Eduardo Cunha de Souza1; Milton Ruiz Alves2
DOI: 10.17545/e-oftalmo.cbo/2017.78
ABSTRACT
A 40y-old white woman, with controlled type 1 diabetes, presented with transient “no light perception vision” in her right eye immediately following uncomplicated cataract surgery. She had vitrectomy for diabetic retinal detachment years ago. The use of intracameral unpreserved lidocaine in a vitrectomized eye may have facilitated the posterior diffusion of the drug in this case. Patient full recovery of vision suggests the relative lack of retinal toxicity of lidocaine in small intracameral concentrations.
Keywords: Cataract; Visual Perception; Diabetes Mellitus Type 1; Vitrectomy
RESUMO
Mulher branca de 40 anos, com diabetes tipo 1 controlado, apresentou perda visual de percepção luminosa no olho direito, imediatamente após cirurgia de catarata sem complicações. A paciente havia se submetido a uma vitrectomia 10 anos antes, devido a um descolamento de retina causado pelo diabetes. O uso de lidocaína intracameral sem conservantes em um olho vitrectomizado pode ter facilitado a difusão posterior do medicamento neste caso. A completa recuperação da visão da paciente sugere uma relativa ausência de toxicidade retiniana da lidocaína em pequenas concentrações intracamerais.
Palavras-chave: Catarata; Percepção visual; Diabetes Mellitus Type 1; Vitrectomia
INTRODUCTION
Intracameral lidocaine is often used to augment topical anesthesia during ocular surgery. Although intracameral lidocaine is believed to be safe for the cornea and anterior chamber1, concerns persist regarding the possible toxic effects of lidocaine in retina. We describe a case of a rare complication with intracameral lidocaine.
Case Report
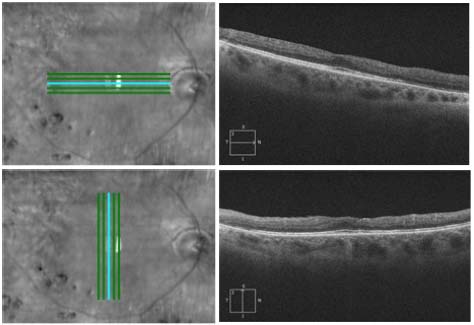
A 40 year-old white woman, with controlled type 1 diabetes, presented with “no light perception vision” in her right eye immediately following uncomplicated cataract surgery. Her past ocular history was remarkable for pars plana vitrectomy for proliferative diabetic retinopathy in this eye 10 years previously. Her best corrected visual acuity prior to cataract surgery was 20/70 due to advanced nuclear sclerosis. Posterior segment evaluation showed a controlled panphotocoagulated retina and a normal macular OCTFigure 1. The cataract surgery was performed via phacoemulsification using intravenous sedation and topical anesthesia supplemented with intracameral non-preserved lidocaine (Xylestesin 1%). Due to her unexpected complaints of no light perception, an urgent retinal consultation was obtained and the patient was examined approximately 45 minutes following the procedure. Her visual acuity was confirmed to be no lightperception to the highest setting on the indirect ophthalmoscope. She denied pain or any type of discomfort in the eye. Digital ocular tension was normal. Examination of the anterior and posterior segment of the eye did not show any abnormalities. Specifically, there was no disc edema or pallor and the retina appeared normal. The retinal blood vessels showed normal caliber and course and no embolus was seenFigure 2. Approximately 90 minutes after the surgery, patient started to recover perception of light. During the following hours, she progressively recovered her full visual field, slowly starting from the temporal side towards the central and nasal areas. The following day, the vision measured 20/25 in the operated eye.
DISCUSSION
Current anesthesia for phacoemulsification surgeryis often obtained with topical lidocaine occasionally supplemented with intracameral unpreserved lidocaine injected into the anterior chamber to decrease pain during surgical manipulation. It is believed that the lidocaine injected in the anterior chamberdoes not reach the retinal tissue or the optic nerve in a high enough concentration in most eyes undergoing cataract surgery, due to the physiologic barrier effect of the lens capsule, zonules and vitreous. However, in this present case, the previous vitrectomy may have altered these structures, facilitating the diffusion of the drug posteriorly during the surgery. In 1997, Hoffman and Fine2 reported a similar case of transient complete visual loss after the use of intracameral unpreserved lidocaine to repair a traumatic corneal graft dehiscence. They believed the mechanism of transitory visual loss was total anesthesia of the retinal nerve fiber layer at or near the optic nerve. In 1998, Gills et al3 reported amaurosis in four patients following the use of intracameral lidocaine, and in each case, the posterior capsule was no intact, All four patients recovered completely within hours. In 2009, Falzon et al4 reported a case of transient, complete loss of vision following phacoemulsification with an intracameral ophthalmic viscosurgical device (OVD) and lidocaine solution complicated by posterior capsule rupture, with improved to 20/80 after one day and 20/25 in one week. In 2014, Gupta and Kumar5 reported a case of temporary complete vision loss after intracameral lignocaine in a post-vitrectomy eye. In 2015, Eshraghi et al6 reported a case of transient complete visual loss after intracameral lidocaine following posterior polar cataract surgery with posterior polar cataract surgery with posterior capsular rupture. As it was observed in these reported cases and the present case, the resulted fullrecovery of vision suggests the relative lack of retinal toxicity of unpreserved lidocaine in small intracameral concentrations. This case illustrates the possible brief visual effects of intracameral lidocaine. Recognition of such cases allows physiciansto reassure the patient visual function should return to normal after a few hours of observation.
FIGURES

REFERENCES
1. Ezra DG, Allan BDS. Topical anaesthesia alone versus topical with intracameral lidocaine for phacoemulsification [review]. Cochrane Database Syst Rev. 2007;(3):CD005276. http://dx.doi.org/10.1002/14651858.CD005276.pub2
2. Hoffmann RS, Fine H. Transient no light perception acuity after intracameral lidocaine injection. J Cataract Surg. 1997;23:957-8. http://dx.doi.org/10.1016/S0886-3350(97)80261-1
3. Gills JP, Johnson DE, Cherchio M, Raanan MG. Intraocular anesthesia. Ophthalmol Clin North Am. 1998;11:65-71
4. Falzon K, Guerin MB, Tim F. Transient, complete loss of vision secondary to posterior diffusion of an ophthalmic viscosurgical device-lidocaine solution during complicated phacoemulsification. J Cataract Refract Surg. 2009;35(8):1472-3. http://dx.doi.org/10.1016/j.jcrs.2009.04.024
5. Gupta SK, Kumar A. temporary complete vision loss after intracameral lignocaine in a post-vitrectomy eye: a single casereport. Egypt Retina J. 2014;2:83-5. http://dx.doi.org/10.4103/2347-5617.158226
6. Eshraghi B, Katoozpour R, Anvari P. Transient complete visual loss after intracameral anesthetic injection in cataract surgery. J Curr Ophthalmol. 2015;27(3-4):129-31. http://dx.doi.org/10.1016/j.joco.2015.12.005
Funding source: None
Conflicts of interest: None
Received on:
December 16, 2016.
Reviewed in:
March 31, 2017.
Accepted on:
December 16, 2016.