Danielle Ribeiro Brega Weiss; Lara de Cássia Dutra Teixeira; Marta Halfeld Ferrari Alves Lacordia
DOI: 10.17545/eOftalmo/2024.0010
ABSTRACT
Divergent strabismus associated with hypotropia in high myopia is rare, with few reports in the literature. Its pathogenesis is uncertain and surgical treatment is not standardized. We describe the case of an 18-year-old patient with myopic anisometropia with exotropia associated with unilateral hypotropia who underwent surgery with a good postoperative outcome.
Keywords: Exotropia; Pathologic myopia; Strabismus; Heterotropia; Secondary exotropia.
RESUMO
A apresentação de estrabismo divergente associado à hipotropia na alta miopia é rara, com poucos relatos descritos na literatura. Possui patogênese incerta e o tratamento cirúrgico não está padronizado. Descrevemos um caso de exotropia associado a hipotropia unilateral em paciente de 18 anos com anisometropia miópica que foi submetida à correção cirúrgica com bom resultado no pós-operatório.
PALAVRAS-CHAVE: Exotropia; Miopia patológica; Estrabismo; Heterotropia; Exotropia secundária.
ABSTRACT
Divergent strabismus associated with hypotropia in high myopia is rare, with few reports in the literature. Its pathogenesis is uncertain and surgical treatment is not standardized. We describe the case of an 18-year-old patient with myopic anisometropia with exotropia associated with unilateral hypotropia who underwent surgery with a good postoperative outcome.
Palavras-chave: Exotropia; Pathologic myopia; Strabismus; Heterotropia; Secondary exotropia.
INTRODUCTION
Studies to better understand the etiopathogenesis of strabismus in high myopia are conducted. The combination of esotropia and hypotropia, also known as Heavy Eye Syndrome (HES), is caused by superotemporal prolapse of the eye due to axial distension. Additionally, the enlargement of the ocular globe leads to instability of the orbital tissues, which leads to alterations of the intermuscular pulleys. Together, these factors cause the displacement of the superior rectus muscle (SR) and lateral rectus muscle (LR). The association of exotropia-hypotropia with high myopia has only been described a few cases in the literature1-4.
We report a case of myopic anisometropia associated with exotropia-hypotropia and review the literature on high myopia-associated strabismus. This study was approved by the Ethics Committee of the University Hospital of the Federal University of Juiz de Fora.
CASE REPORT
An 18-year-old female presented with mild strabismus since birth, which has worsened in recent years (my right eye is drooping). She has been wearing glasses since childhood and has undergone occlusion therapy but no surgery. She has story of being born premature. Ophthalmological examination showed: visual acuity in the right eye (OD): -17.50 sph counting finger at 2 meters and in the left eye (OS): -2.50 = -0.50 at 30º 1.0; biomicroscopy of both eyes (OU) was normal; intraocular pressure was 12 mmHg OU (18:30 h); examination of ocular motility-Krimsky: exotropia of 35 prismatic diopters (PD) and OD hypotropia of 12 PD. She had excessive elevation in adduction of the OD (+1.0), limited elevation of the OD (-2.0), and excessive lowering of the OD (+1.5) (Figure 1). The excessive versions were graded on a subjective scale from 0 to +4, with 0 indicating no excess motility and +4 indicating maximum motility of the eye beyond the horizontal or vertical midline. Version limitation was also graded on a scale of 0 to -4. Ophthalmoscopy showed a halo of peripheral chorioretinal atrophy in the OD and increased excavation in the OS; in the macula there were areas of retinal pigment epithelium (RPE) atrophy in the OD. Diffuse RPE rarefaction in OU, an area of RPE hyperplasia in the OD, a hole in the superior nasal retinal quadrant of the OD, lattice peripheral retinal degeneration, superior and inferior lattice degeneration in the OU, extensive lattice peripheral retinal degeneration in the OD, nasal and temporal whiteness without pressure in the OD. Photocoagulation was performed for lesions prone to rupture.

