Ruth Miyuki Santo1; Fernando Eiji Sakassegawa-Naves2; Richard Yudi Hida3
DOI: 10.17545/e-oftalmo.cbo/2016.54
ABSTRACT
Blepharitis is one of the most common conditions seen in ophthalmological practice. The term represents a spectrum of diseases characterized by varying degrees of eyelid inflammation, and the predominant symptoms include itching, a burning sensation, and ocular discomfort. Though very common, blepharitis is not completely defined, and its exact physiopathological mechanisms are not yet established. Blepharitis offers a diagnostic and therapeutic challenge. Distinctions between different clinical manifestations may be subtle or may overlap and may have a relevant impact on treatment. Moreover, a universal classification system for blepharitis remains unavailable. Although the condition does not typically create risks for patients’ vision, complaints of occular irritation and discomfort may be so persistent that they may have a relevant impact on quality of life. Mites from the genus Demodex are thought to be involved in some blepharitis cases resistant to conventional treatment. The objective of this review is to discuss the role of Demodex mites as agents associated with chronic blepharitis, as well as the physiopathological mechanisms underlying the condition, its diagnosis, and its treatment.
Keywords: Blefarite: Olho: Inflamação: Ácaros: Qualidade de Vida.
RESUMO
Blefarite é uma das condições mais frequentes nos consultórios oftalmológicos. Representam um espectro de doenças caracterizadas por graus variados de inflamação palpebral e os sintomas predominantes incluem prurido, sensação de queimação e desconforto ocular. Embora muito comum, permanece como uma condição não completamente definida e seus mecanismos fisiopatológicos requerem total elucidação. As blefarites constituem um desafio diagnóstico e terapêutico. Distinções entre as diferentes manifestações clínicas podem ser sutis ou sobrepostas e podem ter impacto relevante no tratamento. Até o presente momento não há uma classificação universal. Embora a condição, na maioria das vezes, não seja de risco para a visão, as queixas de irritação ocular e desconforto aos esforços visuais podem ser tão persistentes que podem ter repercussão relevante na qualidade de vida. Alguns casos refratários ao tratamento convencional podem ter a participação do ácaro Demodex. A presente revisão tem como objetivos discutir o papel do Demodex como agente associado às blefarites crônicas, a fisiopatogênese da condição, o diagnóstico e tratamento.
Palavras-chave: Blefarite: Olho; Inflamação: Ácaros: Qualidade de Vida.
INTRODUÇÃO
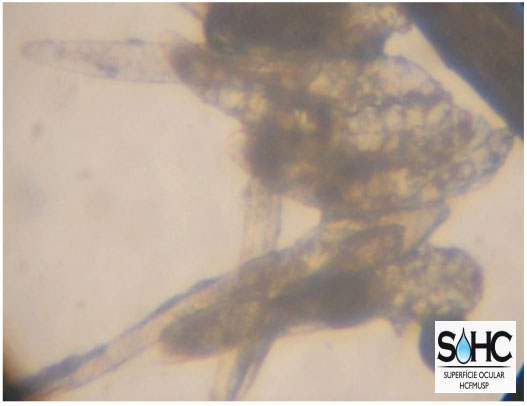
Chronic cases of blepharitis are a common occurrence in ophthalmological practice. The term represents a spectrum of diseases characterized by varying degrees of eyelid inflammation, and the predominant symptoms include itching, a burning sensation, and ocular discomfort. Blepharitis is diagnostically and therapeutically challenging. Distinctions between different clinical manifestations may be subtle or may overlap and may have a relevant impact on treatment. A universal classification system for blepharitis remains unavailable. The condition is often neglected not only by patients but also by ophthalmologists, and may be the source of substantial dissatisfaction. In some cases, complaints of ocular irritation and discomfort are so persistent that they may affect quality of life, even after treatment for blepharitis and dry eye. It is important to remember that blepharitis may be caused by a mite from the genus Demodex (Photo 1).

