Juliana Ishii Iguma1; Camila Ishii Iguma2; José Vital Filho1; Ivana Lopes Romero Kusabara1
DOI: 10.17545/eOftalmo/2024.0016
ABSTRACT
Childhood ocular orbital tumors significantly increase morbidity and mortality, which is why knowledge of their epidemiology is essential in health care planning. This study aimed to evaluate the epidemiological profile of childhood ocular orbital tumors, their signs and symptoms, and the agreement between the clinical and histological diagnoses in a Brazilian tertiary ophthalmology department. This was a retrospective study based on medical records from Santa Casa de São Paulo from 2017 to 2022. We included children up to 14 years of age with a diagnosis or suspicion of an ocular orbital tumor and evaluated the agreement between the clinical and histological diagnoses when possible. Fifty patients were included, of which 25 were female and 25 were male. The mean age at admission was 5.76±4.4 years, and at the onset of the condition, it was 3.52±3.80 years. Laterality was 50% in the right eye, 46% in the left eye, and 4% bilateral. The most frequent tumors were hemangioma (20%), venolymphatic malformation (18%), and retinoblastoma (12%). The tumors that occurred more frequently were benign. There was no statistical difference in the demographic characteristics, except age at diagnosis and time from symptoms to treatment, which were significantly lower in malignant tumors. According to the Kappa coefficient, the agreement between the clinical and histological diagnoses was moderate.
Keywords: Orbital tumors; Orbital diseases; Optic nerve tumors; Exophthalmos; Epidemiology.
RESUMO
Os tumores óculo-orbitários infantis podem aumentar significativamente a morbidade e a mortalidade, por isso o conhecimento da epidemiologia é essencial no planejamento da assistência à saúde. O objetivo deste estudo é avaliar o perfil epidemiológico dos tumores óculo-orbitários infantis, seus sinais e sintomas, bem como a correlação clínica e histopatológica em um serviço oftalmológico terciário brasileiro. Estudo retrospectivo, com avaliação de prontuários da Santa Casa de São Paulo, de 2017 a 2022. Incluímos crianças até 14 anos incompletos com diagnóstico ou suspeita de tumor óculo-orbitário. Avaliamos a concordância do diagnóstico clínico com o anatomopatológico quando possível. Cinquenta pacientes foram incluídos, 25 do sexo feminino e 25 do masculino. A média de idade no atendimento foi de 5.76±4.4 anos e do início do quadro foi 3.52±3.80 anos. A lateralidade foi de 50% do olho direito, 46% do olho esquerdo e 4% bilateral. Os tumores mais frequentes foram hemangioma (20%), má formação venolinfática (18%) e retinoblastoma (12%). Os tumores mais frequentes foram benignos. Não houve diferença estatística nas características demográficas exceto pela idade do diagnóstico e o tempo de sintomas até o atendimento, que foram significativamente menores nos tumores malignos. A concordância entre o diagnóstico clínico e o histopatológico, de acordo com o coeficiente Kappa, foi moderada.
Palavras-chave: Neoplasias orbitátias; Doenças orbitárias; Neoplasias do Nervo Óptico; Exoftalmia; Epidemiologia.
INTRODUCTION
Childhood orbital diseases are a diverse group of illnesses that include both neoplastic and non-neoplastic causes. The epidemiological pattern varies depending on the country, socioeconomic status, and types of ophthalmic care and surveys carried out1,2. Among these diseases, orbital tumors are a major challenge for ophthalmologists because of the difficulty in making an early diagnosis3.
Tumors affect various orbital structures such as the lacrimal gland, adipose and muscle tissue, bones, blood vessels, lymphatic vessels, peripheral nerves, and intraocular structures3. They present some specific features of clinical and radiological examinations that require proper evaluation to define the diagnosis and treatment4.
Although most tumors are benign, some are associated with a significant increase in morbidity and mortality3,5. The lesions can lead to aesthetic problems, reduced or even loss of visual acuity, altered eye mobility, and, eventually, life-threatening conditions1,6.
Epidemiological studies show a frequency of 8%-18% of malignant orbital tumors in children and adolescents. A study conducted in Ethiopia in a tertiary hospital showed a frequency of 7.1% of pediatric ophthalmology consultations, with retinoblastoma and rhabdomyosarcoma being the most prevalent tumors2. In the United States and Western Europe, the majority of malignant tumors are primary tumors such as rhabdomyosarcoma, while in India, most are secondary tumors1.
Proper assessment of tumor prevalence is essential for planning and preparing preventive, diagnostic, and curative measures for health services2. This study aimed to evaluate the epidemiological profile of ocular orbital tumors in the pediatric population, their signs and symptoms, and the agreement between the clinical and histological diagnoses in a Brazilian tertiary ophthalmology department.
