Ana Bárbara Dias Lopes Urzedo; Paula Basso Dias; Nayara Teixeira Flügel;Daniel Wasilewski
DOI: 10.17545/eOftalmo/2023.0023
ABSTRACT
The objective of this study is to report a case of unilateral leukoma due to a herpetic ulcer treated with keratopigmentation (corneal tattoo) in a 53 years old male patient who presented with an aesthetic complaint due to chronic corneal opacity in the left eye. Corrected visual acuity was 20/20 in the right eye and hand movement in the left eye. Biomicroscopy of the right eye showed no alterations, whereas the left eye had total leukoma with superficial and deep neovessels at 360°, athalamia, and inferior nasal corneal thinning. Keratopigmentation in the left eye was indicated to improve the patient’s quality of life and self-confidence. It was performed using the superficial manual technique by mixing two professional ink hues to achieve adequate coloration concordant to the contralateral eye. The patient was extremely satisfied and there were no complications in the immediate postoperative period. In the late postoperative period, he developed a slight calcification of the pigment, but was still satisfied with the aesthetic result. This case shows a classic indication of corneal tattoo, namely a unilateral leukoma with great aesthetic repercussions and asymmetry. Keratopigmentation can also be used to functionally treat photophobia or diplopia associated with the absence of the iris (due to atrophy, trauma, aniridia, or coloboma).
Keywords: Corneal tattoo; Keratopigmentation; Corneal leukoma.
RESUMO
O objetivo deste é relatar um caso de leucoma unilateral por úlcera herpética tratado com ceratopigmentação (tatuagem corneana). Homem, 53 anos, com queixa estética devido a opacidade corneana crônica em olho esquerdo. Acuidade visual com correção de 20/20 em olho direito e movimento de mãos em olho esquerdo. A biomicroscopia de olho direito não havia alterações, enquanto o olho esquerdo apresentava leucoma total com neovasos superficiais e profundos 360°, atalamia e afinamento corneano nasal inferior. Indicada a ceratopigmentação no olho esquerdo, a fim de melhorar a qualidade de vida e autoconfiança do paciente. Realizada com a técnica superficial manual, onde duas colorações de tinta profissional foram misturadas para atingir coloração adequada e simétrica ao olho contralateral. Paciente extremamente satisfeito, evoluiu sem apresentar complicações no pós-operatório imediato. No pós-operatório tardio, evoluiu com leve calcificação sobre o pigmento, mas continuava satisfeito com o resultado estético. O caso descrito mostra uma indicação clássica de tatuagem corneana - leucoma unilateral com grande repercussão estética e assimetria. A ceratopigmentação também pode ser utilizada para tratar funcionalmente a fotofobia ou diplopia associada à ausência da íris (por atrofia, trauma, aniridia ou coloboma).
Palavras-chave: Tatuagem corneana; Ceratopigmentação; Leucoma corneano.
INTRODUCTION
Corneal tattooing or keratopigmentation (KTP) is a method used to cosmetically or functionally treat corneal opacities or defects of the iris or the pupil(1–4) It is considered an alternative to the use of prostheses or contact lenses, especially in patients with severe cosmetic defects who are intolerant of contact lenses and are considered at a high risk for penetrating transplantation.(5)
Its purpose can be cosmetic, aiming to reestablish the symmetry between the eyes, or therapeutic, such as to treat photophobia, diplopia, halo vision, and glare, secondary to some anatomical alteration of the eye.(1,4)
Currently, two techniques for keratopigmentation are known: superficial, further divided into manual (SMK) and automated (SAK), and intrastromal, further divided into manual (MIK) and femtosecond-assisted (FAK).(1,6)
KTP can have both intraoperative and postoperative complications, the most common being light sensitivity, and the least common being changes in magnetic resonance imaging (distortion in the eyeball) and visual field limitations.(1,7–9)
CASE REPORT
A 53-year-old man sought treatment at the Federal University of Paraná Clinics Hospital, in Curitiba, Brazil. He presented with an aesthetic complaint of chronic corneal opacity in the left eye (OS) without any pain. He reported a history of herpetic ulcer lasting for 1 year, without treatment at the time. The ophthalmologic examination revealed a corrected visual acuity of 20/20 in the right eye (OD) and hand movement (HM) in OS. Biomicroscopy showed no alterations in OD, whereas OS showed no tactile sensitivity, total leukoma with calcium deposits, superficial and deep neovessels at 360°, athalamia, and inferior nasal corneal thinning, with no signs of active inflammation. Due to the total corneal leukoma, it was not possible to perform retinal mapping. An ultrasound showed multiple heterogeneous vitreous echoes in OS, suggestive of an intense chronic inflammatory process.
