Mário Henrique Camargos de Lima1; Alex Roque Rizzi2; Francisco Nepomuceno Neto3; Rosângela Aparecida Simoceli4; Fernando Betty Cresta5; William Camargos de Lima6; Gustavo Victor7; Milton Ruiz Alves8
DOI: 10.17545/e-oftalmo.cbo/2016.65
ABSTRACT
OBJECTIVE: To determine whether there is an association between corneal affection asymmetry in keratoconus and preferred sleeping position.
METHODS: A prospective clinical study was performed. All participants answered a questionnaire to report their preferred sleeping position. Regardless of the decubitus (lateral or ventral), the eye that was positioned inferiorly during sleep was classified as the “dependent eye”, and the eye positioned superiorly was classified as the “non-dependent eye”.
RESULTS: This study indicated greater topographic changes in the dependent eyes of keratoconus carriers; this finding may be associated with the patient’s sleeping position. Regardless of the right or left lateral decubitus positions, greater topographic abnormalities were observed in the corneas of the dependent eye. This finding may be explained by the occurrence of mechanical traumas during sleep and may be secondary to the preferred sleeping position.
CONCLUSION: In the treatment of keratoconus, it is essential to identify and reduce the risk factors associated with disease progression. Considering the fact that humans spend a considerable amount of time sleeping, keratoconus patients may benefit from clarifications on position preferences and sleeping habits.
Keywords: Cornea; Sleep; Keratoconus
RESUMO
OBJETIVO: Verificar se há associação da assimetria do acometimento corneano no ceratocone com a posição preferencial de dormir.
MÉTODOS: Realizou-se estudo clínico prospectivo. Todos os participantes foram submetidos a questionário para avaliação da posição preferencial de dormir. Classificou-se como "olho dependente" o olho posicionado inferiormente durante o sono, independentemente do decúbito (lateral ou ventral), e de "olho não dependente" o olho posicionado superiormente, tanto em decúbito lateral quanto ventral.
RESULTADOS: O presente estudo mostrou maiores alterações topográficas nos "olhos dependentes" de portadores de ceratocone e que podem estar relacionadas com a posição de dormir. Independentemente das posições de decúbito lateral direita ou esquerda observou-se maior alteração topográfica da córnea no "olho dependente" com ceracotone e este achado poderia ser explicado pela ocorrência de traumas mecânicos originados durante o sono e secundários à posição preferencial de dormir.
CONCLUSÃO: É fundamental que na orientação ao paciente com ceratocone sejam identificados e reduzidos os efeitos de fatores de risco associados com a evolução da doença. Considerando-se que passamos grande parte de nossas vidas dormindo, esclarecimentos sobre preferências de posições e cuidados ao dormir poderão ser benéficos para os pacientes portadores de ceratocone.
Palavras-chave: Córnea; Sono; Ceratocone
INTRODUCTION
Keratoconus is a bilateral ecstatic disease that evolves with stroma thinning and progressive protrusion of the cornea, resulting in irregular astigmatism, low vision, and visual distortion secondary to high-order aberrations 1 The disease progresses slowly, and its estimated incidence varies according to the population studied and diagnostic criteria used. Most estimates range from 50 to 230 cases per 100,000 individuals in the general population 1,2.
The etiology of keratoconus has been the subject of numerous studies; it is accepted that genetic predisposition is accompanied by environmental factors 1,2,3. Recently, the non-inflammatory nature of the disease has been questioned3 The act of scratching the eye contributes to the pathogenesis of keratoconus 4.
Due to the viscoelastic characteristics of the cornea, changes in intraocular pressure (IOP) are one of the factors suspected of contributing to the development of corneal ectasias5. Acute events, such as perforation and hydropsy, may also be associated with pressure variations 5.
Variations in IOP variation during changes in sleeping position is a well-established fact in the literature that has been exhaustively analyzed in anesthesiology research. These studies report that increases in IOP may lead to complications involving ocular perfusion in prolonged ventral decubitus 6,7,8,9.
