Abrahão da Rocha Lucena
DOI: 10.17545/e-oftalmo.cbo/2017.93
ABSTRACT
Advancements in cataract surgery and intraocular lens (IOL) design have improved the quality of vision for patients subjected to cataract surgery. For the measurement of IOLs, the topographer can provide simulated keratometry, a parameter that simulates the keratometry of the automated refractor. In cases of corneal irregularities, the topography of semimeridians is used, disregarding the keratometric measurements of the ectatic area. Therefore, the measure of convergence of IOL will not be underestimated because the average keratometry obtained will be lower, avoiding the effect of postoperative hypermetropization. Corneal topography allows the quantitative determination of astigmatism and its classification into regular (symmetric and asymmetric) and irregular, guiding the cataract surgeon for the implantation of monofocal, multifocal, toric, or multifocal toric IOLs. Moreover, topography guides the surgeon while performing a corneal incision in the most curved axis to reduce postoperative astigmatism and allows the assessment of changes generated by corneal incision after cataract surgery. Therefore, topography has assumed an importantrole in surgical planning and preventing undesirable outcomes. This study presents the various applications of corneal topography in cataract surgery.
Keywords: Corneal Topography; Surgery; Cataract
RESUMO
A evolução técnica na cirurgia de catarata e o aperfeiçoamento no desenho das lentes intraoculares trouxeram melhorias na qualidade da visão dos indivíduos submetidos à facectomia. Na medida da lente intraocular (LIO) o topógrafo pode fornecer a ceratometria simulada ou SIMK, parâmetro que simula a ceratometria do autorrefrator. Quando há irregularidades na córnea, utiliza-se o recurso topográfico de semimeridianos, desconsiderando as medidas ceratométricas da área ectásica; com isso a medida da vergência da LIO não será hipoestimada, pois a ceratometria média fornecida será menor, evitando-se efeito de hipermetropização no pós-operatório. Através da topografia corneana, a determinação quantitativa do astigmatismo e sua separação em regular (simétrico e assimétrico) e irregular orienta o cirurgião de catarata na indicação do implante das lentes monofocal, multifocal, tórica, ou multifocal tórica. A topografia orienta também o cirurgião na realização da incisão corneana no eixo mais curvo com intuito de diminuir o astigmatismo no pós-operatório. As modificações geradas pela incisão corneana após a facectomia podem ser avaliadas no pós-operatório através da topografia. Portanto, a topografia vem assumindo papel importante no planejamento cirúrgico prevenindo surpresas desagradáveis. Neste artigo são apresentadas as diversas formas de utilização da topografia corneana na cirurgia de catarata.
Palavras-chave: Topografia da Córnea; Cirurgia; Catarata
INTRODUCTION
Advancements in cataract surgery and intraocular lens (IOL) design have improved the quality of vision for patients subjected to cataract surgery. Topography has assumed an important role in surgical planning and preventing undesirable outcomes.
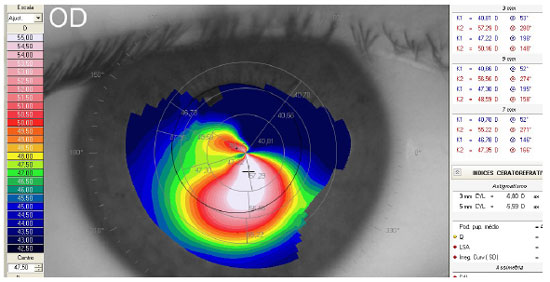
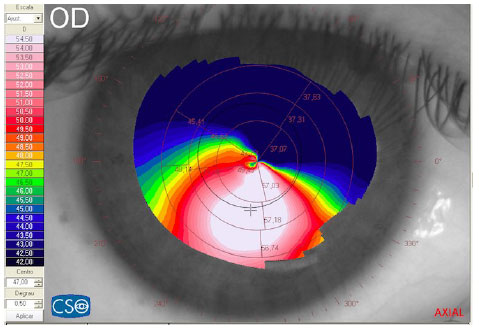
1. Measurement of IOL
For the measurement of IOL, the topographer can provide simulated keratometry, a parameter that simulates the keratometry of the automated refractor. Another use of topography in the measurement of IOL is in cases of corneal irregularities. In these cases,the surgeon can conduct a topographical analysis of the semimeridians (Figure 1), disregarding the keratometric measurements of the ectatic area. Therefore, the degree of convergence of IOL will not be underestimated because the average keratometry provided will be smaller, thereby avoiding the effect of postoperative hypermetropization1,2,3.