Demodex and blepharitis
Species in the genus Demodex-from the Greek roots dēmos ("fat") and dēx ("worm")–are microscopic ectoparasites from the class Arachnida and the subclass Acarina that colonize pilosebaceous units. Demodex species are the most common permanent parasite in humans.1 Of the many species, only two have been described on the surface of the human body: D. folliculorum and D. brevis. Adult mites are between 0.3 and 0.4 mm in length. D. brevis is slightly smaller than D. folliculorum.2 Demodex mites tend to be found on the face, cheeks, forehead, nose, and external acoustic meatus, where the consistent sebum secretion acts as a food source and a favorable habitat for reproduction. Because these structures surround the eye, the eyelids are also easily colonized by these agents. Older adults and individuals with rosacea are more likely to harbor these mites. In and around the eye, D. folliculorum is found on the infundibular portion of the eyelash follicles, and Demodex brevis is found on the sebaceous gland ducts of the upper eyelashes and the Meibomian glands.3 Lower Demodex counts can be found on asymptomatic individuals.4 In most cases, the mites go undetected, with no adverse symptoms: however, in certain situations (typically those involving immunosuppression caused by stress or disease), mite populations may drastically increase, which results in a condition known as demodicosis, characterized by itching and inflammation.
Demodex was detected more than 150 years ago (by Simon in 1842), but its role in the development of chronic blepharitis has recently become a topic of interest and the subject of numerous studies, particularly in the last 10 years. Rodriguez et al. 5 found that 75% of patients with chronic blepharitis had Demodex on their eyelashes and often had much higher counts than healthy individuals. The relationship between blepharitis and Demodex infestation has been confirmed by other researchers 6,7 and a recent meta-analysis found that patients with Demodex on their eyelashes are 4.7 times more likely to develop symptomatic blepharitis.8 Clinical improvement after treatments to decrease Demodex populations also corroborates the existence of the clear correlation between the development of blepharitis and Demodex infestation.9
Blepharitis caused by Demodex may be either anterior (eyelash region) or posterior (Meibomian glands). The physiopathological mechanism underlying the inflammatory process is the direct action of the mite, the action of bacteria (the mite serves as a vector), or a hypersensitivity reaction. Mites cause distension of the follicles, microabrasions on the skin around the follicles using their scales, and obstruction of the orifices of the Meibomian glands. They may cause recurrent chalazia and evaporative dry eye. The mites also serve as vectors by carrying bacteria, including streptococci and staphylococci, on their surface. Antigens produced by these bacteria can cause an antigen-antibody reaction, with the development of sterile infiltrates in the periphery of the cornea (catarrhal ulcers) or phlyctenular keratoconjunctivitis, especially in patients with rosacea. The skeletal proteins and excretory products of mites may induce late hypersensitivity, with T lymphocyte recruitment and cytokine release.10,11
Diagnosis of blepharitis associated with the presence of Demodex
The diagnosis of blepharitis associated with Demodex is based on three criteria: (1) Clinical history: blepharitis, blepharokeratoconjunctivitis, or recurrent chalazia resistant to conventional treatment; (2) Slit lamp examination results: presence of cylindrical “dandruff” at the root of the eyelashes (Photo 2); (3) Results of the examination of eyelashes by optical microscopy: detection of adult mites or larvae (Photo 3).

Treatment for blepharitis associated with the presence of Demodex
Demodex is resistant to a variety of common antiseptic solutions, including 70% ethanol and 10% povidone-iodine, as well as antimicrobial agents such as erythromycin and metronidazole. The literature has shown that the use of tea tree oil in eyelid hygiene is a safe and effective treatment for blepharitis caused by Demodex12 and has advantages over the use of neutral shampoo: it not only removes external “dandruff” but also stimulates migration of the mites from the follicles to the cutaneous surface. In addition to eradicating Demodex, treatment with tea tree oil provides substantial relief of ocular irritation symptoms and often resolves eyelid inflammation.13 Tea tree oil is a natural oil extracted from the leaf of the Melaleuca alternifolia plant, and it has antibacterial, antifungal and anti-inflammatory properties 14 It therefore complements the treatment of blepharitis.
In a recent study, Holzchuh et al. demonstrated that systemic ivermectin may be very useful as a complement to the treatment of Demodex infestation, especially in cases in which patients fail to comply with the necessary eyelid hygiene regimen. In Holzchuh et al.’s study, a substantial reduction in the number of mites found on eyelashes was observed, along with a statistically significant improvement in clinical parameters such as tear film rupture time and ocular surface coloration. As treatment, a single dose of oral ivermectin (200 µg/kg: 6 mg tablets) was administered, which was repeated after 1 week.
