Carolina Zuccolotto Pereira1; Bárbara Palma Saccon1; Jéssica Queiroz Soares1; Dayane Cristine Issaho1,2
DOI: 10.17545/eOftalmo/2023.0047
ABSTRACT
The present study reports the case of a 36-year-old male patient with incomitant strabismus and anomalous head posture with depressed chin to relieve symptoms of diplopia. He was submitted to a combined surgical approach (recession-resection) of the left inferior rectus muscle. The purpose of this surgical technique is to correct the deviation in its most incomitant position, with no damage to ocular alignment in the primary gaze position. It has shown to a safe alternative for cases of incomitant horizontal and vertical strabismus, offering good surgical outcomes.
Keywords: Incomitant strabismus; Recession-resection; Diplopia; Case report.
RESUMO
O presente estudo relata o caso de um paciente, masculino, 36 anos, com estrabismo incomitante e posição viciosa de cabeça com mento deprimido para aliviar sintoma de diplopia. Paciente foi submetido à cirurgia combinada (recuo-ressecção) do músculo reto inferior esquerdo. O objetivo desta técnica cirúrgica é a correção do desvio em sua posição de maior incomitância, sem prejudicar o alinhamento ocular na posição primária do olhar. Atualmente vem se concretizando como uma alternativa segura para casos de estrabismo incomitante horizontal e vertical, oferecendo um bom desfecho cirúrgico.
Palavras-chave: Estrabismo incomitante; Recuo-ressecção; Diplopia; Eelato de caso.
INTRODUCTION
Patients with incomitant strabismus may have diplopia only in specific gaze positions. A subset of these patients may present a unique clinical situation, wherein the patient is asymptomatic or free of diplopia in the primary position, but has diplopia in functionally important secondary gaze positions, such as infraversion (for reading) or lateroversion (for driving)1.
The main causes of uncommon horizontal deviations include muscle paresis, ocular restrictions, dissociated horizontal divergence, high accommodative convergence/accommodation (AC/A) ratio, or previous surgery2. Although a few surgical techniques have been proposed to correct this, the results have been unsatisfactory, showing the ipsilateral hypocorrection of the affected muscle and hypercorrection in the contralateral field3.
Generally, these patients undergo Faden surgery (posterior fixation suture surgery), which was proposed by Cuppers in 1976 and involves fixating the extraocular muscle onto the sclera posterior to the equator without detaching the muscle from the sclera4,5.
Faden surgery reduces the maximum rotation of the eye, creating a new insertion for the rotational action of the muscle, with minimal to no influence on positions not controlled by this muscle5.
In 1994, Scott described a new technique in which the effect of posterior fixation is created without sutures. In this technique, a portion of the muscle is resected and the same muscle is retracted. This recession must be greater than or equal to the resection to produce a selective reduction in muscle function in its field of action6. This study reported the case of a man with incomitant strabismus who underwent the combined surgical approach (resection-recession) of the same extraocular muscle as proposed by Scott.
CASE REPORT
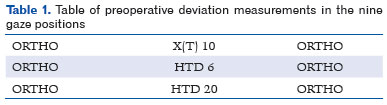
A 36-year-old man complained that 4 months prior he started experiencing diplopia when looking down. On ophthalmic examination, the corrected visual acuity (VA) was 20/20 in both the eyes (OU) (right eye [OD]: +1.00 -5.00 165º and left eye [OS]: +0.25 -1.75 35º). His head was abnormal positioned with a depressed chin to relieve the diplopia symptom. Biomicroscopy and fundus examination revealed no alterations. The extrinsic ocular motility examination showed slight hypofunction (1-/4-) of the right inferior rectus and right superior oblique muscles in infraversion. The alternate prism cover examination with correction is described in Table 1.
The neurological investigation showed no changes. Magnetic resonance imaging of the skull and orbits revealed no anatomical changes in the extraocular muscles. A 6-mm recession and a 3-mm resection of the left inferior rectus muscle was decided.
On the first postoperative day, the patient exhibited hypertropia of 6 prism diopters in OD in the infraversion position and was orthophoric in the other positions. After 30 days of the surgery, the patient maintained a corrected VA of 20/20 OU and was orthophoric in all the nine gaze positions in the alternate prism cover examination with correction. The patient remained stable on follow-up at 4 months and was satisfied with the surgical result.
DISCUSSION
Surgery using the technique of resection and recession of the same muscle was first proposed by Scott and has become a safe alternative for cases of horizontal and vertical incomitant strabismus. It aims to weaken the muscle in its field of action without significantly altering the primary gaze position6.
Scott initially proposed a large resection, but Bock et al. proposed reducing the resected portion of the muscle due to the impossibility of predicting long-term effects7.
Bock et al. concluded that this is a safe procedure for incomitant strabismus involving the lateral rectus, making it possible to use adjustable sutures to eliminate the problem of posterior fixation. For other muscles, however, the authors concluded that they lacked experience to evaluate the effectiveness of the procedure7.
The patient who underwent this procedure had difficulty reading, as diplopia occurred only in infraversion, with no complaints in other positions. The deviation was significantly reduced and the result after 4 months was satisfactory for both the surgeon and the patient.
REFERENCES
1. Thacker NM, Velez FG, Rosenbaum AL. Combined adjustable rectus muscle resection--recession for incomitant strabismus. J AAPOS. 2005 Apr;9(2):137-40.
2. Souza-Dias C, Prieto-Diaz J. Cirurgia do estrabismo. In: Prieto-Diaz J, Souza-Dias C. Estrabismo. 4a ed. São Paulo: Santos; 2002. p.475-7.
3. Ribeiro GB, Almeida HC, dos Santos EM. New surgical aproach in the treatment of incomitant strabismus: case report. Arq Bras Oftalmol. 2006;69(4):585-8.
4. Cuppers C. The so-called fadenoperation: surgical corrections by small-defined changes of the arc of contact. In: Fells P, editor. The 2nd congress of the International Strabismology Association. Marseilles (France): Diffusion Generale de Librairie; 1976. p. 395.
5. von Noorden GK. Binocular vision and ocular motility: theory and management of strabismus. St Louis (MO): Mosby-Year Book; 1978.
6. Scott AB. Posterior fixation: adjustable and without posterior sutures. In: Lennerstrand G, editor. Update on strabismus and pediatric ophthalmology: Proceedings of the june 1994 Joint ISA and AAPO&S Meeting. Vancouver, Canada. Boca Raton (FL): CRC; 1995. p.399.
7. Bock CJ Jr, Buckley EG, Freedman SF. Combined resection and recession of a single rectus muscle for the treatment of incomitant strabismus. J AAPOS. 1999;3(5):263-8.
| AUTHORS INFORMATION |
|
 |
» Carolina Zuccolotto Pereira https://orcid.org/0000-0003-3675-4691 http://lattes.cnpq.br/1322624712208002 |
 |
» Bárbara Palma Saccon https://orcid.org/0000-0002-3922-4939 http://lattes.cnpq.br/2514218750645064 |
 |
» Jéssica Queiroz Soares https://orcid.org/0000-0003-2972-0557 http://lattes.cnpq.br/5911891259820431 |
 |
» Dayane Cristine Issaho https://orcid.org/0000-0001-8572-5980 http://lattes.cnpq.br/7586438822727319 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
January 10, 2023.
Accepted on:
September 24, 2023.