In subsequent consultations, the patient progressed with light-perception (LP) CVA in OS. Due to the changes of the vitreous in the ultrasound and the alterations of the anterior segment, as described above, and the great chance of rejection of a corneal transplant by the superficial and deep diffuse neovessels; the case was discussed with the patient. Considering the poor visual prognosis, keratopigmentation was suggested for the OS to improve the patient’s quality of life and self-confidence, which was his greatest desire at that moment.
KTP was performed using SMK in which micro-punctures are applied to the superficial layers of the stroma (Figure 1). The technique consisted of removing the epithelium and delineating the central corneal area (which defines the pupillary diameter) with a dermatographic pen, with the subsequent introduction of an angled insulin needle as a cystotome at 90° in the corneal stroma. Two hues of the Electric Ink® Easy Glow Professional® 30 mL professional tattoo ink (black for the pupil and a mixture of black with dark brown for the iris, so as to achieve an appropriate coloration, concordant to the contralateral eye). The inks were composed of deionized water, non-ionic surfactant, vegetable glycerin, propylene glycol, and micronized inorganic (mineral) and organic pigments (CI 77891, 11741, 21110, 12475, 73915, 51319, 74160, 74260, and 77266), and were sterilized using gamma rays.
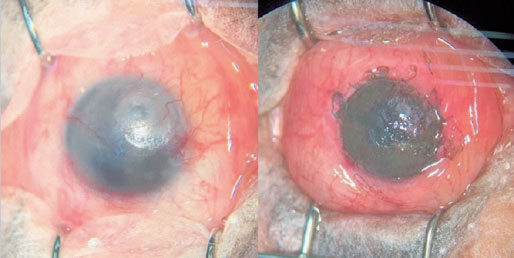
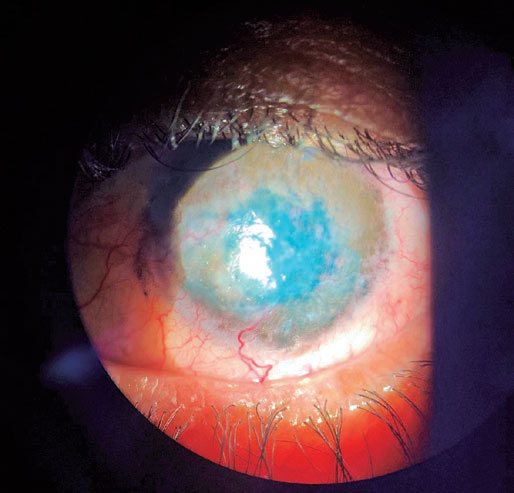
During the postoperative period, topical corticosteroids (1% prednisolone acetate) and antibiotics (moxifloxacin hydrochloride) were prescribed in addition to the placement of a therapeutic contact lens for more comfort. Herpesvirus (HSV) prophylaxis was performed with aciclovir 800 mg/day 5 days before the procedure and in the postoperative period, during the period of topical corticosteroid use, due to the patient’s history of herpetic ulcer. The patient was extremely satisfied and progressed without pigment fading or other complications during the immediate one-week postoperative period (Figure 2), remaining with LP CVA. During the late postoperative period (1 year), the patient developed slight calcification of the pigment (Figures 3 and 4), but was still satisfied with the aesthetic result.