2. Diagnosis of corneal astigmatism
Corneal topography allows the quantitative determination of astigmatism and its classification into regular and irregular, guidingthe cataract surgeon for the implantation of monofocal, multifocal, toric, or multifocal toric IOLs. Moreover, topography can guide the main incision of cataract surgery in the most curved corneal axis to reduce postoperative astigmatism4. and can assess the changes generated by corneal incision after cataract surgery5.
The topographic pattern of the corneal surface allows the classification of the type and degree of astigmatism, when present. In the absence of significant astigmatism, the cornea is considered to have a spherical or oval topographic pattern6.
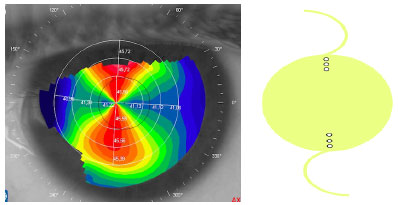
Regular astigmatism occurs in cases in which the most planar and most curved corneal meridians form an angle of 90° with each other. Regular astigmatism is subdivided into symmetrical (Figure 2) and asymmetrical (Figures 3 and 4). The classification of symmetry is possible when the difference between the equidistant points of the most curved or most planar hemimeridians is smaller than 1.0 D. Stigmatism is asymmetrical in cases in which this difference exceeds 1.0 D6,7,8,9.
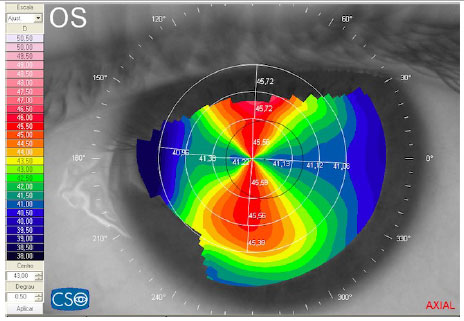
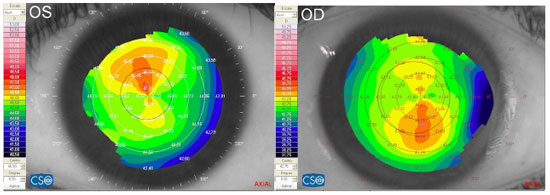
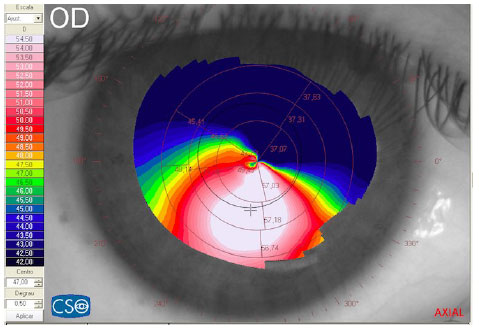
The classification of irregularity is possible in cases in which the most curved and most planar meridians lose orthogonality. Some classifications of irregularity are presented in the literature10,11. Visual classification can be achieved by observing the local increase in the curvature, with the subsequent loss (amputation) of the corresponding bow-tie image on the opposite hemimeridian (Figure 5).
3. Identifying the corneal asphericity coefficient (Q)
The cornea and IOL are involved in image formation in the retina. Advancements in IOL design have allowed the customization of the implant according to the corneal pattern. Therefore, the study of the corneal surface by topography is critical because this technique allows the diagnosis of irregularities on the corneal surface and the determination of Q, which is the rate of change in the curvature of a lens as we move away from the center12. The calculation of Q allows the determination of the longitudinal spherical aberration (LSA) generated by the cornea, and this optical phenomenon occurs when the corneal wavefront tangentially reaches the periphery of a spherical lens,increasing its convergence effect and producing a second focus (positive LSA) anterior to the main focus (Figure 6)12,13.
