Bianca Prado Patrús; Augusto Terra Baccega; Gustavo Lustosa Neves; Henrique Sampaio Ferreira; Marcelo Vicente de Andrade Sobrinho
DOI: 10.17545/eOftalmo/2021.0033
ABSTRACT
In this paper, we report a rare case of bilateral morning glory syndrome at Hospital da Pontifícia Universidade Católica de Campinas. This is a retrospective case. The patient was a 20-year-old man with bilateral morning glory syndrome and other midline changes. Herein, the main characteristics of this syndrome and the main differential diagnoses are discussed.
Keywords: Morning glory syndrome; Optic nerve; Midline changes.
RESUMO
O objetivo é reportar um raro caso de Síndrome de Morning glory bilateral no Hospital da Pontifícia Universidade Católica de Campinas. Este é um caso retrospectivo. Paciente de 20 anos com síndrome de Morning glory bilateral e outras alterações da linha média. Este caso discute as principais características da síndrome e os principais diagnósticos diferencias.
Palavras-chave: Síndrome de morning glory; Nervo optico; Alterações de linha média.
INTRODUCTION
Morning glory syndrome (MGS) or morning glory optic disc anomaly is a form of optic nerve dysplasia. This syndrome was first identified and named by Kindler in 19701. The name MGS is derived by the appearance of the optic nerve that resembles the plant species Ipomoea tricolor, a tropical flower popularly known as the morning glory. This anomaly is usually unilateral, with few cases of bilateral involvement reported in the literature. The syndrome presents a variety of symptoms, such as enlarged optic disc with a funnel-shaped excavation, retinal vessels in a radial pattern on the periphery of the excavation, glial hyperplasia filling the optic disc, and peripapillary pigmentary changes. The blood vessels of the retina are at the periphery of the excavation in a radial pattern. Women are twice as likely to have MGS as men. Peripapillary staphyloma and optic nerve coloboma are differential diagnoses of MGS. Absence of glial hyperplasia, peripapillary depigmentation, and vascular changes can differentiate optic nerve coloboma from MGS2.
It is believed that the pathophysiology of this syndrome is related to the lack of closure of the fetal fissure. Therefore, it could be a variant of optic nerve coloboma or a primary mesenchymal abnormality3.
Fei et al. believed that the abnormal tissue covering the optic disc in MGS is derived from the primitive hyaloid system4.
Common ocular associations of MGS are non-rhegmatogenous retinal detachment strabismus, congenital cataracts, primary vitreous persistence, eyelid hemangiomas, preretinal gliosis, crystalline colobomas, glaucoma, Duane syndrome, and hypertelorism4.
There is no definitive treatment for this pathology. The patient should be monitored for other pituitary disorders associated with midline malformations. The condition can be treated by refractive error correction, occlusion therapy for amblyopia treatment, retinal detachment monitoring, and the use of aids for low vision in cases of bilateral MGS. It is also important to explain to the patient and their family about the syndrome4.
A thorough PubMed survey revealed that only seven cases of bilateral presentation of MGS have been reported so far.
The objective of this paper is to report a case of a patient with MGS along with corpus callosum digenesis, hypertelorism, and cleft lip.
CASE REPORT
S.L.H, a 20-year-old male, visited the ophthalmology outpatient clinic at our hospital for low vision in the left eye since childhood. He was being monitored at the genetics outpatient clinic due to other defects at birth. He was reportedly diagnosed with dysgenesis of the corpus callosum. His surgical history includes a surgery to correct cleft lip at 3 months of age and another to correct divergent strabismus 9 years before the present visit. His family and gestational history presented nothing of note. His mother denies the use of drugs, alcohol, teratogenic substances, having infections during pregnancy, or consanguinity with the patient’s father.
The exam showed visual acuity of hand movements in the right eye and 20/40 in the left eye. Examination revealed hypertelorism, a scar in the nasolabial fold, esotropia of 15 prismatic diopters, and bilateral horizontal nystagmus with high frequency and low amplitude. Tonometry revealed an intraocular pressure of 12 mmHg in both eyes, and fundoscopy showed bilateral enlargement of the optic disc with central excavation, elevated pigmented edges from which the retinal vessels emerged (Figures 1 and 2), and an optic disc filled with glial tissue.
