Amanda Geara1; Vanessa Nicola Labrea2; Eric Vieira3; Liana Grupenmacher Iankilevich4; Luiz Fernando Interaminense Garbers4
DOI: 10.17545/eOftalmo/2023.0046
ABSTRACT
The Weill-Marchesani syndrome consists of a rare systemic congenital pathology that can present an autosomal recessive or dominant pattern of inheritance. It affects the connective tissue of different organs, including the eyes, leading to changes in anatomical patterns and subsequent complications. This article reports the case of a 24-year-old female patient with intermittent episodes of pupillary block in both eyes. The diagnosis of Weill-Marchesani syndrome is described, as well as the clinical-surgical management of the disease, whose outcome involved iridotomy and cataract surgery. The importance of knowledge of the course of the disease by the ophthalmologist is highlighted, as well as the performance of an early diagnosis, given that its complications can be of high ophthalmological severity if not properly managed.
Keywords: Weill-Marchesani; Glaucoma; Microspherophakia; Ectopia Lentis.
RESUMO
A síndrome de Weill-Marchesani consiste em uma patologia congênita sistêmica rara que pode apresentar um padrão de herança autossômica recessiva ou dominante. Acomete o tecido conjuntivo de diferentes órgãos, entre eles os olhos, levando a alterações em padrões anatômicos e subsequentes complicações. O presente artigo relata o caso de uma paciente feminina de 24 anos com crises intermitentes de bloqueio pupilar em ambos os olhos. Descreve-se o diagnóstico de síndrome de Weill-Marchesani, assim como o manejo clínico-cirúrgico da doença, cujo desfecho envolveu iridotomia e cirurgia de catarata. Destaca-se a importância do conhecimento do curso da doença pelo oftalmologista, assim como a realização do diagnóstico precoce, dado que suas complicações podem ser de alta gravidade oftalmológica se não manejadas adequadamente.
Palavras-chave: Weill-Marchesani; Glaucoma; Microesferofacia; Ectopia Lentis.
INTRODUCTION
Weill-Marchesani syndrome (WMS), also known as congenital mesodermal dystrophy, is a rare systemic disease that affects the connective tissue. Its earliest reports were made in 1932 and 1939 by Weill and Marchesani, and its phenotypic characteristics are short stature, brachydactyly, and joint stiffness1. The most common ophthalmological complication is microspherophakia, which can lead to intermittent pupillary closure1,2.
Although rare, WMS can affect various organs and tissues and should be readily suspected and recognized when present. Follow-up with other medical specialties is also essential to investigate associated systemic changes. We report the case of a patient with angular closure episodes secondary to WMS and perform a review of the condition. We discuss the challenging surgical intervention performed and emphasize the importance of knowledge of this disease and its early management in ophthalmological practice.
CASE REPORT
Patient J.C.C.S., a 24-year-old female, presented to our service in December 2020 complaining of eye pain episodes in both eyes (OU). The patient denied any comorbidities and continuous use of medications. She reported a family history of two brothers with unknown ophthalmological pathologies. The patient had a short stature (156 cm) and brachydactyly.
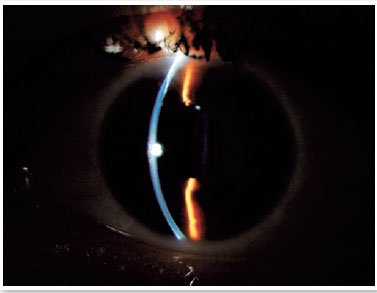
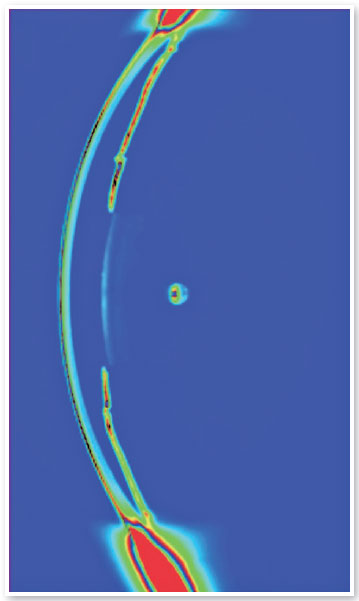
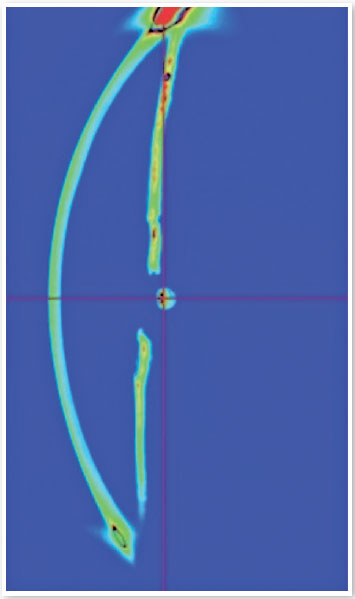
On ophthalmological examination, the best-corrected visual acuity was 20/30 in the right eye (OD), with a refraction of -13.00 spherical and -1.25 cylindrical at 20 degrees, and 20/30 in the left eye (OS), with a refraction of -15.00 spherical and -1.75 cylindrical at 125 degrees. Biomicroscopy revealed microspherophakia (Figure 1), a shallow anterior chamber (Figures 2 and 3) and a golden ring (Figure 4) in the lens. The rest of the examination was normal, with no signs of phacodonesis or other complications.