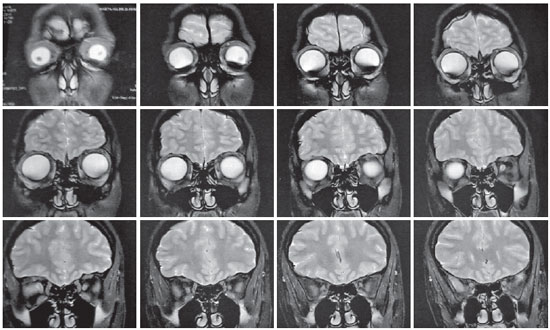
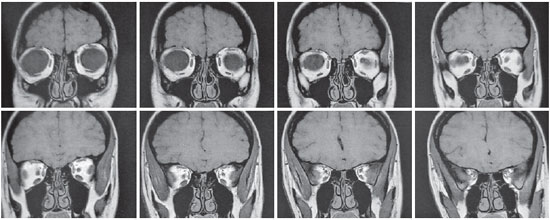
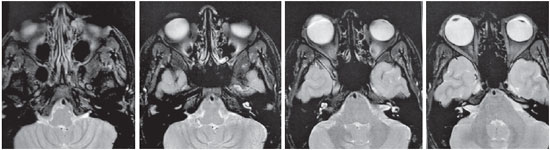
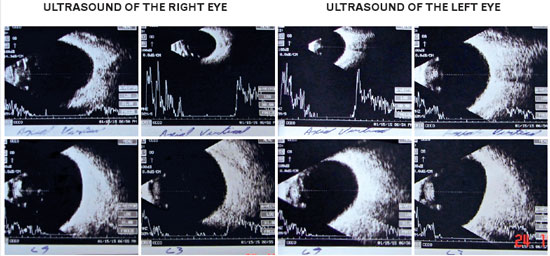
Magnetic resonance imaging (MRI) of the orbits revealed an increase in the ocular globes, which was more marked in the anteroposterior diameter of the OD. The signal and size of the extraocular muscles (EOM) were normal (Figures 2-4). Ocular ultrasound showed an increased and asymmetrical axial length, with the OD (32 mm) being larger than the OD (26 mm) (Figure 5), as well as an increase and bulging of the posterior curvature of the OD, which suggested posterior pole staphyloma.
Surgery was performed to correct strabismus: 8 mm LR recession, 5.5 mm resection of the medial rectus muscle (MR) on the right side, and recession of the inferior oblique muscle (IO) on the left side.
The postoperative Krimsky test results showed orthotropia, limited elevation in adduction (-1.0), and limited elevation (-2.0) of the OS due to recession of the IO of the OS (Figure 6).

DISCUSSION
Strabismus in high myopia is an acquired strabismus due to a high degree of myopia, usually greater than 25 spherical diopters, in eyes with an increased anteroposterior diameter5. It is characterized by restricted abduction and elevation, with esotropia and hypotropia of the affected eye6. In advanced cases, the compromised eye is extremely fixed in the convergence position and hypotropia, and no movement in any other direction. This extreme condition is referred to as convergent strabismus fixus, myopic strabismus fixus or HES. It can be unilateral or bilateral7. HES was first described in 1966 by Bagshaw, who presented a case report of two patients with vertical and horizontal deviations and high myopia, which he then called heavy eye phenomenon8.
Strabismus associated with high myopia does not always take the form of a fixed deviation. In some cases, small-angle esotropia occurs with slight restriction of abduction and the eye may move beyond the midline. Convergent deviation does not always occur, and exotropia associated with hypotropia is a rare manifestation, with only a few reports2,9-13.
Theories regarding the etiology of acquired esotropia-hypotropia in high myopia have been proposed. This progressive deviation has been described as resulting from myositis and consequent fibrosis of the LR as well as compression of the LR by the orbital walls due to the enlargement of the eye7.
