Renata Caroline Ferreira Gomes1; Isabela Martins Melo1; Déborah Schulthais Ramos2; Marcela Mattar de Melo Miranda Salim1
DOI: 10.17545/eOftalmo/2022.0006
ABSTRACT
Dysthyroid optic neuropathy is a severe complication of Graves orbitopathy resulting from the compression of the optic nerve by enlarged extraocular muscles and orbital fat. Reduction in visual acuity, visual field loss and relative afferent pupillary defect are some of its symptoms, which can progress if not treated correctly, leading to blindness in 30% of patients. In this report, we will discuss the case of a female patient with dysthyroid optic neuropathy, complaining of progressive visual loss in her right eye, but with only mild changes in her visual functions. We will elucidate the diagnosis and challenging treatment of this clinical condition, which requires a close and cautious follow-up.
Keywords: Dysthyroid Optic Neuropathy; Thyroid Eye Disease; Graves Orbitopathy; Treatment.
RESUMO
A neuropatia óptica distireoidiana é uma complicação da orbitopatia de Graves resultante da compressão do nervo óptico pelos músculos extraoculares e pela gordura orbitária. Redução da acuidade visual, alterações do campo visual e defeito pupilar aferente relativo são alguns dos sintomas resultantes dessa neuropatia, que, se não tratada corretamente, apresenta 30% de chance de evoluir para cegueira. Neste relato, discutiremos o caso de uma paciente do sexo feminino com quadro de neuropatia óptica distireoidiana, queixando-se de embaçamento visual progressivo em olho direito, porém com pouca alteração da função visual. Elucidaremos o diagnóstico e tratamento desafiador dessa condição clínica, que requer acompanhamento próximo e cauteloso.
Palavras-chave: Neuropatia Óptica Distireoidiana; Doença dos Olhos da Tiroide; Orbitopatia de Graves; Tratamento.
INTRODUCTION
Dysthyroid optic neuropathy (DON) is the most severe form of Graves orbitopathy (GO), occurring due to the compression of the optic nerve by enlarged extraocular muscles and orbital fat, within the rigid ocular bone structure. Luckily, DON is a rare complication, affecting only about 5% of patients with GO1-2. Nevertheless, when not diagnosed and treated correctly, it carries a considerable risk of morbidity, leading to blindness in 30% of patients3.
Abnormalities in visual function such as visual acuity, visual field, color vision and contrast sensitivity, are observed in most patients affected by DON2. Other common findings that can be found in the ophthalmological exam are optic nerve edema and relative afferent pupillary defect (RAPD)1. The aim of this report is to describe the treatment of DON in a patient with mild changes in her visual function.
CASE REPORT
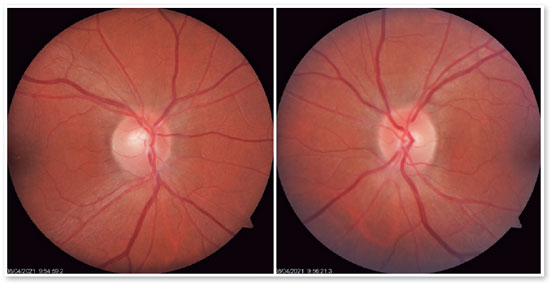
A 48-year-old female patient was referred to our department with a previous diagnosis of Graves’ disease, complaining of progressive visual blurring in the right eye (OD) and near vision diplopia, worse in downward gaze. She had undergone treatment with radioactive iodine and strabismus surgery to correct a restrictive squint in 2018. On ophthalmological examination, she had a bilateral proptosis, eyelid retraction and lid lag. Pupils were round and equal in size, without RAPD. Best corrected visual acuity (BCVA) was 20/30 in OD and 20/25 in OS. Color vision, assessed with Panel 15, was found normal in both eyes (OU) and contrast sensitivity, assessed with Pelli-Robson Contrast Sensitivity Chart, had a reduction in OD. Haag-Streit Octopus standard automated perimetry (SAP) showed few relative central and paracentral scotomas in OD and no abnormalities in OS (Figure 1). Slit-lamp examination revealed mild conjunctival hyperemia, without caruncle swelling, and an elevated optic disc, with blurred margins in OU (Figure 2). Optic disc Zeiss Cirrus spectral-domain optical coherence tomography (SD-OCT) was performed, showing an increased retinal nerve fiber layer (RNFL) thickness, compatible with optic disc edema (Figure 3). Orbital magnetic resonance imaging (MRI) revealed enlarged extraocular muscles, specially the medial and lateral rectum, crowded apex and a compression of the optic nerve in the optic canal (Figure 4).
