Thiago Gonçalves dos Santos Martins1,2; Thomaz Goncalves dos Santos Martins3
DOI: 10.17545/eOftalmo/2021.0016
ABSTRACT
This article seeks to carry out a mini review on teaching models used for teaching students in the field of ophthalmology.
Keywords: Medical education; Ophthalmology; Models.
RESUMO
Esse artigo busca realizar uma pequena revisão sobre modelos de ensino utilizados para ensino de estudantes na área de oftalmologia.
Palavras-chave: Educação médica; Oftalmologia; Modelos.
INTRODUCTION
The teaching of ophthalmology has been reduced in the health curriculum. A survey carried out in Canada in 1996 found that more than half of the curricula of medical schools in the country did not have a required internship in ophthalmology1. Doctors have graduated without the most basic knowledge of ophthalmology due to the short time that medical schools have been dedicated to teaching this subject2. The same situation applies to nurses and other members of the eye team.
Long-lasting memories are formed by repetition, which leads to the formation of new synapses between neurons. Practice and repetition are necessary to ensure that these memory connections are permanent3,4. Thus, the development of teaching techniques that capture the attention of students and facilitate retention of knowledge by repetition should be valued. This can be achieved through the utilization of various teaching models.
Simulation has been part of medical training for a long time, as well as the use of cadavers for learning anatomy. Students should, therefore, practice their procedures before attending and operating patients, mainly due to the increase in legal repercussions for patient safety.
The ideal teaching model must meet the following requirements: obtain the student’s attention, inform the student of the main training objectives, stimulate the recall of previous learning, evaluate and provide feedback on their performance5.
This review is based on observing teaching models in the field of clinical and surgical training. We discussed models and learning as a continuous practice of maintaining the skill of the ophthalmologist.
Teaching Models
In education and training, the use of simulation allows students to experience a clinical situation close to reality but without real risk. Students can acquire a variety of skills, repeating clinical decision-making and procedures as many times as necessary until mastery is reached. This process allows students to develop at their own pace which personalizes learning and facilitates interaction between the teacher and student, allowing the teacher to have an immediate grasp of the level of knowledge acquired by the student. The training model performed with the Eyesi cataract surgical simulator helps ophthalmology students in training cataract surgery before being performed on humans. It allows students to practice both cataract and vitreoretinal surgery. A virtual image is created on the computer. The virtual image is projected on two oculars of the microscope, creating a binocular virtual image of the anterior segment. The image is also shown on an observer screen. The model calculates student performance by providing a score for each level based on five criteria: the achievement of the objective, efficiency, manipulation of instruments, handling of the microscope and treatment of tissues. The use of training models has been shown to increase surgeons’ skills and self-confidence. The cataract mannequin contains a model eye with eight possible entries that pivot and rotate when manipulated (Figure 1)6. The simulators are not only useful for the instruction and evaluation of surgical techniques, but also for simulating intraoperative decisions in situations of complications. Students who participate in cognitive skills training along with technical skills perform better than students who have only technical training7.

Another example of a hybrid simulation model for cataract surgery training was developed for the student to perform the surgery and train to place the intraocular lens8.
The use of training models began in the Roman era and is currently used in several fields of medicine including ophthalmology. There is the Human Eye Model which uses photos revealed in slides that are positioned in the posterior region of the eye of the human simulator, representing the retina9. Other training models use electronic photos of approximately at the bottom of the eye of a model, simulating pathologies for student training, as well as manikins for practicing the eye examination. These models allow the photos to be digitally altered by the teacher, who can simulate retinal pathologies for the student. The device can simulate the reduction in pupil size that occurs in direct ophthalmoscopy10.
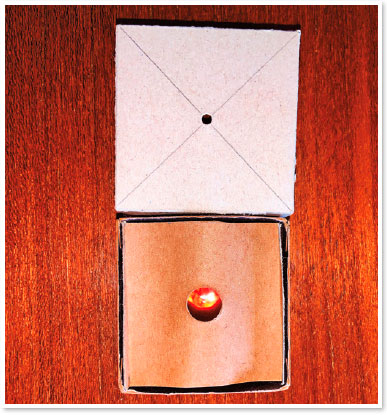
Other simulation models for training direct and indirect ophthalmoscopy exams in addition to Bruckner test training can be built by the student himself. Low-cost training models allow all students to have their model and carry out training whenever it is necessary to reinforce knowledge (Figures 2 and 3)11,12.

