Hugo Coelho Carvalho Sousa; Paula de Castro Pedroza; Rafael de Paiva Oliveira; Waleska Cecilia Costa de Oliveira Alcoforado; Felipe Crozara Ferreira de Oliveira; Fabrício Tadeu Borges; Kátia Delalibera Pacheco; Marcos Ávila
DOI: 10.17545/eOftalmo/2020.0003
ABSTRACT
INTRODUCTION: The capture of peripheral retinal images has gradually become increasingly important for the diagnosis and treatment of diseases. Some types of peripheral degeneration are important because they are risk factors for retinal detachment.
OBJECTIVE: We aimed to assess the sensitivity of wide-field retinal imaging using indirect binocular ophthalmoscopy.
METHOD: A prospective study was conducted including patients presenting with lesions predisposed to retinal detachment who were examined using binocular indirect ophthalmoscopy with scleral indentation. All patients were referred for wide-field retinal imaging. We compared the lesions found using the equipment (groups A and B) with the diagnoses obtained using BIO (sample group).
RESULTS: On analyzing the images from group A (photographs of the 4 quadrants), 122 lesions of the 143 found in the sample group were identified, resulting in 85.31% sensitivity. When a single central photograph was taken (group B), 96 lesions of 158 found in the sample group were located, resulting in 60.76% sensitivity.
CONCLUSION: When examining peripheral lesions, it is recommended to assess at least 4 photographs in positions preset by the equipment (superior, nasal, inferior, and temporal).
Keywords: Ophthalmic diagnostic techniques; Retina; Eye health services.
RESUMO
INTRODUÇÃO: A captura de imagens retinianas periféricas se tornou cada vez mais importante para o diagnóstico e tratamento de doenças ao longo dos anos. Algumas degenerações periféricas são importantes por serem fatores de risco para descolamento de retina.
OBJETIVO: Avaliar a sensibilidade da retinografia de grande angular com a oftalmoscopia binocular indireta.
MÉTODO: Estudo prospectivo que incluiu pacientes examinados com a oftalmoscopia binocular indireta com indentação escleral que apresentaram lesões predisponentes ao descolamento de retina. Todos os pacientes foram encaminhados para realizar retinografia de grande angular. Comparamos as lesões encontradas no aparelho, Grupos A e B, com as diagnósticas pela OBI, Grupo Amostral.
RESULTADOS: Ao analisar as imagens do Grupo A (foto dos 4 quadrantes) identificaram 122 lesões de 143 encontradas no Grupo Amostral, com sensibilidade de 85,31%. Quando realizado foto única central, Grupo B, foram localizadas 96 lesões de 158 definindo sensibilidade de 60,76%.
CONCLUSÃO: Ao pesquisar lesões periféricas é recomendado a realização de no mínimo 4 fotos com uma posição pré-estabelecida pelo aparelho (superior, nasal, inferior e temporal).
Palavras-chave: Técnicas de diagnóstico oftalmológico; Retina; Serviços de saúde ocular.
INTRODUCTION
The first retinal image was obtained in the year 1886. Since then, there has been significant progress in the capturing method and image quality. From its inception, the main retinal imaging techniques were able to capture the posterior pole, macula, and optic disc(1). In the late 1990s, digital equipment was developed that enabled photomontage by capturing mid-periphery images, thereby expanding the observation area using specific software(2). In the past 40 years, varied techniques for grouping several images have been developed, which enable the observation of 100°-160° of the retina in a single grouped image. The first single image wide-field system was developed in 1975 by Oleg Pomerantzeff when it became possible to document up to 148° between the central and peripheral retina using a lens system in contact with the cornea(2).
Recently, devices that capture a single image without the need for contact with the cornea have appeared, among which are Optos® Optomap, Heidelberg Spectralis® HRA Ultra-Widefield, and Clarus® Zeiss(3). Optomap is capable of capturing high-resolution fundus images and enabling observation of approximately 200° of retinal perimeter, thereby comprising 82% of its extension(3-6). Its new generation upgrade-Optomap 200DTx-uses red, green, blue, and infrared lights; image acquisition time is approximately 0.3 s(4,7). It has a wide visualization capacity due to the ellipsoidal mirror, which is a new technology that does not require direct contact with the eyeball(1,2).
Capturing peripheral retinal images has gradually become increasingly important for the diagnosis and treatment of diseases in cases such as pre- and postoperative care for vitreoretinal surgery, hereditary conditions, ischemic proliferative vascular diseases, peripheral degenerations, inflammatory diseases, and neoplasms(1).
Some peripheral degenerations, including lattice degeneration, tears, atrophic holes, vitreoretinal traction, and dialysis, are important because they are risk factors for retinal detachment (RD). Early detection of these lesions is of great importance for the potential effective treatment and prevention of RD(4). Currently, the gold standard examination to assess the peripheral retina is binocular indirect ophthalmoscopy (BIO) with scleral indentation(7).