Humans generally spend one-quarter to one-third of their lives asleep, and changes in sleeping position are associated with changes in IOP during sleep. Kim et al. 10 interviewed 692 patients with open-angle glaucoma using a questionnaire that determined the preferred sleeping position and its relation to asymmetrical visual field loss. There are also reports of a higher prevalence of keratoconus in patients with sleep apnea 11.
The present study sought to verify the presence of an association between asymmetry of corneal involvement in keratoconus and preferred sleeping position.
METHODS
A prospective clinical study was approved by the Research Ethics Committee of the Padre Bento Hospital Center in Guarulhos, São Paulo State, Brazil. All subjects signed an informed consent form; when patients were minors, the form was signed by a parent or guardian. The study was performed in the Ophthalmology Department of the Padre Bento Center from January to December 2014.
The study population consisted of 60 individuals over 10 years of age with a topographic diagnosis of keratoconus. The participants included in the study had keratoconus classified according to its topography as grade II (moderate, between 45.00 and 52.00 D), grade III (advanced, between 52.00 and 62.00 D), or grade IV (intense, greater than 62.00 D). Patients with inflammatory and/or infectious ocular conditions and those with a history of ocular surgery were excluded.
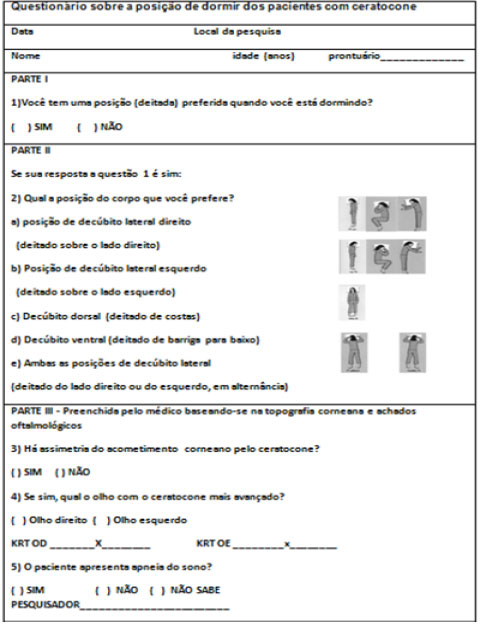
All participants answered the questionnaire proposed by Kim et al. 9 for assessing their preferred sleeping position Figura 1. Regardless of the position (lateral or ventral), the eye that was positioned inferiorly during sleep was classified as the “dependent eye”, and the eye positioned superiorly was classified as the “non-dependent eye”.
Bilateral corneal topography was performed on all participants using the EyeSys® System 2000. Axial and tangential maps were obtained on a 0.50 D scale. Differences greater than 1 D in the mean keratometry values were used to indicate the eye with the greatest involvement (asymmetry). The presence of sleep apnea was also assessed.
The mean values of the keratometric measurements of the eyes with the lowest and the highest involvement were compared using a paired t-test (quantitative variables). The influence of right lateral, left lateral, and ventral decubitus, as well as of the preferred sleeping position on the onset of asymmetry in the dependent and non-dependent eyes, were assessed using the chi-squared test (qualitative variables). All statistical analyses were performed using SPSS software, version 18.0 (SPSS Inc., Chicago, IL, USA). A p-value < 0.05 was adopted as the level of statistical significance.
RESULTS
The study population consisted of 60 individuals (58% female and 42% male). All of the participants were found to have a preferred sleeping position. Lateral decubitus was preferred by 67% of the participants. Topographic asymmetries were observed between the eyes in 93.3% of the participants (Table 1).
The keratometric means of the eyes with the lowest involvement was significantly lower than those of the eyes with the greatest involvement (p-value < 0.001; Table 2).
There was a significant association between lateral decubitus and the most affected eye, which was also classified as the dependent eye (p = 0.014; Table 3).
Graph 1 shows a higher involvement of the dependent eye in the right or left lateral decubitus position.
There was no significant association between ventral and lateral decubitus positions and greater involvement of the dependent eye (p = 0.452; Table 4).
The comparison between lateral decubitus, regardless of the decubitus side, showed a consistent association with higher involvement of the dependent eye (p = 0.005; Table 5).
Chart 2 illustrates the greater involvement of the dependent eye in the right-side and left-side sleeping position.
