Renato Bredariol Pereira1; Moisés Moura de Lucena2; Leonardo Luis Cassoni2; Rodrigo Jorge2
DOI: 10.17545/eOftalmo/2023.0020
ABSTRACT
Vasoproliferative retinal tumor is an acquired disease characterized by vascular lesions, usually located in the pre-equatorial and inferotemporal region, that can cause exudates, macular edema, epiretinal membrane, and retinal detachment. Approximately 75% of cases are idiopathic ocular conditions and 25% are secondary to other eye diseases such as uveitis, retinal detachment, congenital toxoplasmosis, and Coats disease. Vasoproliferative retinal tumors are clinically diagnosed, and they can be confirmed by fluorescein angiography and ocular ultrasonography. Treatment, when indicated, involves cryotherapy, laser photocoagulation, surgical excision, radiation therapy, and intravitreal injections of antiangiogenic drugs. In this article, we describe the occurrence of a vasoproliferative retinal tumor secondary to chronic rhegmatogenous retinal detachment in a high myopic patient and the outcomes of its treatment with cryotherapy and scleral buckle surgery.
Keywords: Retina; Vasoproliferative tumor; Retinal detachment.
RESUMO
O tumor vasoproliferativo da retina é uma doença adquirida caracterizada por lesões vasculares, usualmente localizadas em região pré-equatorial e inferotemporal, que podem causar exsudatos, edema macular, membrana epirretiniana e descolamento de retina. Aproximadamente 75% dos casos são idiopáticos e 25% são secundários a outras doenças oculares como uveíte, descolamento de retina, toxoplasmose congênita e doença de Coats. O diagnóstico é clínico. A angiofluoresceinografia e a ultrassonografia ocular contribuem para a confirmação diagnóstica. O tratamento, quando indicado, pode ser feito por meio de crioterapia, fotocoagulação a laser, excisão cirúrgica, radioterapia e injeções intravítreas de antiangiogênicos. Nesse artigo, descrevemos a ocorrência de tumor vasoproliferativo da retina secundário a descolamento de retina regmatogênico crônico em paciente alto míope, além dos resultados do tratamento cirúrgico com crioterapia e buckle escleral.
Palavras-chave: Retina; Tumor vasoproliferativo; Descolamento de retina.
INTRODUCTION
Vasoproliferative retinal tumor (VPT) is a rare benign lesion that affects mostly young, caucasian adults. Although the pathophysiology is not fully understood, VPT is though to occur as a result of vascular proliferation reactive to ischemic and/or inflammatory phenomena. Histological study shows glial cells interconnected with the thin and dilated capillary network, with the presence of exudates and macrophages. Clinically, VPT presents as reddish-yellow solid masses located in the periphery, often associated with exudative and hemorrhagic changes1,2.
As for classification, VPT can be divided into idiopathic or secondary, with the idiopathic form being more prevalent, accounting for 75% of cases. The secondary form can be related to uveitis, retinitis pigmentosa, retinopathy of prematurity, sickle cell retinopathy, and Coats disease. The lesions are usually single, peripheral, unilateral, located in the temporal-inferior and inferior quadrants, and <10 mm in size. Patients with VPT may have low visual acuity. Other ocular manifestations of the disease are vascular dilatation with or without exudation, sub retinal fibrosis, vitreous hemorrhage and retinal detachment (RD)3.
Although the term vasoproliferative tumor is widely used, it is believed that VPT is not a true tumor and it should be considered as a retinal pseudotumor. No consensus exists thus far regarding the best form of treatment, which must be individualized. The following is a brief case report of VPT secondary to previous chronic rhegmatogenous RD followed by a brief discussion of its treatment.