With the increasing use of this technology in several countries and because it is a rapid, practical examination without the need for dilating eye drops, technologies using wide-field imaging have been used as screening method for peripheral retinal lesions predisposed to RD. However, the extent of the periphery that should be viewed to achieve a diagnosis and the efficacy of the method are unclear(6). The present study aims to assess the sensitivity of Optomap 200DTx and compare the two capturing modes of the device with regard to the detection of peripheral retinal lesions previously detected using the gold standard method BIO with scleral indentation.
METHOD
This prospective study was conducted in the retinal examination department at Centro Brasileiro da Visão (CBV) and approved by the ethics committee of Fundação de Ensino e Pesquisa em Ciências da Saúde (CAAE protocol number 13237919.3.0000.5553). All technicians and physicians involved have previously been familiarized with the use of Optomap for 20 months from November 2017.
Patients considered for the study were aged >16 years, consecutively treated from August to October 2019, and had at least one of the following conditions: complaints of eye floaters or flashes up to 60 days before the appointment, short-sightedness, history of RD in one eye, and family history of first-degree relatives with RD. An ophthalmologist specialized in retina with over 10 years of experience performed BIO with scleral indentation for these patients. Patients who presented with peripheral retinal lesions predisposed or not to RD were included in the study, with indications for clinical follow-up or laser photocoagulation to prevent RD. The patients included underwent wide-angle retinographic examination using Panoramic Ophthalmoscope Optomap P-200DTX Optos® equipment by a trained technician having extensive experience in the use of the apparatus; these patients constituted the sample group. Cases excluded presented anatomical ocular alterations due to previous trauma or congenital abnormalities, eyes with severe opacity, previous history of RD or vitreoretinal surgery, aphakia, or difficulty rotating their heads.
Images were acquired using two different techniques available in the equipment. The first technique was performed on group A, performed with the patient’s gaze aimed at a position preset by the device, combined with slight rotation of the head to ensure that images of all four quadrants (superior nasal, inferior nasal, superior temporal, and superior temporal), including axes (horizontal and vertical), are captured (Figure 1). The second technique was performed on group B wherein a single image involving the posterior pole and the periphery was obtained. The eyes included in the study were randomly assigned sequentially (1:1) to either group A (photograph of the four quadrants) or group B (single photograph).

The physician who analyzed the images filled out a specific previously designed form and was kept unaware about the existence, quantity, type, and location of the following lesions in peripheral retina: lattice, hole, tear, thinning, retinoschisis, vitreous traction, and dialysis.
We compared the number of peripheral lesions found in the sample group with the images found in groups A and B. The images were analyzed by a second physician, a retina specialist with an experience of >10 years, who was kept unaware with regard to the eye that had the lesion or lesion type or location. For the analyses, the physician used the device software to enlarge the image throughout the retinal periphery. Statistical analysis was performed with the SPSS program and the data were entered into Microsoft Office Excel 2019. The image database is available in the device located at CBV.
RESULTS
BIO identified 192 patients, with an overall sample of 320 lesions in 255 eyes. Further, 18 eyes (17 patients; 16 from group A and 2 from group B) were excluded due to poor image quality and difficulty in head rotation; therefore, a total of 175 patients (237 eyes and 301 lesions) were included in the sample group. Of these, 110 eyes (143 lesions) were examined using the four-quadrant technique (group A) and 127 eyes (158 lesions) using a single central photograph (group B).
In the analysis of group A images, 122 lesions of the 143 (110 eyes) found in the sample group were identified, resulting in a sensitivity of 85.31% (Figure 2). On analyzing the single central photograph used in group B, 96 lesions of 158 (127 eyes) were identified, resulting in a sensitivity of 60.76% (Figure 3).
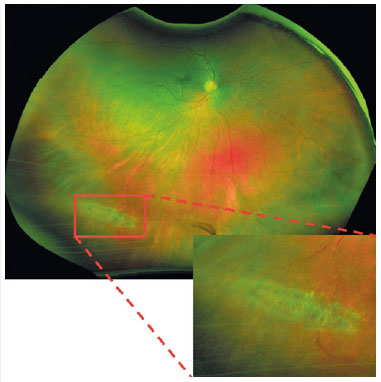

Data in table 2 show a sensitivity of 100% and 91.67% for the detection of lesions on the horizontal axis in groups A and B, respectively. However, sensitivity was lower on the vertical axis (Figure 1): 63.89% in group A and 35.56% in group B (Table 2).
The types of lesions with indication for laser photocoagulation or clinical follow-up were lattice degeneration (31.89%), atrophic hole (25.25%), tear (23.26%), thinning (9.97%), retinoschisis (5.32%), vitreous traction (3.65%), and dialysis (0.66%), in that order (Table 3). There was no significant difference in the number of lesions observed with BIO as well as in the types of lesions detected between groups A and B (Tables 1 and 2).
The assessments performed via image analysis described two lesions that were not detected with BIO: one retinal thinning and one atrophic retinal hole. These lesions were not considered a part of the sample group.