CONCLUSIONS
Blepharitis offers a diagnostic and therapeutic challenge. Some cases that are resistant to conventional treatment may involve mites from the genus Demodex. Blepharitis caused by Demodex may be either anterior (eyelash region) or posterior (Meibomian glands). The physiopathological mechanism underlying the inflammatory process is the direct action of the mite, the action of bacteria (the mite serves as a vector), or a hypersensitivity reaction. The diagnosis of blepharitis associated with Demodex is based on three criteria; (1) Clinical history: blepharitis, blepharokeratoconjunctivitis or recurrent chalazia resistant to conventional treatment; (2) Slit lamp examination results: presence of cylindrical “dandruff” at the root of the eyelashes; (3) Results of the examination of the eyelashes by optical microscopy: detection of larvae or adult mites. Treatment includes the use of tea tree oil as part of the eyelid hygiene regimen, but it requires patient compliance. Ivermectin may be very useful as a complement to the treatment of Demodex infestation, especially in cases in which patients fail to comply with the necessary eyelid hygiene regimen.
REFERENCES
1 Boge-Rasmussen T, Christensen JD, Gluud B, Kristensen G, Norn MS. Demodex folliculorum hominis (Simon): incidence in a normomaterial and in patients under systemic treatment with erythromycin or glucocorticoid. Acta Derm Venereol 1982; 62:454-456. PMid:6183907
2. Rufli T, Mumcuoglu Y. The hair follicle mites Demodex folliculorum and Demodex brevis: biology and medical importance. A review. Dermatological 1981; 162:1-11. https://doi.org/10.1159/000250228
3. English FP, Nutting WB. Demodicosis of ophthalmic concern. Am J Ophthalmol 1981 ; 91:362-372. https://doi.org/10.1016/0002-9394(81)90291 -9
4. Norn MS. Demodex folliculorum. Incidence and possible pathogenic role in the human eyelid. Acta Ophthalmol Suppl 1970;108:7-85. PMid:4322592
5. Rodriguez AE, Ferrer C, Alió JL. Chronic blepharitis and Demodex. Arch Soc Esp Oftalmol 2005; 80:635-42. https://doi.org/10.4321/S0365-66912005001100004
6. Kemal M, Sümer Z, Toker MI, Erdogan H, Topolkara A, Akbulut M. The prevalece of Demodex folliculorum in blepharitis and the normal population. Ophthalmic Epidemiol 2005; 12:287-90. https://doi.org/10.1080/092865805910057
7. Rusiecka-Ziólkowska J, Nokiel M, Fleischer M. Demodex - An Old Pathogen or a New One? Adv Clin Exp Med 2014; 23:295-8. https://doi.org/10.17219/acem/37081
8. Zhao YE, Wu LP, Hu L et al. Association of blepharitis with Demodex: a metaanalysis. Ophthalmic Epidemiol 2012; 19:95-102. https://doi.org/10.3109/09286586.2011.642052
9. Holzchuh FG, Hida RY, Moscovoci BK, Albers MBV, Santo RM, Kara-José N, Holzchuh R. Clinical Treatment of Ocular Demodex folliculorum by Systemic Ivermectin Am J Ophthalmol 2011;151:1030-4.
10. Liu J, Sheha H, Tseng SCG. Patogenic role of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol 2010; 10:505-10. https://doi.org/10.1097/ACI.0b013e32833df9f4
11. Kim JH, Chuan YS, Kim JC. Clinical and immunological responses in ocular demodecosis. J Korean Med Sci 2011 ; 26:1231 -7. https://doi.org/10.3346/jkms.2011.26.9.1231
12. Gao Y-Y, Di Pasquale MA, Li W, et al. In vitro and in vivo killing of ocular Demodex by tea tree oil. Br J Ophthalmos 2005; 59:113-25. https://doi.org/10.1136/bjo.2005.072363
13. Koo H, Kim TH, Kim KW, Wee SW, Chun YS, Kim JC. Ocular Surface Discomfort and Demodex: Effect of Tea Tree Oil Eyelid Scrub in Demodex Blepharitis. J Korean Med Sci 2012; 27:1574-9. https://doi.org/10.3346/jkms.2012.27.12.1574
14. Carson CF, Hammer KA, Riley TV. Melaleuca alternifolia (Tea Tree) Oil: a Review of Antimicrobial and Other Medicinal Properties. Clin Microbial Rev 2006; 19: 50-62. https://doi.org/10.1128/CMR.19.1.50-62.2006

Fonte de financiamento: declaro não haver.
Conflicts of interest: The authors declare that there are no conflicts of interest associated with this publication
Received on:
May 16, 2016.
Accepted on:
May 16, 2016.