CASE REPORT
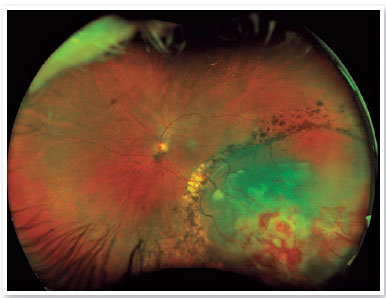
Forty-eight-year-old woman, presented with painless visual loss in the left eye (OS) for 20 days, without associated trauma. She had a past history of high myopia and previous rhegmatogenous RD 18 years ago, treated with laser. On examination, visual acuity was 20/20 in the right eye (OD) with spherical equivalent (SE) of −7.50 spherical diopters (SD) and 20/60 in OS with SE of −6.25 SD. Biomicroscopic examination showed clear lens in both eyes. Ocular fundus examination of OD was normal. In the left eye there was RD affecting the macula, extending to the inferior and inferior temporal region, where a vasoproliferative lesion with exsudation and sub-retinal hemorrhage was visualized (Figure 1). Laser marks were visualized delimiting inferior temporal area, in addition to a retinal tear in the inferior temporal retinal periphery. Ultrasonography (US) of the OS ruled out cancer lesions or alterations in the choroid. Fluorescein angiography showed neovessels in the lesion topography (Figure 2), whereas optical coherence tomography (OCT) of the macula showed subretinal fluid affecting the foveal center (Figure 3A).

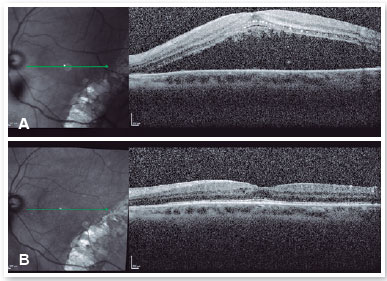
Under the diagnostic hypothesis of VPT in OS with associated regmatogenous RD, initial treatment with 0.05 ml of intravitreal Bevacizumab was chosen to reduce lesion exsudative changes. On reevaluation after 14 days, the patient maintained the lesion and retinal detachment, with corrected visual acuity of 20/20 (OD) and 20/125 (OS). Surgical treatment with cryotherapy, inferotemporal drainage of subretinal fluid and primary retinopexy was subsequently chosen. The procedure was uneventful and the patient progressed satisfactorily. At the 3rd postoperative month, the retina remained attached and the patient had visual acuity in OD of 20/20, with SE of -7.50 SD, and in OS of 20/20, with SE of -9.25 SD (Image 3B).
DISCUSSION
The diagnosis of VPT is essentially clinical. Additional examinations such as fluorescein angiography (FA) and US can assist in the diagnosis. Often the FA has a limited role because of the peripheral tumor location; when possible, rapid filling is observed in the arterial phase, while in the venous phase, leakage and staining remain in the late phases3. However, US shows a medium to high reflectivity structure, with the absence of a kappa angle and no signs of internal vascularity4.
The management of VPT varies considerably and treatment is usually instituted when there is loss of visual acuity as in cases of macular edema, epiretinal membrane, or retinal detachment. When these manifestations are not present, one can opt for expectant management3. Several forms of treatment have been proposed, most notably cryotherapy, laser photocoagulation, photodynamic therapy (PDT), intravitreal injection of antiangiogenic drugs, brachytherapy, and surgical resection.
Cryotherapy is the main therapeutic arsenal5. Due to the peripheral location of the tumors, cryotherapy can be performed transconjunctivally under direct visualization with optical aid. Complications of this treatment modality include macular edema and retinal detachment in the area adjacent to the cryotherapy6.
Brachytherapy is usually indicated in tumors thicker than 2.5 mm associated with retinal detachment. Previous studies have described cases in which brachytherapy with Ruthenium and Iodine led to complete remission of the tumor, except in cases associated with neovascular glaucoma7,8.
Laser photocoagulation, PDT, and intravitreal injection of anti-VEGF agents are usually used in association with another form of treatment. Laser photocoagulation can be used in small tumors while PDT is limited owing to the peripheral location of the tumor9. Intravitreal injection used as monotherapy appears to cause transient remission in tumor size, with recurrence of the lesion during follow-up. The greatest benefit of its application occurs in cases with concomitant macular edema10. Cases of surgical resection are limited to the failure of other therapies or in cases of multiple lesions associated with vitreous hemorrhage11.