DISCUSSION
Nagiel et al. (2016) presented 149 cases using Optomap and detected 90.9% of peripheral lesions, including those not predisposed to RD; for retinal tears, their sensitivity was 43.8% compared with BIO(3,8). Panoramic 200 SLO, an older version of Optomap, presented 100% sensitivity for the detection of RD and 33% for peripheral holes compared with 67% for the usual examination. When considering all retinal lesions, Panoramic 200 SLO and BIO showed 62% and 73% sensitivity, respectively(9).
The field of view of Optomap features a few limitations, such as the presence of eyelids and eyelashes, associated with its great depth of focus(3,6,10). The eyelashes visualized in the inferior portion of the image represent the upper eyelid eyelashes. This effect is evident when analyzing inverted images, wherein the retinal image laterality (horizontal and vertical) is preserved; therefore, we have an inverted external image of the eyeball.
A study conducted with an artificial eye constructed using synthetic material found a limitation in superior and inferior visibility caused by both the presence of eyelashes and eyelids and the limited superior and inferior vision angles, which was noted even in an artificial eye model without any external factors. Another change observed is with regard to image brightness, which is smaller in the superior portion. The contrast is worse in the superior portion and better in the temporal portion, which can influence image assessment(6).
The data obtained in the present study justify the difficulty associated with locating the lesions on the vertical axis and demonstrate the excellent sensitivity on the horizontal axis. A study conducted with an artificial eye model found that rotating the eye 15° in each direction could increase the field of view to 106.6° superior, 121.2° nasal, 91° inferior, and 120.4° temporal.
The physician who analyzed the images assumed beforehand that one or both eyes featured peripheral lesions, although he was kept unaware regarding the number and type of lesions or their location. The fact that the physician previously presumed about the existence of injuries could have increased the rate of accuracy or the false description of lesions; however, the comparison of results showed otherwise because only two lesions described were not detected using BIO with scleral indentation.
In the present study, the sensitivity of detection of peripheral lesions with images obtained from the four quadrants was significantly higher (85.31%, group A) than that with single images (60.76%, group B; p>0.05). These results suggest that when researching peripheral lesions, it is recommended to consider at least four photographs with the patient’s eyes directed to a position preset by the device (superior, nasal, inferior, and temporal) combined with a slight rotation of the head to ensure that all four quadrants are captured.
The present protocol should be validated by other studies enrolling a larger number of cases to facilitate the adoption of this technology as one of the recommended methods to safely identify peripheral retinal lesions in the future.
REFERENCES
1. Ghasemi Falavarjani K, Tsui I, Sadda SR. Ultra-wide-field imaging in diabetic retinopathy. Vision Res. 2017 Oct;139:187-90.
2. Bronstein MA, Mainster MA, Pomerantzeff O, Trempe CL, Schepens CL, Ávila MP, Scheneider J. High Magnification Fundus Photografhy With the Macula-Disk Camera. Ophthalmology (Rochester). 1982;89(8):189-91.
3. Nagiel A, Lalane RA, Sadda SR, Schwartz SD. ULTRA-WIDEFIELD FUNDUS IMAGING: A Review of Clinical Applications and Future Trends. Retina. 2016;36(4):660-78.
4. Peng J, Zhang Q, Jin H-Y, Lu W-Y, Zhao P-Q. Ultra-wide field imaging system and traditional retinal examinations for screening fundus changes after cataract surgery. Int J Ophthalmol. 2016;9(9):1299-303.
5. Liu L, Wang F, Xu D, Xie C, Zou J. The application of wide-field laser ophthalmoscopy in fundus examination before myopic refractive surgery. BMC Ophthalmol. 2017;17(1):250.
6. Oishi A, Hidaka J, Yoshimura N. Quantification of the image obtained with a wide-field scanning ophthalmoscope. Invest Ophthalmol Vis Sci. 2014;55(4):2424-31.
7. Mackenzie PJ, Russell M, Ma PE, Isbister CM, Maberley DAL. Sensitivity and specificity of the optos optomap for detecting peripheral retinal lesions. Retina. 2007;27(8):1119-24.
8. Lee DH, Kim SS, Kim M KH. Identifiable Peripheral Retinal Lesions Using Ultra-Widefield Scanning Laser Ophthalmoscope and Its Usefulness in Myopic Patients. J Korean OphthalmolSoc. 2014;55(12):1814-20.
9. Khandhadia S, Madhusudhana KC, Kostakou A, Forrester JV, Newsom RSB. Use of Optomap for retinal screening within an eye casualty setting. Br J Ophthalmol. 2009;93(1):52-5.
10. Inoue M, Yanagawa A, Yamane S, Arakawa A, Kawai Y, Kadonosono K. Wide-field fundus imaging using the Optos Optomap and a disposable eyelid speculum. JAMA Ophthalmol. 2013;131(2):226.
AUTHOR’S INFORMATION





Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
March 10, 2020.
Accepted on:
May 5, 2020.