METHODS
The study was a retrospective population-based descriptive analysis based on the evaluation of medical records and histological results of childhood ocular orbital tumors. The period analyzed was from July 2017 to July 2022, and we used data from the electronic medical records of the ophthalmology department of the Santa Casa de São Paulo Hospital, a tertiary-level public care institution.
The inclusion criteria were children aged up to 14 years old who attended the ocular orbit department at Santa Casa de São Paulo with a diagnosis or suspicion of intraocular and/or orbital tumor and who had an electronic medical record. The medical records were used to obtain demographic information such as gender, age, clinical presentation, and diagnosis.
Patients without a record in the department's electronic medical records and cases without a defined diagnosis were excluded. Information from the first diagnosis was taken into account for patients with bilateral or relapsing disease.
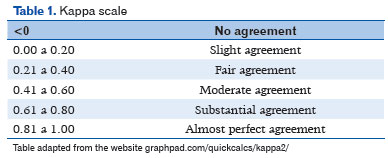
The data were collected by a single researcher and the information obtained was transferred to an Excel spreadsheet for statistical analysis, which involved determining means and standard deviations, as well as percentages. Fisher's exact and Student's t-tests were used to compare some variables considering p<0.05 to be statistically significant. The Kappa coefficient was used to assess the agreement between the clinical and histopathological diagnoses (Table 1).
RESULTS
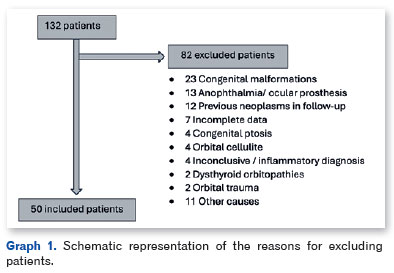
In the selected period from July 2017 to July 2022, a total of 132 patients aged up to 14 years old attended the ocular orbit department for evaluation, of which 50 (37.8%) had ocular orbital tumors. The reasons for excluding the other patients are shown in Graph 1.
Among the patients, 50% were male and 50% female, with no statistical difference even when the groups of benign and malignant tumors were evaluated separately. Laterality was 50% in the right eye, 46% in the left eye, and 4% bilateral (Table 2).
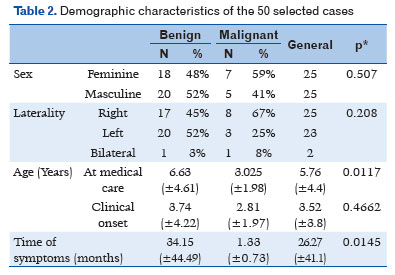
The mean age at admission was 5.76±4.4 years, and the mean age at disease onset was 3.52±3.80 years. There was a statistically significant difference in age at admission between benign (6.63 ± 4.61 years) and malignant (3.02 ± 1.98 years) tumors, with p=0.0117. In addition, there was a statistically significant difference in the time from symptom onset to seeking medical attention between benign (34.15 ± 44.49 months) and malignant (1.33 ± 0.73 months) tumors, with p=0.0145 (Table 2).
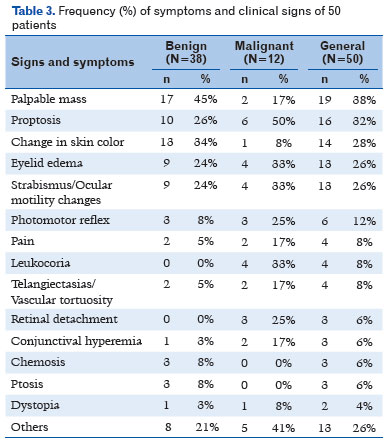
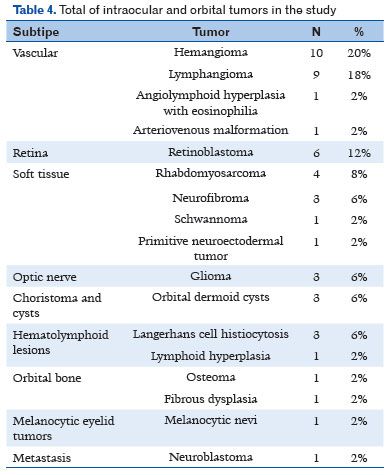
The most common signs and symptoms were tumor mass (38%), proptosis (32%), and changes in skin color (28%), including hyperemia and violaceous lesions (Table 3). Most tumors were vasculogenic, with 20% being hemangiomas, 18% venolymphatic malformations, 12% retinoblastoma, and 8% rhabdomyosarcoma (Table 4).
Among the patients with a suspected or diagnosed tumor, 28 underwent incisional or excisional biopsy for histopathological analysis. The agreement between the clinical and histopathological diagnoses was moderate, with a Kappa coefficient of 0.47 (95% confidence interval: 0.194–0.762).