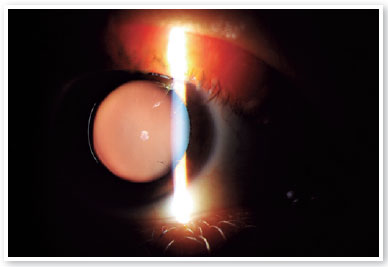
Intraocular pressure was 13mmHg in OD and 14mmHg in OS, and the iridocorneal angle was open 360 degrees in OU on gonioscopy. Fundoscopy was normal and showed a cup-to-disc ratio of 0.3. The clinical symptoms raised the suspicion of WMS, which might be causing intermittent episodes of pupillary block in OU. An OU iridotomy and evaluation by a cataract surgeon were then performed.
Subsequently, the patient underwent phacoemulsification with femtosecond anterior capsulotomy in the OS (Figures 5 and 6). During the procedure, it was necessary to implant a capsular tension ring because of zonular dehiscence, a characteristic of the syndrome. A toric intraocular lens was implanted in the capsular bag. One month after the procedure, the patient was asymptomatic and had an uncorrected visual acuity of 20/25 in the operated eye. Biomicroscopy revealed an increase in the anterior chamber depth. The patient is under ophthalmological follow-up, with a plan of approach involving phacoemulsification in the contralateral eye.
DISCUSSION
WMS, a rare systemic disease with an estimated prevalence of 1:100,000, is characterized by the involvement of connective tissue in various organs. It has either autosomal recessive inheritance, related to the genes ADAMTS-10, ADAMTS-17, and LTPBP2, or autosomal dominant inheritance, which in turn is linked to the polymorphism in the FBN1 gene, the same as in Marfan syndrome1. Its diagnosis is usually clinical, but a search for these genes can help in cases where the diagnosis is inconclusive.
Clinically, the syndrome presents with short stature, brachydactyly (Figure 7), joint stiffness, and ophthalmological changes1-3. Among these, microspherophakia, characterized by a small and circular lens, is present in up to 94% of patients and can result in lenticular myopia, ectopia lentis, retinal detachment, and glaucoma due to pupillary block1,2,4. Ectopia lentis, often located inferiorly, typically appears in late childhood and early adulthood1,2. Marfan syndrome and homocystinuria, diseases that can also lead to ectopia lentis, are included in the differential diagnosis of this pathology.

The pathophysiology of the disease is currently explained by a small ciliary body and elongated zonules, leading to a lower traction force on the lens and, consequently, a circular shape of the lens. These changes are linked to increased mobility of the lens, leading to its anterior displacement and pupillary block. This can be aggravated or complicated by therapy with miotics; therefore, the prescription of miotics in cases of suspected WMS should be carefully considered5.
Management of WMS mainly includes avoiding pupillary block, to which the patients are predisposed. To reverse an acute crisis of pupillary block, nonsurgical options can be attempted, such as keeping the patient in the supine position, manual posterior displacement of the lens, aqueous humor suppressant medications, and analgesia. Iridectomy/iridotomy, as well as iridoplasty, can help but do not solve the causative mechanism, requiring lensectomy later, a surgical procedure complicated by the ocular anatomical characteristics of the syndrome6.
The zonular fragility that may be present, associated with microspherophakia and decreased anterior chamber depth, can make phacoemulsification challenging in these patients7,8. The choice of a capsular tension ring implant depends on the presence and extent of zonular dehiscence7,9. In this case, the use of the same contributed to the success of the procedure.