Yokoyama et al. postulated that myopic stretching of the eye leads to prolapse of the posterior supratemporal quadrant outward of the muscle cone, between the SR and LR. Therefore, the SR and the LR are medially and inferiorly displaced, respectively. Inferior displacement of the LR pulley increases infraduction, whereas medial displacement of the SR pulley increases adduction force, leading to limited supraduction and abduction, respectively4,5.
Rutar and Demer suggested that degeneration of ligament band between LR and SR with advancing age contributes to inferior displacement of the LR. Similar changes or instability in the EOM pulleys due to the disproportionate volume between the orbit and the ocular globe and well as the consequent fragility of the orbital tissue may contribute to the pathogenesis of this strabismus3.
This theory has been reinforced by imaging examinations, such as MRI, allowing the study of extraocular muscles. Several studies have shown that this strabismus is a consequence of the altered path of the EOM associated with the elongation of the eye in extreme axial myopia2,7,14.
Monga et al. reported the largest series of exotropia and hypotropia in 15 patients with progressive strabismus, high myopia, and anisometropic amblyopia. Hypotropia greater than 5 PD was seen in 80% of cases. The average axial length of the deviated eye was 29.43 + 1.51 mm, which is less than that observed in the esotropia-hypotropia complex. The average divergent deviation was 37 + 9 PD and hypotropia was 13 + 6 PD. Elevation deficiency was observed in six patients (40%). However, the position of the EOM on imaging examination was normal2. This provides data concordant with the clinical case presented herein and confirms the results of previous studies.
Ahmed et al. reported a pattern of unilateral high myopia with moderate-angle exotropia, with limited elevation and profound amblyopia of the deviated eye. Perioperatively, inferior displacement of the LR was observed, as occurs in HES. A temporal displacement of the SR, rather than the nasal displacement described in the HES, was initially assumed. However, exploration of the SR in all surgeries revealed no such displacement, consistent with the findings of MRI prior to surgery10.
The etiology of acquired exotropia-hypotropia in high myopia is unclear. The term “exotropic heavy eye” has been proposed to describe this pattern of deviation in myopic patients; however, this term should not suggest the same pathogenesis as that of HES. One explanation for the exotropic heavy eye is that an amblyopic eye tends to enter a state of hypotropia and exotropia, which is the resting state for the eye. Long-standing hypotropia and exotropia resulted in some restriction in both elevation and adduction10.
Various surgical procedures have been proposed to treat HES. The choice of technique depends largely on the preference and experience of the surgeon11. The traditional recess-resect technique is associated with esotropia recurrence because it does not address the correction of the altered muscle path15.
In 2002, Yamada et al. proposed one of the first techniques to address the altered muscle pathway in HES. Yamada's technique involves hemitransposition of the SR and LR, often combined with MR recoil recession. The SR and LR are partially divided in half by approximately 15 mm from their origin. The temporal half of the SR and the superior half of the LR are attached to the sclera 7 mm posterior to the limbus16.
In 2004, Larsen and Gole used the Jensen procedure, partially, in a case of myopic strabismus fixus. The procedure divided the SR and LR in half, from the insertion to the equator, and a nonabsorbable suture 12 to 15 mm from the limbus joined the lateral half of the SR and the upper half of the LR17.
In 2010, Yamaguchi et al. proposed the Yokoyama technique, which consists in creating a union and approximation between the bellies of the SR and the LR and placing a nonabsorbable 5-0 polyester suture 15 mm behind the muscle insertions. This approximation results in a sling that supports the elongated eye, pushing it back into the muscle cone. It can be associated with MR recession in cases where esotropia is not completely corrected or there is MR contracture6. A review by Su et al. determined that the Yokoyama technique associated with MR recession is more effective in patients with esotropia between 12 and 85 PD18.