DISCUSSION
KTP is an ancient technique, first described more than 2000 years ago in Greece by the physician Galen of Pergamon, and later in 450 CE by the physician Aetius, in an attempt to mask corneal opacities.(1,3,10)
The cosmetic indications of KTP include total or partial corneal leukoma, opacification of the donor-recipient border in eyes with keratoplasty, chronic corneal edema, congenital glaucoma, and others.(1,2) Moreover, there are some reports of KTP being used for elective change in eye color.(11,12) It must be noted that an asymmetry in the appearance of the eyes often directly affects the patient’s quality of life and self-confidence, as was the case with the patient in this report. Other therapeutic indications of KTP are for aniridia, iridodialysis, iris atrophy, Urrets-Zavalia syndrome, monocular diplopia, and other issues. Photophobia, halo vision, and glare are common complaints in patients with these conditions.(1,4,5)
Among the superficial techniques used in KTP, the pioneering one is the SMK technique in which micropunctures are made in the superficial layers of the stroma, and this maneuver is repeated until the appropriate amount of pigment is introduced into the superficial cornea.(13) This was the technique used in the present case, with an immediately symmetrical aesthetic result after surgery. Conversely, SAK, consists of making micropunctures using an automatic puncturing device.(1,13)
In the MIK technique, the pigment is inserted into the anterior stroma through an intrastromal corneal pouch. This has the advantages of greater safety, speed, and tolerability, leaving the corneal surface intact and consequently reducing the rate of complications.(1,4,13) In contrast, FAK is an intrastromal technique in which stromal tunnels are bored with a femtosecond laser, with the depth defined through a pachymetry map, followed by the application of a colored pigment in the most superficial part of the tunnels and a darker pigment in the deeper parts in an attempt to imitate the anatomy of the iris.(4,14).
Previously reported intraoperative complications include perforation, secondary infection, epithelial erosions, and subconjunctival pigmentation; postoperative complications include sensitivity to light, inconsistent staining of the opaque area, pigment fading, uveitis, corneal edema, conjunctivitis, epithelial defects, and visual field limitations.(1,9,15,16) One Brazilian case series described eight patients that underwent KTP using the double lamellar pouch technique followed by stromal micropuncture, and corneal perforation was reported in only one patient (12.5%), thus being the only case of intra- or postoperative complication.(17) In the study conducted by Alió et al., considered the father of modern KTP, 234 eyes underwent SAK, FAK, and MIK techniques in their study. The most common complication was sensitivity to light (49%) followed by color fading (19%) and color change (19%).(9) A Brazilian report showed pigment stability in the late postoperative period (1 year) in a patient with leukoma and corneal irregularities who underwent KTP associated with lamellar keratoplasty.(18)
It is known that HSV remains in a state of latency in the trigeminal ganglion, where viral RNA is constantly produced. Ultraviolet exposure, fever, tissue lesions, hormonal disorders, or immunosuppression can cause viral reactivation in tissues innervated by the trigeminal ganglion, causing different forms of HSV keratitis: epithelial, stromal, or endothelial.(19) Thus, in the present case, we decided to administer aciclovir in prophylactic doses due to the patient’s history of herpetic ulcer.
The pigments used for KTP are fundamentally stable, safe, and can withstand long periods of exposure to light while preserving the transparent nature of the cornea. Micronized mineral pigments have the advantage over natural pigments of reducing the chance of developing foreign-body reactions.(1,3,9). In the case described, mineral pigments were chosen, and the patient progressed with no organic or functional complications.
The case described shows a classic indication for corneal tattoo-unilateral leukoma with great aesthetic repercussion and asymmetry. The procedure was performed without complications, and the patient was extremely satisfied with the result, even after presenting a slight recurring calcium deposition during the late postoperative period.
REFERENCES
1. Hasani H, Es’haghi A, Rafatnia S, Alilou S, Abolmaali M. Keratopigmentation: a comprehensive review. Eye (Lond). 2020 Jun;34(6):1039-1046.