In the study sample, no patient presented sleep apnea as comorbidity.
DISCUSSION
The presence of microtraumas is a determinant factor for the evolution of keratoconus. Pruritus (eye allergy) and eye scratching have been consistently associated with disease progression 12. Certain sleeping positions lead to changes in IOP 6 and sleeping position has been found to be associated with asymmetric visual field loss in patients with primary open-angle glaucoma 9.
The present study showed greater topographic changes in the dependent eyes with keratoconus; these changes may be associated with the patient’s sleeping position. In the right and left lateral decubitus positions, greater corneal deformation was observed in the dependent eye with keratoconus; this finding could be a response to mechanical traumas originating during sleep and secondary to the preferred sleeping position.
In the treatment of keratoconus, it is paramount to identify and reduce the risk factors associated with disease progression. The recommendation to avoid scratching the eyes has been widely publicized and is already included in the routine medical recommendations for these patients.4 However, the present study raises a new risk factor for the evolution of keratoconus. Considering the fact that humans spend a considerable amount of time sleeping, clarifications on position preferences and sleeping habits may be beneficial for patients with keratoconus. The creation of devices to be used by these patients during sleep would be welcomed if they can minimize the risk of microtrauma to the eye during sleep.
Prospective clinical studies with follow-up on keratoconus patients are necessary to reinforce the validity of the present findings.
REFERENCES
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998:42(4):297-319. http://dx.doi.org/10.1016/S0039-6257(97)00119-7
2. Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: current scenario. Br J Ophthalmol. 2011:95(8):1044-50. http://dx.doi.org/10.1136/bjo.2010.185868
3. Sugar J, Macsai MS. What causes keratoconus? Cornea. 2012:31:716-9. http://dx.doi.org/10.1097/ICO.0b013e31823f8c72
4. Korb DR, Leahy CD, Greiner JV. Prevalence and characteristics of eye rubbing for keratoconic and non-keratoconic subjects. Invest Ophthalmol Vis Sci.1991;32 Suppl:884
5. McMonnies CW. The possible significance of the baropathic nature of keratectasias. Clin Exp Optom. 2013; 96:197-200. https://doi.org/10.1111/j.1444-0938.2012.00726.x
6. Walick KS, Kragh JE Jr, Ward JA, Crawford JJ. Changes in intraocular pressure due to surgical positioning studying potential risk for postoperative vision loss. Spin. 2007;32:2591-5
7. Abraham M, Sakhuja N, Sinha S, Rastogi S. Unilateral visual loss after cervical spine surgery. J Neurosurg Anesthesiol. 2003;15:319-22. http://dx.doi.org/10.1097/00008506-200310000-0000
8. Lee L, Lam A. Unilateral blindness after prone lumbar spine surgery. Anesthesiology. 2001;95:793-5. Disponível em: http://anesthesiology.pubs.asahq.org/article.aspx?articleid=1944802
9. Ozcan MS, Praetel C, Bhatti MT, Gravenstein N, Mahla ME, Seubert CN. The effect of body inclination during prone positioning on intraocular pressure in awake volunteers: a comparison of two operating tables. Anesth Analg. 2004;99:1152-8. http://dx.doi.org/10.1213/01.ANE.0000130851.37039.50
10. Kim KN, Jeoung JW, Park KH, Kim DM, Ritch R. Relationship between preferred sleeping position and asymmetric visual-field loss in open-angle glaucoma patients. Am J Ophthalmol. 2014;157(3):739-45. http://dx.doi.org/10.10167j.ajo.2013.12.016
11. Gupta PK, Stinnett SS, Carlson AN. Prevalence of sleep apnea in patients with keratoconus. Cornea. 2012;31:595-9. http://dx.doi.org/10.1097/ICO.0b013e31823f8acd
12. McMonnies CW. Mechanisms of rubbing-related corneal trauma in keratoconus. Cornea. 2009;28:607-15. http://dx.doi.org/10.1097/ICQ.0b013e318198384f




Funding source: None
Conflicts of interest: None
Received on:
October 24, 2016.
Accepted on:
November 24, 2016.