Eyesi can be used for indirect ophthalmoscopy training, minimizing training and discomfort for patients with exposure to examination light. The computer allows you to track the student’s skill progression and provide feedback13.
Videos can be used to record the surgeries and be discussed later with students to discuss strengths and weaknesses and focus on future steps for improvement. Videos can be combined with clinical case discussions5.
OASiS (Ophthalmic Anesthesia Simulation System) is a model for ophthalmic anesthesia training with high realism of the face and eye orbit structures. The model helps in the knowledge of ocular anatomy and allows safe procedures to be performed before the first anesthesia is given to patients reducing complications. OASiS consists of a mannequin that has anatomically accurate orbital and ocular structures with an integrated sensor to provide immediate feedback of the anesthesia performed. The model has no structure that simulates intraorbital vessels and its structures that simulate extraocular muscles are rigid. However, the model allows the detection of the entry of the needle into the orbital space and if the eyeball or extra-ocular muscles are reached with the needle14.
Youtube has become a platform for disseminating ophthalmic knowledge. In it, we can provide videos explaining the development of models. Other types of training involve the examination of corpses, animals, and enucleated eyes. But, the preservation of eyes must be adequate so that the cornea does not become opaque and prevent examination. It is difficult to get the right material for all student training. Also, there are ethical issues involved in the use of animals and corpses15,16.
Some more modern models adopt virtual reality, in which the student uses special glasses during training. The virtual reality simulator was initially used by military defense professionals. It has grown in popularity and has been incorporated in healthcare education. However, it is limited due to costs and special training for instructors.
The simulation can be complemented with the use of robotic surgery, where the doctor can send commands from miles away in minimally invasive procedures17.
Medical and nursing curricula containing classes that no longer use cadavers for teaching are becoming increasingly common, especially in developed countries. There are currently 11 medical schools that no longer use corpses in education, eight of which are located in Australia. Some colleges no longer use corpses to teach human anatomy and use simulators to save training with patients. However, the simulators still have a graphical limitation and some structures are better studied using cadavers. With learning using a simulator, many students can participate in simulated surgeries, complications and information sharing the study of anatomy with animals can have ethical problems and high costs. Virtual reality simulators are portable and generally cost less than animals and corpses18. Another alternative is the use of 3D printing for teaching anatomy, as with human bones. The bones are made of hard and monochromatic tissue, which makes them the easiest component of the human body to duplicate in 3D printing, with high levels of precision, preserving both visual and tactile values of real tissue. Besides that, there is a possibility that in the near future bioprinting will make it possible to print organs and other organic structures for study. The motivation for printing anatomical pieces is that it is an alternative for the use of cadavers in the teaching of anatomy in courses in the health area, since the maintenance of anatomical laboratories demands a high amount of resources19.
The use of simulators can help not only health professionals but visually impaired patients. The MoBIC Pre-Journey System (MoPS) allows the user to explore a world of virtual reality20.
Another solution for teaching anatomy has been the use of a 3D printer. The uses of 3D printing can be used in the manufacture of living tissues and organs; creation and customization of prostheses, implants, and anatomical models; and pharmaceutical use The printing of 3D models of organs, bones and even tumors already help doctors in planning more elaborate surgical approaches and diagnosis, complementing exams seen only in two dimensions. Also, 3D-printed can be used in medical education to explain complex procedures for students and even patients. The 3D printing allows the greater visualization and understanding of the anatomical part, making the procedures are carried out quickly and more accurately21.
Orbit surgeries have also been shown to be a procedure where 3D technology can provide great benefits. The computer program can create a copy of the contralateral orbit, using it as a model for the ipsilateral orbit to the lesion22.
We cannot focus our attention on ophthalmology education on outdated models. Our students today are immersed in a society so “colorful” and full of attractions that educators need to align their approaches to meet this changing student population. To facilitate long-term memory of ophthalmology knowledge, information needs to be repeated in many ways for it to be stored in various areas of the brain. This can be facilitated through various teaching models including virtual reality and 3D printing. The next steps for the future are the interaction of the health professional with the machine in real-time, the improvement of the quality of the digital image, and the storage of a large amount of data in interfaces that allow the interaction.
REFERENCES
1. Bellan L. Ensino de Oftalmologia na graduação no Canadá. Can J Ophthalmol. 1998;33(1):3-7.
2. Quillen DA, Harper RA, Haik BG. Ensino de Oftalmologia para estudantes de Medicina: Crises e oportunidades. Ophthalmology. 2005;112(11):1867-8.