Therefore, the physician plans the implantation of the lens according to LSA of each manufacturer. LSA of the lens is given in microns, and thus the corneal LSA determined by topography should also be in microns. IOLs can have a positive LSA, as is the case of spherical lenses14, or neutral or negative LSA, as is the case of aspherical IOLs15.
4. Corneal topography versus monofocal and multifocal IOLs
The implantation of monofocalIOLs is usually indicated in cases in which the degree of astigmatism is less than or equal to 1.0 D. Refractive astigmatism should be considered because it may contain a residual crystalline component, leading to misinterpretations of the actual corneal astigmatism16.
The use of multifocal and monofocal IOLs is also indicated for the same degree of astigmatism. In these cases, the level of astigmatism and the magnitude of corneal LSA should be considered (Figure 6). The extent of LSA and pupil size may enhance the visualization of halos, which occur with multifocal IOLs because of diffraction, resulting in lower contrast sensitivity and glare15. Another relevant consideration is to avoid theimplantation of multifocal IOLs in cases in which an irregular topographic pattern is identified16.
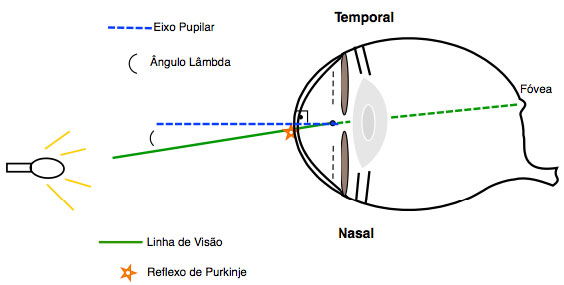
5. Importance of the lambda angle
The indication of implantation of multifocal IOLs is also based on the size of the lambda angle of each eye (Figure 7). Topography calculates the lambda angle by measuring the distance between the center of the pupil and the Purkinje reflection (corneal apex or center of the inner ring of the Placido disk). The presence of the Purkinje reflex shifted nasally is caused by the compensation to the temporal position of the macula. The aberrations generated by the nasal displacement of the corneal vertex relative to the pupillary axis are naturally neutralized by the lens. After cataract surgery, this neutralization is broken and corneal wavefront aberration, generated bya high lambda angle (greater than 0.2 mm), can reach the multifocal IOL and reduce the quality of vision17,18,19,20.
6. Corneal topography in the implantation of toric IOLs
Toric IOLs are usually indicated in cases in which astigmatism is more than 1.0 D. The presence of residual crystalline astigmatism should be investigated21, and its presence is suspected in cases in which topographic astigmatism does not match refractive astigmatism22. The determination of the degree of astigmatism is followed by the location of its axis, and these data are fed into the toric IOL calculators for the development of the lenses. The implantation of IOLs should follow the axis indicated by the calculator of each manufacturer, and these values may deviate a little from those found in corneal topography because of the positioning of the main corneal incision used by the surgeon (Figure 8).
The identification of an irregular topographic pattern should alert the surgeon about the contraindication of the implantation of toric IOLs.
Furthermore, the degree and location of astigmatism on the posterior surface of the cornea should be considered. Placido-disk corneal topography does not evaluate the posterior surface of the cornea. Previous studies suggest that the toricity of IOL should be calculated considering a decrease of 0.5 D in the toricity value in cases of with-the-rule astigmatism and an increase of 0.3 D in cases of against-the-rule astigmatism. Although the difference is small, it is important to follow this approach, especially in cases of astigmatism of small magnitude, because of the effects of proportionality. A better strategy is the calculation of the total refractive power of the cornea using the Scheimpflug method, in which the degree of astigmatism is determined in the anterior and posterior surface of the cornea with its final vector result23,24,25.
7. Relaxing incisions (RIs)
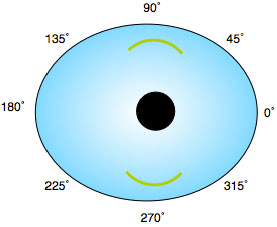
The identification of the degree and axis of astigmatism is the main step in the planning of corneal or limbalRIs for the correction of astigmatism after cataract surgery4. Corneal topography becomes a valuable tool for the execution of RIs. The procedure can be performed with a diamond scalpel and a micron caliper or femtosecond laser26.