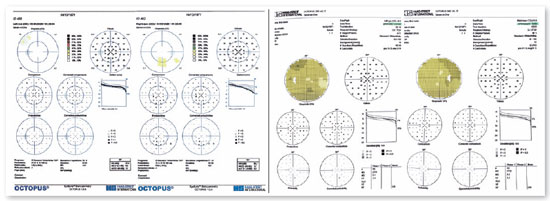
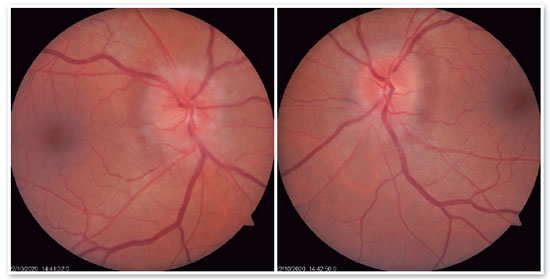
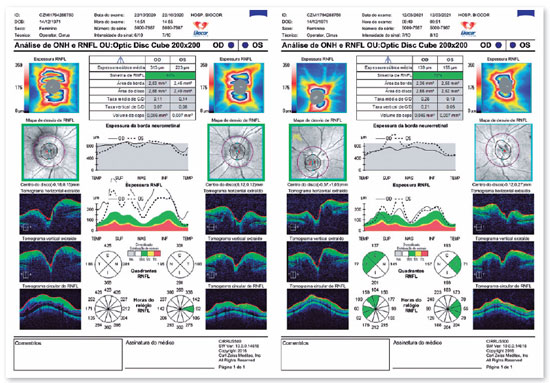

Intravenous treatment with methylpredinisolone 500 mg per day for three days was performed, with improvement in the optic disc edema and BCVA (OD 20/25 and OS 20/20). The patient received hospital discharge to follow-up with the Neuro-Ophthalmology Department at Biocor Instituto. A new appointment was scheduled in two weeks, nevertheless the patient only returned after seven weeks complaining of worsening vision. On her new clinical examination, she presented BCVA of 20/40 in OD and 20/30 in OS and worsening of the optic disc edema, especially in OS (Figure 5). She underwent a new cycle of intravenous methylprednisolone with a higher dose of 1g per day for five days and afterwards, oral prednisone 60 mg per day, duration to be determined. After five weeks of treatment, her affected visual functions were finally completely normalized (BCVA and SAP), both fundus examination and SD-OCT showed an important reduction of the optic disc edema (Figure 3).
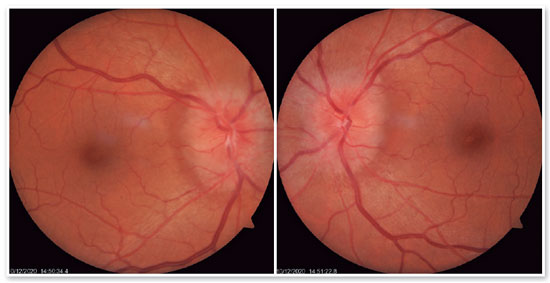
Nevertheless, before starting the steroid taper, she noticed mild visual changes and came back for a new exam. Surprisingly, the optic disc edema relapsed, with BCVA of 20/25 in OD and 20/20-2 in OS, with a slight reduction in the contrast sensitivity test in OD. At this point, with such a high-dose maintenance treatment of prednisone, its tolerance problems and side effects, an endoscopic orbital decompression was programmed. An endonasal bilateral concurrent sphenoethmoidectomy was performed in the standard fashion with both the Neurosurgery and the Ophthalmology staff. After two weeks of post operation recovery, the patient presented an esthetical improvement of the proptosis and, most important, full recovery from the visual deficits including the resolution of the optic disc edema (Figure 6).
DISCUSSION
DON is a rare and potentially irreversible complication of GO, an autoimmune disease caused by the activation of fibroblasts by autoantibodies against thyroid receptors. Ocular fibroblasts have receptors for thyroid stimulating hormone and become a target of cellular and humoral autoimmunity4-5. This ultimately results in the deposition of glycosaminoglycans and connective tissue remodeling, leading to extraocular muscle enlargement and orbital fat expansion, which causes a compression of the optic nerve at the level of the optic canal5, as demonstrated in the MRI in the reported case.
Optic nerve involvement commonly results in visual function loss, with reduced color vision and contrast sensitivity, low visual acuity, visual field scotomas, in addition to RAPD and optic disc edema. Congestive symptoms generally precede visual loss, which is usually asymmetrical6. In our case it was not different, visual acuity was mildly affected at the time of diagnosis, although congestive symptoms were already extremely evident (proptosis, optic disc edema, enlarged extraocular muscles). Even though color testing was normal, Desaturated Panel-15 would likely be a better option to evaluate DON, since it has a greater sensitivity and, thus, ability to discriminate acquired dyschromatopsia.
The diagnosis of DON was suggested by the bilateral optic disc edema and an increased RNFL thickness in the SD-OCT, concurrent with the MRI findings, which demonstrated a compression of both optic nerves.