Cases of VPT secondary to chronic RD are rare and probably related to chronic hypoxia of the outer layers of the retina due to blood hypoflow and rupture of Bruch’s layer, with growth of the lesion originating from the choroidal vasculature12. Studies have reported VPT formation after various forms of retinal detachment treatment, such as scleral buckle, laser photocoagulation, and vitrectomy12-14.
In the present case, due to the peripheral location of the lesion and the presence of associated rhegmatogenous retinal detachment, we chose to perform primary retinopexy (42 band, inferotemporal drainage and cryotherapy). The patient had a regular follow-up, with good evolution and complete remission of the lesion.
VPT are rare, benign lesions that can cause significant visual impairment. Thus, an individualized assessment must be performed to ensure adequate therapy, whether with clinical, surgical, or observational treatment, in order to preserve the patient’s visual quality. Periodic ophthalmologic evaluation is essential in patients with previous treatment for retinal detachment to look for possible lesions affecting the retinal periphery.
REFERENCES
1. Jain K, Berger A, Yucil Y, McGowan HD. Vasoproliferative tumours of the retina. Eye (Lond). 2003;17(3):364–8.
2. Heimann H, Bornfeld N, Vij O, Coupland SE, Bechrakis NE, Kellner U, Foerster MH. Vasoproliferative tumours of the retina. Br J Ophthalmol. 2000;84(10):1162-9.
3. Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol. 1995;113(5):615-23.
4. Piñeiro-Ces A, Blanco-Teijeiro MJ, Mera-Yáñez MP, Capeans-Tome C. [Ultrasound diagnosis in vasoproliferative tumours of the ocular fundus]. Arch Soc Esp Oftalmol. 2011;86(8):247-53. Spanish.
5. Makdoumi K, Crafoord S. Vasoproliferative retinal tumours in a Swedish population. Acta Ophthalmol. 2011;89(1):91-4.
6. Marback EF, Guerra RL, Maia Junior OO, Marback RL. Retinal vasoproliferative tumor. Arq Bras Oftalmol. 2013;76(3):200–3.
7. Anastassiou G, Bornfeld N, Schueler AO, Schilling H, Weber S, Fluehs D, et al. Ruthenium-106 plaque brachytherapy for symptomatic vasoproliferative tumours of the retina. Br J Ophthalmol. 2006;90(4):447-50.
8. Cohen VM, Shields CL, Demirci H, Shields JA. Iodine I 125 plaque radiotherapy for vasoproliferative tumors of the retina in 30 eyes. Arch Ophthalmol. 2008;126(9):1245-51.
9. Blasi MA, Scupola A, Tiberti AC, Sasso P, Balestrazzi E. Photodynamic therapy for vasoproliferative retinal tumors. Retina. 2006;26(4):404-9.
10. Rogers C, Damato B, Kumar I, Heimann H. Intravitreal bevacizumab in the treatment of vasoproliferative retinal tumours. Eye (Lond). 2014;28(8):968-73.
11. Yeh S, Wilson DJ. Pars plana vitrectomy and endoresection of a retinal vasoproliferative tumor. Arch Ophthalmol. 2010;128(9): 1196-9.
12. Felder KS, Brockhurst RJ. Retinal neovascularization complicating rhegmatogenous retinal detachment of long duration. Am J Ophthalmol. 1982;93(6):773-6.
13. Gottlieb F, Fammartino JJ, Stratford TP, Brockhurst RJ. Retinal angiomatous mass. A complication of retinal detachment surgery. Retina. 1984 Summer-Fall;4(3):152-7.
14. Gray RH, Gregor ZJ. Acquired peripheral retinal telangiectasia after retinal surgery. Retina 1994;14(1):10–3.
AUTHOR’S INFORMATION

Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
December 1, 2022.
Accepted on:
March 11, 2023.