3. Buckner RL, Kelley WM, Petersen SE. O córtex frontal contribui para a formação da memória humana. Nat Neurosci. 1999; 2(4):311-4.
4. Erk S, Kiefer M, Grothe J, Wunderlich AP, Spitzer M, Walter H. O contexto emocional modula o efeito de memória subsequente. Neuroimage. 2003;18(2):439-47.
5. Lorch AC, Kloek CE. Uma abordagem baseada em evidências para o ensino cirúrgico em Oftalmologia. Surv Ophthalmol. 2017; 62(3):371-7.
6. Bisol T, Rezende RA, Rezende F. Eficácia do treinamento com o simulador cirúrgico Eyesi na melhoria do desempenho de cápsulas de alta tensão na capsulorrexe. Rev Bras Oftalmol. 2016;75(5):376-9.
7. Kohls-Gatzoulis J, Regehr G, Hutchinson C. Ensinar habilidades cognitivas melhora o aprendizado em cursos de habilidades cirúrgicas: um estudo cego, prospectivo e randomizado. Can J Surg. 2004;47(4):277-83.
8. Shen X, Zhou J, Hamam A, Nourian S, El-Far NR, Malric F, Georganas ND. Simulação de cirurgia com telementoria habilitada com háptica. IEEE MultiMedia. 2008;15(1):64-76.
9. Issenberg SB, McGahlie WC, Petrusa ER, Gordon DL, Scalese RJ. Recursos e usos de simulações médicas de alta fidelidade que levam a um aprendizado eficaz: Uma revisão sistemática pela BEME. Med Teach. 2005;27(1):10-28.
10. Pao KY, Uhler TA, Jaeger EA. Criando o THELMA - The Human Eye Learning Model Assistant (o Assistente de Simulação de Aprendizado sobre o Olho Humano). J Acad Oftalmol. 2008; 1(1):25-9.
11. Martins TGS, Costa ALFA, Martins RV, Schor P. Um modelo de ensino para o teste de Brückner: Melhorando a triagem para catarata congênita. Insight. 2017;42(1):33-4.
12. Martins TG, Costa ALF, Helene O, Martins RV, Helene AF, Schor P. Treinamento de oftalmoscopia direta usando simuladores. Clin Teach. 2017;14(6):423-6.
13. Chou J, Kosowsky T, Payal AR, Gonzalez Gonzalez LA, Daly MK. Validade de construto e de face do simulador de oftalmoscopia indireta Eyesi. Retina. 2017;37(10):1967-76.
14. Mukherjee B, Venkatakrishnan JV, George B, Sivaprakasam M. Avaliação de um sistema de simulação de anestesia oftalmológica para treinamento em bloqueios regionais. Ophthalmology. 2015; 122(12):2578-80.
15. Amberg R, Pollak S. Endoscopia post-mortem do fundo ocular: Uma ferramenta valiosa na prática forense post-mortem. Forensic Sci Int. 2001;124(2-3):157-62.
16. Borgersen NJ, Henriksen MJV, Konge L, Sørensen TL, Thomsen ASS, Subhi Y. Oftalmoscopia direta no YouTube: Análise do conteúdo de vídeos instrucionais do YouTube e abordagem da visualização. Clin Ophthalmol. 2016;10:1535-41.
17. Suzuki S, Suzuki N, Hattori A, Hayashibe M, Konishi K, Kakeji Y, et al. Simulação de telecirurgia com simulador de órgãos do paciente para treinamento em cirurgia robótica. Int J Med Robot. 2005;1(4):80-8.
18. Reznick RK, MacRae H. Ensinando Habilidades Cirúrgicas - Mudanças de Direção. N Engl J Med. 2006;355(25):2664-9.
19. Negi S, Dhiman S, Sharma RK. Noções básicas e aplicações de simulações médicas de prototipagem rápida. Rapid Prototyp J. 2014;20(3):256-67.
20. Rodrigues CEM. Um dispositivo háptico de auxílio à navegação para deficientes visuais [trabalho de conclusão de curso]. 2006. Recife: Centro de Informática da Universidade Federal de Pernambuco.
21. Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Avaliação da impressão 3D e seu potencial impacto na Biotecnologia e nas Ciências Químicas. Am Chem. 2014;86(7):3240-53.
22. Choi JW, Namkug K. Aplicação clínica da tecnologia de impressão tridimensional na cirurgia plástica craniofacial. Arch Plastic Surg. 2015;42(3):267-77.
AUTHOR’S INFORMATION

Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
August 10, 2020.
Accepted on:
December 21, 2020.