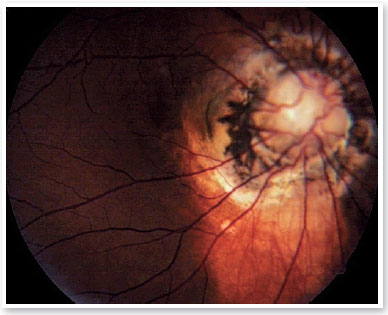

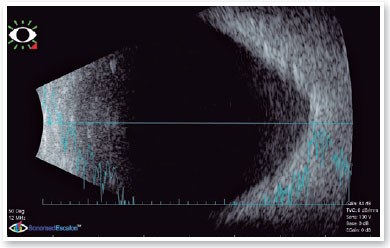
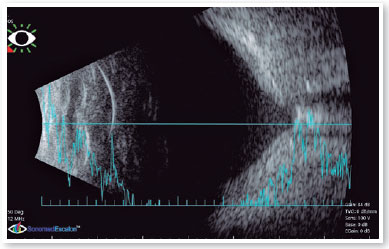
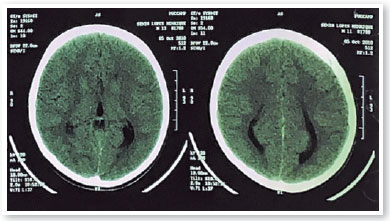
Ultrasound revealed increased funnel-shaped optic nerve excavation (Figures 3 and 4). Computed tomography of the skull showed parallel lateral ventricles, suggesting dysgenesis of the corpus callosum (Figure 5). Clinical and ultrasonographic findings confirmed the diagnosis of MGS.
DISCUSSION
After talking to the patient and answering questions about his condition, he was referred to the retina and strabismus outpatient clinic for follow-up.
MGS is associated with midline skull facial malformations, such as basal encephalocele, corpus callosum agenesis, absence of optic chiasm, hypertelorism, cleft lip, and cleft palatine6,7. In this case, the patient presented with cleft lip, hypertelorism, and dysgenesis of the corpus callosum, which confirms the association with facial malformations. In addition, GMS must be differentiated from nerve coloboma.
According to Bayer et al., bilateral involvement of MGS is marked by impaired moderate visual acuity, whereas in cases of unilateral involvement, visual acuity is highly compromised8.
This paper reports a rare case of bilateral MGS and confirms its relationship with midline skull facial malformations. We also present several clinical findings that will assist in the diagnosis of MGS and its differentiation from other optic nerve anomalies to allow for the correct diagnosis and prognosis.
REFERENCES
1. Kindler P. Morning glory syndrome: Unusual congenital optic disk anomaly. Am J Ophthalmol. 1970;69(3):376-9.
2. Deb N, Das R, Roy IS. Bilateral morning glory disc anomaly. Indian J Ophthalmol. 2003;51(2):182-3.
3. Cennamo G, Crecchio G, Iaccarino G, Forte R, Cennamo G. Evaluation of Morning Glory Syndrome with Spectral Optical Coherence Tomography and Echography. Ophthalmology. 2010;117(6):1269-73.
4. Fei P, Zhang Q, Li J, Zhao P. Clinical characteristics and treatment of 22 eyes of morning glory syndrome associated with persistent hyperplastic primary vitreous. Br J Ophthalmol. 2013;97(10):1262-7.
5. Dedhia CJ, Gogri PY, Rani PK. Rare bilateral presentation of morning glory disc anomaly. BMJ Case Rep. 2016 Aug 29;2016:bcr2016215846.
6. Leitch RJ, Winter RM. Midline craniofacial defects and morning glory disc anomaly. A distinct clinical entity. Acta Ophthalmol Scand Suppl. 1996;(219):16-9.
7. Görbe E, Vámos R, Rudas G, Jeager J, Harmath A, Csaba A, et al. Neuronal migration disorders, agenesis of corpus callosum, preauricular skin tag and bilateral morning glory syndrome in a term newborn infant. Clin Dysmorphol. 2008;17(2):123-5.
8. Beyer WB, Quencer RM, Osher RH. Morning Glory Syndrome: A Functional Analysis Including Fluorescein Angiography, Ultrasonography, and Computerized Tomography. Ophthalmology. 1982;89(12):1362-7.
AUTHOR’S INFORMATION
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
March 6, 2021.
Accepted on:
August 25, 2021.