RIs are classified into limbal and corneal (Figure 9).Limbal RIs are easier to execute, less dependent on pachymetry, and less susceptible to overcorrections and have faster stabilization and better postoperative corneal topography; it is used in degrees of astigmatism smaller than 3 D. The disadvantage is the larger size of the incision, typically 1–3 hours in arc length. In contrast, corneal RIs have a greater capacity of correction with smaller incisions but are more uncomfortable, have increased risk of perforation (pachymetry-dependent), and can cause overcorrections and irregular astigmatism27,28.
With-the-rule and against-the-rule astigmatisms are better tolerated than oblique astigmatism. Individuals with hyperopic astigmatism do not benefit because the spherical equivalents are not relatively affected. Therefore, it is indicated for spherical and planar-spherical equivalents of myopia in cases of high astigmatism, with the distortion of peripheral vision by glasses28.
The greatest challenge of RIs is planning the degree and location of astigmatism to be corrected. In the case of orthogonal astigmatism, refraction can help because it produces a combination ofcorneal and crystalline astigmatism. The topographic axis should be followed in cases in which the meridians are not perfectly orthogonal27,28.
REFERENCES
1. Borzog S, Pineda R. Cataract and keratoconus: minimizing complications in Intraocular lens calculations. Seminar Ophthalmol. 2014;29(5-6):376-9. http://dx.doi.org/10.3109/08820538.2014.959193
2. Bourges JL. Cataract surgery in keratoconus with irregular astigmatism. In: Goggin M, editor. Astigmatism-optics, physiology and management. Croatia: InTech; 2012. p.93-103. http://dx.doi.org/10.5772/20522
3. Watson MP, Anand S, Bhogal M, Gore D, Moriyama A, Pullum K. Cataract surgery outcome in eyes with keratoconus. Br J Ophthalmol. 2014; 98(3):361-4. http://dx.doi.org/10.1136/bjophthalmol-2013-303829
4. Watson MP, Anand S, Bhogal M, Gore D, Moriyama A, Pullum K. Cataract surgery outcome in eyes with keratoconus. Br J Ophthalmol. 2014; 98(3):361-4. http://dx.doi.org/10.1136/bjophthalmol-2013-303829
5. Gross RH, Miller KM. Corneal astigmatism after phacoemulsification and lens implantation through unsutured scleral and corneal tunnel incisions. Am J Ophthalmol. 1996;121(1):57-64. http://dx.doi.org/10.1016/S0002-9394(14)70534-3
6. Bogan SJ, Waring GO, Ibrahim O, Drews C, Curtis L. Classification of normal corneal topography based on computer-assisted videokeratography. Arch Opthalmol. 1990;108(7):945-9. http://dx.doi.org/10.1001/archopht.1990.01070090047037
7. Polisuk P. Topografia da córnea: atlas clínico. 4ª ed. Rio de Janeiro: Cultura Médica; 2015.
8. Klyce SD. Computer-Assisted corneal topography. High-resolution graphic presentation and analysis or keratoscopy. Invest Ophthalmol Vis Sci. 1984;25(12):1426-35. Disponível em: http://iovs.arvojournals.org/article.aspx?articleid=2176858
9. Koch DD, Foulks GN, Moran CT, Wakil JS. The corneal EyeSys sistem: accuracy analysis and reproducibility of firt generation prototypy. J Refract Surg. 1989;5(6):424-9. http://dx.doi.org/10.3928/1081-597X-19891101-14