Myopexy with a silicone band is another technique used to treat HES. A scleral tunnel is created 14-16 mm from the limbus between the SR and LR and then a silicone band is passed under the LR, then through the scleral tunnel, and then under the SR, thus joining the bellies of these muscles19.
In 2022, Mendonça et al. proposed a new technique called interlacing for the treatment of HES. It consists of detaching and interlacing the upper half of the LR to the divided SR at its insertion and reinserting this LR band to its original insertion20.
Contrary to esotropia-hypotropia complex, the surgical approach for the exotropia-hypotropia complex is not described with a specific and simple procedure. Monga et al., in a large series study, performed retrograde resection with elevation of the muscle insertions in all patients. Additional retraction of the inferior rectus muscle was required for two patients. Tenotomy of the superior oblique was performed in one patient with “A” anisotropy. Another patient required myectomy of the IO. One patient who underwent retrograde MR suffered perioperative temporal displacement of this muscle. Myopexy combining MR and SR was performed in one patient as a reoperation for residual exotropia of 16 PD and hypotropia of 22 PD, with a satisfactory result2,21.
In 2019, Ganesh et al. reported a series of three cases involving exotropia-hypotropia and high myopia. Perioperatively, they observed an inferior deflection in the MR path from its insertion and lateral displacement of the SR insertion by almost one tendon width. No staphyloma was observed between the MR and SR, although thinning of the sclera could be seen. They hypothesized that the limited preoperative elevation of the SR was due to the altered path and insertion of the muscle, which caused more abducting effect than elevating effect, thus explaining the exotropia. They performed recession and resection of the horizontal rectus muscles associated with nasal myopexy in a loop between the SR and MR, 12 mm from their insertions, using nonabsorbable 5-0 polyester. Episcleral sutures were not performed because of scleral thinning in these sites. They obtained satisfactory postoperative results with improvement in elevation in abduction and ocular deviation in all cases22.
In the present case, there were no alterations in the path of the EOMs on the MRI or perioperatively. He had unilateral high myopia, intermediate-angle exotropia (35 PD) and hypotropia of 12 PD, similar to the average deviation found by Monga et al. An 8-mm LR recession and a 5.5-mm MR resection were performed in the OD, as this was the eye affected by high myopia, nonfixation, and amblyopia. Additionally, we opted to perform recession of the IO in the OS because it is a reversible and separable technique that limits the elevation of the OS and thus corrects the vertical deviation. The postoperative result was considered satisfactory, especially by the patient who has been followed up for 7 years since the surgery and has maintained orthotropy.
Most patients with exotropia-hypotropia complex have unilateral high myopia, dense amblyopia, and moderate-angle exotropia, whereas most reported cases of HES have bilateral high myopia and large-angle esotropia2. The pathogenesis of exotropia-hypotropia complex in high myopia is unclear, and surgical management is not standardized, requiring further studies to better understand its pathogenesis.
REFERENCES
1. Demer JL, von Noorden GK. High myopia as an unusual cause of restrictive motility disturbance. Surv Ophthalmol.1989;33(4):281-4.
2. Monga S, Kekunnaya R, Sachdeva V. Exotropia-hypotropia complex in high myopia. J Pediatr Ophthalmol Strabismus.2013;50(6):340-6.
3. Rutar T, Demer JL. “Heavy Eye” syndrome in the absence of high myopia: A connective tissue degeneration in eldery strabismic patients. J AAPOS.2009;13(1):36-44.
4. Tan RJD, Demer JL. Heavy eye syndrome versus sagging eye syndrome in high myopia. J AAPOS. 2015;19(6):500-6.
5. Yokoyama T, Tabuchi H, Ataka S, et al. The mechanism of development in progressive esotropia with high myopia. In: J.T. de Faber (eds) Transactions of the 26th Meeting. Barcelona: European Strabismological Association, Swets&Zeitlinger, 2000, 218-221.