In the biomicroscopy examination with the pupil dilated, the visualization of a golden reflex on the margins of the lens upon retroillumination (golden ring)10,11 occurs because of microspherophakia and should always raise the suspicion of WMS, particularly in patients with high myopia, and even more so if it is associated with short stature and/or brachydactyly, as was the case with this patient. In already complicated cases, such as the one reported, delaying surgical treatment may worsen the visual prognosis due to acute glaucoma crises due to pupillary block12 and progressive endothelial damage resulting from lenticulocorneal examination in cases of anterior lens dislocation.
Because the ophthalmological symptoms are characteristic, patients with WMS may initially present to ophthalmologists, which enables and emphasizes the importance of an early diagnosis by the ophthalmologist and referral to other clinical specialties involved. Early management of ophthalmological involvement in these patients is crucial to avoid serious complications13, such as acute glaucoma and blindness. If surgical intervention is necessary in already complicated cases, it must be meticulously planned because of the challenging nature of the anatomical changes peculiar to the syndrome.
REFERENCES
1. Marzin P, Cormier-Daire V, Tsilou E. Weill-Marchesani Syndrome. 2007 Nov 1 [updated 2020 Dec 10]. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2020.
2. Chang BM, Liebmann JM, Ritch R. Angle closure in younger patients. Trans Am Ophthalmol Soc. 2002:100: 201-12; discussion 212-4.
3. Verloes A, Hermia JP, Galand A, Koulischer L, Dodinval P. Glaucoma-lens ectopia-microspherophakia-stiffness-shortness (GEMSS) syndrome: a dominant disease with manifestations of Weill-Marchesani syndromes. Am J Med Genet. 1992;44(1):48-51.
4. Faivre L, Dollfus H, Lyonnet S, Alembik Y, Mégarbané A, Samples J, et al. Clinical homogeneity and genetic heterogeneity in Weill-Marchesani syndrome. Am J Med Genet. 2003 Dec 1;123A(2): 204-207.
5. Jensen AD, Cross HE, Paton D. Ocular complications in the Weill-Marchesani syndrome. Am J Ophthalmol. 1974;77(2):261-9.
6. Ritch R, Solomon LD. Argon laser peripheral iridoplasty for angleclosure glaucoma in siblings with Weill-Marchesani syndrome. J Glaucoma. 1992;1(4):243-247.
7. Groessl SA, Anderson CJ. Capsular tension ring in a patient with Weill-Marchesani syndrome. J Cataract Refract Surg. 1998;24(8):1164-1165.
8. Chung JL, Kim SW, Kim JH, Kim TI, Lee HK, Kim EK. A case of Weill-Marchesani syndrome with inversion of chromosome 15. Korean J Ophthalmol. 2007;21(4):255-260.
9. Cionni RJ, Osher RH. Endocapsular ring approach to the subluxed cataractous lens. J Cataract Refract Surg. 1995;21(3):245-249.
10. Singh S, Yangzes S, Ram J. The golden ring. Oman J Ophthalmol. 2019;12(2):141.
11. Nayak B, Sinha G, Patil B, Khokhar S. Golden ring in the eyes: Weill-Marchesani syndrome. BMJ Case Rep. 2015 May 24:2015:bcr2015210547.
12. Abdi R, Bourakba S, Chariba S, Maadan A, Sekhsoukh R. [A case of secondary glaucoma in Weill-Marchesani syndrome]. J Fr Ophtalmol. 2020;43(3):e109-11.French.
13. Shahriar NA, Roy SR. Timely diagnosis of Weill-Marchesani syndrome can preserve vision and prevent complication: A case report. BIJCROO. 2022;1(1):26-8.
| AUTHORS INFORMATIONS |
|
 |
» Amanda Geara http://orcid.org/0000-0001-7056-3958 http://lattes.cnpq.br/2614558505262993 |
 |
» Vanessa Nicola Labrea http://orcid.org/0000-0003-2158-6920 http://lattes.cnpq.br/0724349260025686 |
 |
» Luiz Fernando Interaminense Garbers http://orcid.org/0000-0003-0239-4149 http://lattes.cnpq.br/4945236956766062 |
 |
» Eric Vieira http://orcid.org/0000-0001-6856-5073 http://lattes.cnpq.br/8518586929681594 |
 |
» Liana G. Iankilevich http://orcid.org/0000-0003-2287-3788 http://lattes.cnpq.br/7740035733089770 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
October 10, 2022.
Accepted on:
October 11, 2023.