When DON is not treated adequately in its early stages, it may lead to blindness in up to 30% of cases3. In the current literature, recommended treatments include intravenous corticosteroids, orbital decompression, and orbital radiotherapy, although the latter is still questionable7. According to the 2008 Consensus of Eugogo, high dose intravenous corticosteroid is the first line treatment for DON. Nevertheless, if clinical response is insufficient after two weeks, orbital decompression is the next step to consider8.
Since our patient presented with relapsing optic disc edema and visual function deterioration, despite high doses of methylprednisolone pulse therapy and maintenance treatment with oral prednisone, an endoscopic orbital decompression was performed to obtain an ultimate clinical end point. It is noteworthy that although visual recovery can be seen in approximately 43% of cases that used venous methylprednisolone 9, steroids will rarely cause a reduction in the proptosis, and recurrences can often occur. Thus, surgical decompression may still be warranted10.
Surgery for DON should decompress the optic nerve at the orbital apex by decreasing the volume of soft tissue, removing orbital fat, and expanding its bony structure, which was done in this case through a sphenoethmoidectomy. Although bone removal can be performed along any orbital wall, the inferomedial wall extends deeper into the apex and is the first-line approach for the decompression10.
In the reported case, the patient showed a complete recovery in visual acuity, visual fields, and optic disc edema after endoscopic bilateral concurrent orbital decompression.
If not diagnosed and treated early, DON can cause irreversible visual loss due to compressive injury of the optic nerve. It is crucial to evaluate all visual functions including visual field, color vision and contrast sensitivity, not only for diagnosis, but also to weight risks and benefits of the available treatment options. In the case described, visual function tests, fundus examination and optic nerve evaluation through the analysis of RNFL by SD-OCT were all essential in DON diagnosis, monitoring and surgical decision.
REFERENCES
1. McKeag D, Lane C, Lazarus J, Baldeschi L, Boboridis K, Dickinson A et al. Características clínicas da neuropatia óptica distireoidiana: uma pesquisa do Grupo Europeu de Orbitopatia de Graves (EUGOGO). Br J Oftalmol. 2006;91(4):455-8.
2. Saeed P, Tavakoli Rad S, Bisschop P. Disthyroid Optic Neuropathy. Cirurgia Oftálmica Plast Reconstr. 2018;34(4S):S60-S67.
3. Giaconi J, Kazim M, Rho T, Pfaff C. Evidências de tomografia computadorizada de neuropatia óptica distireoidiana. Cirurgia Oftálmica Plast Reconstr. 2002;18(3):177-82.
4. Tanda M, Piantanida E, Liparulo L, Veronesi G, Lai A, Sassi L et al. Prevalência e História Natural da Orbitopatia de Graves em uma Grande Série de Pacientes com Hipertireoidismo de Graves Recém-diagnosticado atendidos em um único centro. J Clin Endocrinol Metab. 2013;98(4):1443-1449.
5. Bahn R. Insights atuais sobre a patogênese da oftalmopatia de Graves. Horm Metab Res. 2015;47(10):773-778.
6. Jonathan D. Trobe; Joel S. Glaser; Pierre Laflamme. Perfil Clínico da Neuropatia Óptica Distireoidiana e Racional para o Gerenciamento. Arch Oftalmol . 1978;96(7):1199-1209.
7. Mourits M, van Kempen-Harteveld M, García M, Koppeschaar H, Tick L, Terwee C. Radioterapia para orbitopatia de Graves: estudo randomizado controlado por placebo. Lancet. 2000; 355(9214):1505-9.
8. Bartalena L , Baldeschi L , Dickinson A , Eckstein A , Kendall-Taylor P , Marcocci C , Mourits M , Perros P , Boboridis K , Boschi A , Currò N , Daumerie C , Kahaly GJ , Krassas GE , Lane CM , Lazarus JH , Marinò M , Nardi M , Neoh C , Orgiazzi J , Pearce S , Pinchera A , Pitz S , Salvi M , Sivelli P , Stahl M , V on Arx G , Wiersinga WM . Declaração de Consenso do Grupo Europeu de Orbitopatia de Graves (EUGOGO) sobre o manejo da OG. Eur Endocrinologia. 2008;158(3):273-85.
9. Currò N, Covelli D, Vannucchi G, Campi I, Pirola G, Simonetta S et al. Resultados terapêuticos de esteróides intravenosos de alta dose no tratamento da neuropatia óptica distireoidiana. Tireoide. 2014; 24(5):897-905.
10. Alexander D. Blandford, Dalia Zhang, Rao V. Chundury, Julian D. Perry. Neuropatia óptica distireoidiana: atualização sobre patogênese, diagnóstico e tratamento. Especialista Rev Oftalmol. 2017;12(2):111-21.
AUTHOR’S INFORMATION


Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 5, 2021.
Accepted on:
May 5, 2022.