stone JH. Rituximab for the treatment of IgG4-related disease: lessons from 10 consecutive patients. Medicine (Baltimore). 2012 jan;91(1):57-66.




Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 5, 2018.
Accepted on:
May 9, 2019.