2. Amesty MA, Rodriguez AE, Hernández E, De Miguel MP, Alio JL. Tolerance of Micronized Mineral Pigments for Intrastromal Keratopigmentation: A Histopathology and Immunopathology Experimental Study. Cornea. 2016;35(9):1199-205.
3. Ziegler SL. Multicolor Tattooing of the Cornea. Trans Am Ophthalmol Soc. 1922;20:71-87.
4. Alio JL, Rodriguez AE, Toffaha BT. Keratopigmentation (corneal tattooing) for the management of visual disabilities of the eye related to iris defects. Br J Ophthalmol. 2011;95(10):1397-401.
5. Sirerol B, Walewska-Szafran A, Alio JL, Klonowski P, Rodriguez AE. Tolerance and biocompatibility of micronized black pigment for keratopigmentation simulated pupil reconstruction. Cornea. 2011;30(3):344-50.
6. Alió JL, Amesty MA, Rodríguez A, El Bahrawy M. Text and atlas on corneal pigmentation. India: JP Medical Ltd; 2015.
7. Mannis MJ, Eghbali K, Schwab IR. Keratopigmentation: a review of corneal tattooing. Cornea. 1999;18(6):633-7.
8. Pitz S, Jahn R, Frisch L, Duis A, Pfeiffer N. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002;86(4):397-9.
9. Alio JL, Al-Shymali O, Amesty MA, Rodriguez AE. Keratopigmentation with micronised mineral pigments: complications and outcomes in a series of 234 eyes. Br J Ophthalmol. 2018;102(6):742-7.
10. Samderubun EMvdV, Kok JH. Dermatology as a modern treatment for coloring leucoma corneae. Cornea. 1994;13(4):349-53.
11. Alió JL, Rodriguez AE, El Bahrawy M, Angelov A, Zein G. Keratopigmentation to Change the Apparent Color of the Human Eye: A Novel Indication for Corneal Tattooing. Cornea. 2016;35(4):431-7.
12. D’Oria F, Abu-Mustafa SK, Alio JL. Cosmetic Change of the Apparent Color of the Eye: A Review on Surgical Alternatives, Outcomes and Complications. Ophthalmol Ther. 2022;11(2):465-77.
13. Al-Shymali O, Rodriguez AE, Amesty MA, Alio JL. Superficial keratopigmentation: an alternative solution for patients with cosmetically or functionally impaired eyes. Cornea. 2019;38(1):54-61.
14. Alio JL, Rodriguez AE, Toffaha BT, El Aswad A. Femtosecondassisted keratopigmentation double tunnel technique in the management of a case of Urrets-Zavalia syndrome. Cornea. 2012;31(9):1071-4.
15. Calas E, Gueudry J, Muraine M. Severe color change in corneal tattoos: Report of 3 cases. J Fr Ophtalmol. 2018;41(10):e469-e475.
16. Tone SO, Li DQ, Ashkenazy Z, Borovik A, Slomovic AR, Rootman DS, et al. Simple preoperative ink test as a novel adjunct to intrastromal keratopigmentation for post-laser peripheral iridotomy dysphotopsias. Cornea. 2017;36(10):1282-4.
17. Xavier LD, Becker CU, Salomão HM, Costa AX. Ceratopigmentação (tatuagem corneana): utilização de técnicas combinadas para melhora estética em olhos de pacientes com opacidades corneanas. Rev Bras Oftalmol. 2022;81:e0031.
18. Berger A, Perez MF, Pazos HSB, De Biase SG, Gomes JÁP. Transplante lamelar de córnea associado à tatuagem estromal para tratamento de leucoma: relato de caso. Arq Bras Oftalmol. 2009;72(2):247-50.
19. Nowińska A. Recent Advances in the Diagnosis and Management of Herpetic Keratitis. Infectious Eye Diseases - Recent Advances in Diagnosis and Treatment. 2021. IntechOpen. DOI: 10.5772/ intechopen.96898.
INFORMAÇÃO DOS AUTORES


Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
December 1, 2022.
Accepted on:
May 6, 2023.