10. Rabinowith YS. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11(5):371-406.
11. Maeda N, Klyce SD, Smolek MK. Neural network classification of corneal topography. Preliminary demonstration. Invest Ophthalmol Vis Sci. 1995; 36(7):1327-35. Disponível em: http://iovs.arvojournals.org/article.aspx?articleid=2161494
12. FRANCO, SMB. Determinação óptica da estrutura tridimensional da córnea [tese de doutorado]. Portugal: Universidade do Minho, 2005 [acesso em 2017 Mar 14]. Disponível em: http://repositorium.sdum.uminho.pt/bitstream/1822/4574/3/Sandra%20Franco.pdf
13. GlasserA, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision Res. 1998;38(2):209-29. http://dx.doi.org/10.1016/S0042-6989(97)00102-8
14. Miller JM, Anwaruddin R, Straub J, Schwiegerling J. Higher order aberrations in normal, dilated, intraocular lens, and laser in situ keratomileusis corneas. J Refract Surg. 2002;18(5):S579-83. http://dx.doi.org/10.3928/1081-597X-20020901-16
15. Caporossi I, Martone G, Casprini F, Rapisarda L. Prospective randomized study of clinical performance of 3 aspheric and 2 spherical intraocular lenses in 250 eys. J Refract Surg. 2007;23(7):639-48. http://dx.doi.org/10.3928/1081-597X-20070901-02
16. Hayashi K, Manabe S, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2010;36(8):1323-9. http://dx.doi.org/10.1016/j.jcrs.2010.02.016
17. Uozato H, Guyton DL. Centering corneal surgical procedures. Am J Ophthalmol 1987;103:264-75. Disponível em: https://www.researchgate.net/profile/David_Guyton/publication/19336170_Centering_corneal_surgical_procedures/links/00463518861bd02117000000/Centering-corneal-surgical-procedures.pdf
18. Tabernero J, Benito A, Alcon E, Artal P. Mechanism of compensation of aberrations in the human eye. J Opt Soc Am A. 2007;24(10):3274-83. https://doi.org/10.1364/JOSAA.24.003274
19. Braaf B, Watering TCV, Spruijt K, Heijde RGLV, Sicam VADP. Calculating angle lambda (λ) using zernike tilt measurements in specular reflection corneal topography. J Optom. 2009;2(4):207-14. http://dx.doi.org/10.3921/joptom.2009.207
20. Mandell RB. Locating the corneal sighting center from videokeratography. J Refract Surg. 1995;11(4):253-310. http://dx.doi.org/10.3921/joptom.2009.207http://dx.doi.org/10.3921/joptom.2009.207
21. Marques A, Portelinha J, Isidro F, Simões P, Ferreira T. Análise do astigmatismo corneano nos candidatos a cirurgia de catarata. Oftalmologia. 2015;39(1):23-29. Disponível em: http://revistas.rcaap.pt/index.php/oftalmologia/article/view/6876/5506
22. Ernest P, Potvin R. Effects of preoperative corneal astigmatism orientation on results with a low-cylinder-power toric intraocular lens. J Cataract Refract Surg. 2011;37(4):727-32. http://dx.doi.org/10.1016/j.jcrs.2010.11.026
23. Koch DD, Jenkins RB, Weikert MP, Yeu E, Wang L. Correcting astigmatism with toric intraocular lenses: effect of posterior corneal astigmatism. J Cataract Refract Surg. 2013;39(12):1803-9. http://dx.doi.org/10.1016/j.jcrs.2013.06.027
24. Savini G, Versaci F, Vestri G, Ducoli P, Næser K. Influence of posterior corneal astigmatism on total corneal astigmatism in eyes with moderate to high astigmatism. J Cataract Refract Surg. 2014;40(10):1645-53. http://dx.doi.org/10.1016/j.jcrs.2014.01.046
25. Savini G, Naeser K. An analysis of the factor influencing the residual refractive astigmatism after cataract surgery with toricintraocular lenses. Invest Ophthalmol Vis Sci. 2015;56(2):827-35. http://dx.doi.org/10.1167/iovs.14-15903
26. Abbey A, Ide T, Kymionis GD, Yoo SH. Femtosecond laser-assisted astigmatic keratotomy in naturally occurring high astigmatism. Br J Ophthalmol. 2009; 93(12):1566-9-. http://dx.doi.org/10.1136/bjo.2008.149971
27. Kwitko S, Belfort Jr R. Correção cirúrgica do astigmatismo. In: Belfort Jr. R, Kara-José N, editores. Córnea clínica cirúrgica. São Paulo: Roca; 1996. p. 559-73.
28. Carvalho MJ, Suzuki SH, Freitas LL, Branco BC, Schor P, Lima ALH. Limbal relaxing incisions to correct corneal astigmatism during phacoemulsification. J Refract Surg. 2007;23(5):499-504. http://dx.doi.org/10.3928/1081-597X-20070501-14
Funding source: None
Conflicts of interest: None
Received on:
February 27, 2017.
Reviewed in:
March 31, 2017.
Accepted on:
March 9, 2017.