6. Yamaguchi M, Yokoyoma T, Shiraki K. Surgical procedure for correcting globe dislocation in highly myopic strabismus. Am J Ophthalmol.2010;149(2):341-346.e2.
7. Martínez PH, del Valle JMR. Revisión del estrabismo en miopes. Arch Soc Esp Oftalmol. 2017;92(12):585-93.
8. Bagshaw J. The “heavy eye” phenomenon: a preliminary report. Br Orthopt J 1966;75-78.
9. Krzizoh TH, Kaufmann H, Traupe H. Elucidation of restrictive motility in high myopia by magnetic resonance imaging. Arch Ophthalmol.1997;115(8):1019-27.
10. Awadein A, Hassanein DH. Exotropic heavy eye syndrome in unilateral high axial myopia. J AAPOS.2020;24(3):131.e1-131.e6.
11. Hennein L, Robbins SL. Heavy eye syndrome: Myopia-induced strabismus. Surv Ophthalmol. 2021;66(1):138-144.
12. Sharma TK, Grewal JS, MacDonald M. Divergent strabismus fixus-a case report. Eur J Ophthalmol. 2003;13(2):207-8.
13. Maiolo C, Fresina M, Campos EC. Role of magnetic resonance imaging in heavy eye syndrome. Eye (Lond). 2017;31(8):1163-1167.
14. Tanaka A, Ohno-Matsui K, Shimada N, Hayashi K, Shibata Y, Yoshida T, et al. Prevalence of strabismus in patients with pathologic myopia. J Med Dent Sci.2010;57(1):75-82.
15. Ranka MP, Steele MA. Esotropia associated with high myopia. Curr Opin Ophthalmol. 2015;26(5):362-5.
16. Yamada M, Taniguchi S, Muroi T, Satofuka S, Nishina S. Rectus eye muscle paths after surgical correction of convergent strabismus fixus. Am J Ophthalmol. 2002;134(4):630-2.
17. Larsen PC, Gole GA. Partial Jensen's procedure for the treatment of myopic strabismus fixus. J AAPOS. 2004;8(4):393-5.
18. Su Y, Shen Q, Fan X. Loop Myopexy Surgery for Strabismus Associated with High Myopia. J Ophthalmol. 2016:2016:8657036.
19. Siah WF, Guerin MB, Flitcroft I, Fulcher T. Surgical management of heavy eye phenomenon. Orbit. 2010;29(5):259-61.
20. Mendonça TS, Rossetto JD, Correa AB, Plut M. New Surgical Interlacing Technique for Correction of Highly Myopic Strabismus. J Pediatr Ophthalmol Strabismus. 2022;59(1):e1-e6.
21. Kekunnaya R, Chandrasekharan A, Sachdeva V. Management of strabismus in myopes. Middle East Afr Ophthalmol.2015; 22(3):298-306.
22. Ganesh SC, Jayadev NA, Oguego N, Narendran K, Rao SG. Nasal loop myopexy as a primary procedure to correct exotropia hypotropia complex in high myopia. Strabismus. 2019;27(4):223-9.
AUTHORS INFORMATIONS |
|
 |
» Danielle Ribeiro Brega Weiss https://orcid.org/0000-0002-1950-7149 http://lattes.cnpq.br/5107661603504202 |
 |
» Lara de Cássia Dutra Teixeira https://orcid.org/0009-0007-0664-3460 http://buscatextual.cnpq.br/buscatextual/visualizacv.do |
 |
» Marta Halfeld Ferrari Alves Lacordia https://orcid.org/0000-0003-4296-4871 http://lattes.cnpq.br/4777310256357609 |
Funding: No specific financial support was available for this study.
Approved by the following research ethics committee: Hospital Universitário da Universidade Federal de Juiz de Fora - UFJF (CAAE: 49475321.3.0000.5133).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
September 11, 2023.
Accepted on:
February 12, 2024.