DISCUSSION
Most studies that analyze the frequency of occurrence of ocular orbital tumors are limited to the adult population, and, therefore, we found few studies on tumors in children, especially in the Brazilian population. In addition to the lack of data that may compromise the organization of the health system on all levels of care, there is not enough emphasis on teaching about these conditions, which create difficulties in diagnosis and access to treatment and social support2,7.
This study was conducted in a tertiary public health institution. In Brazil, public health is managed under the Unified Health System (SUS), which is divided according to its complexity of care into primary, secondary, and tertiary levels and by health regions with their respective reference centers. As such, it is biased because tertiary services are a reference for highly complex cases that could not be solved at lower levels and do not reflect the general population7.
The most common signs and symptoms observed in the clinical evaluation of these patients were palpable tumor mass, proptosis, altered skin color, eyelid edema, and altered extrinsic ocular mobility. Similar findings were obtained in Saudi Arabia, with a higher prevalence of proptosis/dystopia, edema, restricted motility, and diplopia. In Ethiopia, a study with a 77.2% frequency of retinoblastoma indicated that proptosis and leukocoria were the most common signs. This description of symptoms was scarce in other studies, which made comparisons difficult1,4.
In line with the literature, we obtained a higher frequency of benign ocular orbital tumors, which were mainly vasculogenic tumors: hemangioma and venolymphatic malformation. Infantile hemangiomas are hamartomas of the endothelial cells of blood capillaries and are considered the most common orbital vascular tumors in childhood. Venolymphatic malformation, however, is slightly less common and is part of a spectrum of complex congenital lesions of the orbit, with lymphatic and vascular involvement5,8,9.
In a study conducted in Saudi Arabia with patients aged up to 18 years old, 107 patients were submitted to orbital biopsy over a 13-year period, 43% of which were cystic lesions and 15% were vasculogenic tumors. Other studies also show a high prevalence of cystic lesions, described by many as the most common orbital lesion in the pediatric population. These lesions can be congenital or acquired and are mostly benign1,8,10,11.
An 18-year retrospective study conducted in China with 719 cases of tumor or tumor-like lesions in patients up to 20 years old found that 92.1% were benign tumors, with nevus, dermoid/epidermoid cyst, and epithelioma being the most common. Many types of benign lesions were not frequent in the present study, especially cystic lesions, which may be explained by the fact that these types of conditions are resolved at the primary and secondary levels of care1,12.
In this Chinese study, the mean age at diagnosis was 12.91±4.86 years, which is much higher than that reported herein (5.76 ± 4.4 years). This difference is even greater if we look at the mean age at diagnosis of malignant cases, which in the Chinese study was 12.96±4.65 years and in the present study was 3.02±1.98 years. This is a relevant point considering the potential increase in morbidity and mortality associated with late diagnosis of childhood tumors. The data obtained shows that these patients probably had easier access to this healthcare service than those in other studies in the literature, in which the mean age was 61,3-5,12.
In Ethiopia, a study evaluated all ocular diseases in the population under 16 years old in a tertiary hospital over 1 year and identified 88 ocular orbital tumors: 66 retinoblastomas, 10 rhabdomyosarcomas, 6 hemangiomas, and 6 gliomas. The dermoid cyst fell into the congenital abnormality category, with 18 cases detected. Unlike the other studies, except for a study conducted in India, there was a predominance of malignant tumors2,3. The most common malignant tumor in the pediatric populations of the analyzed studies was retinoblastoma1,2,4,12-14.
Many lesions in our series of cases were less frequent tumors and even rare tumors, such as angiolymphoid hyperplasia with eosinophilia, neuroendocrine tumors, and fibrous dysplasia. Many of them have not been observed in other epidemiological studies. This may be due to how the SUS works, i.e., its units are referral centers for more complex cases.
After clinical evaluation and imaging exams, our diagnostic hypothesis agreed moderately with the histopathological examination. All cases of clinically suspected malignancy were confirmed through histopathology; however, two cases were considered benign, and two cases with indeterminate diagnoses were confirmed as malignant tumors after biopsy. Given that access to resources and surgical procedures in the public sector is often difficult, an assessment by an experienced professional is essential; however, it is worth emphasizing the importance of complementary histopathological tests in potentially severe and malignant cases5,15.
The limitations of this study included the retrospective nature of the analysis and the small sample size, which was due to the low occurrence of these diseases. Furthermore, the lack of standardization between the published demographic studies regarding the age of the study population, type of ophthalmic care, and inclusion criteria makes it difficult to compare studies. Conducting a prospective study with a multicenter evaluation over a longer period would help establish the pattern of presentation of childhood ocular orbital tumors in Brazil.
There was no statistical difference in gender distribution and laterality or age at disease onset, but there was a difference in age at diagnosis and time from symptoms to treatment, which were significantly lower in malignant tumors. The most frequent patients' symptoms were palpable tumor mass, proptosis, and altered skin color. Benign tumors were the most common lesions, especially tumors of vascular origin (hemangioma and venolymphatic malformation). There was moderate agreement between the clinical and histopathological diagnoses.
REFERENCES
1. Alkatan HM, Al Marek F, Elkhamary S. Demographics of pediatric orbital lesions: A tertiary eye center experience in Saudi Arabia. J Epidemiol Glob Health. 2019;9(1):3-10.
2. Kidane YT, Teshome AW. Eye disorders spectrum: A tertiary hospital pediatric ophthalmology clinic based in Ethiopia. BMC Ophthalmol. 2022;22(1):120.
3. Modi PJ, Shah NA, Bhalodia JN, Gonsai RN. Orbital tumors in children: A descriptive study at tertiary care centre. Natl J Med Res. 2013;3(4):362-366.
4. Issa SA, Nour AS, Neknek GA. Pediatric oculo-orbital tumor characteristics, imaging and histopathology agreement in a tertiary level teaching hospital, Ethiopia. Ethiop J Health Sci. 2022;32(2):313-320.
5. Rao AA, Naheedy JH, Chen JY, Robbins SL, Ramkumar HL. A clinical update and radiologic review of pediatric orbital and ocular tumors. J Oncol. 2013;2013:975908.
6. Colafati GS, Piccirilli E, Marrazzo A, Carboni A, Diociaiuti A, El Hachem M, et al. Vascular lesions of the pediatric orbit: A radiological walkthrough. Front Pediatr. 2022 Nov 30;10:734286.
7. Instituto Nacional de Câncer José Alencar Gomes da Silva. Diagnóstico precoce do câncer na criança e no adolescente. 2. Ed. rev. ampl., 3. reimp. Rio de Janeiro: Inca, 2014. Disponível em: https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/diagnostico-precoce-na-crianca-e-no-adolescente.pdf. Acesso em: 26/09/2023.
8. Angotti H Neto, Cunha LP, Gasparin F, Santo RM, Monteiro MLR. Lesões expansivas da órbita: distribuição de casos com estudo histopatológico em 11 anos no Hospital das Clínicas da FMUSP. Arq Bras Oftalmol. 2008;71(6):809-12.
9. Gontijo B, Silva CMR, Pereira LB. Hemangioma da infância. An Bras Dermatol. 2003;78(6):651-73.
10. Castillo BV Jr, Kaufman L. Pediatric tumors of the eye and orbit. Pediatr Clin North Am. 2003;50(1):149-72.
11. Bonavolontà G, Strianese D, Grassi P, Comune C, Tranfa F, Uccello G, et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthalmic Plast Reconstr Surg. 2013;29(2):79-86.
12. Dai XZ, Wang LY, Shan Y, Qian J, Xue K, Ye J. Clinicopathological analysis of 719 pediatric and adolescents' ocular tumors and tumor-like lesions: a retrospective study from 2000 to 2018 in China. Int J Ophthalmol. 2020;13(12):1961-1967.
13. Skalet AH, Gombos DS, Gallie BL, Kim JW, Shields CL, Marr BP, et al. Screening children at risk for retinoblastoma: Consensus report from the American Association of Ophthalmic Oncologists and Pathologists. Ophthalmology. 2018;125(3):453-458.
14. Suleiman DE, Iliyasu Y, Ahmed SA, Liman AA. Histopathologic spectrum of paediatric eye and ocular adnexal tumours: A 10-year review from a referral centre in Nigeria. Niger J Clin Pract. 2020;23(5):654-659.
15. Shields JA, Bakewell B, Augsburger JJ, Donoso LA, Bernardino V. Space-occupying orbital masses in children. A review of 250 consecutive biopsies. Ophthalmology. 1986;93(3):379-84.
AUTHORS INFORMATIONS |
|
 |
» Juliana Ishii Iguma https://orcid.org/0000-0002-8745-6582 https://lattes.cnpq.br/9614009693321638 |
 |
» Camila Ishii Iguma https://orcid.org/0000-0002-1193-9262 https://lattes.cnpq.br/0934903889666313 |
 |
» José Vital Filho https://lattes.cnpq.br/2460766132336890 |
 |
» Ivana Lopes Romero Kusabara https://orcid.org/0009-0006-8697-7112 https://lattes.cnpq.br/1229526964122072 |
Funding: No specific financial support was available for this study.
Project number and institution responsible for the opinion of the Research Ethics Committee: CAAE: 64717822.0.0000.5479 pela Santa Casa de Misericórdia de São Paulo (SCMSP).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
April 2, 2024.
Accepted on:
July 4, 2024.