George Alencastro de Carvalho Paes Landim1; Rayssa Medeiros Léda2; Vinícius Stival Veneziano Sobrinho1
DOI: 10.17545/eOftalmo/2019.0024
ABSTRACT
We report the case of a 62-year-old patient with primary iris stromal cyst that was treated with laser. A female patient presented with a complaint of foreign body sensation and decreased visual acuity in the left eye for last 2 months. Ophthalmologic and additional examinations showed a cystic lesion exhibiting features compatible with a primary iris stromal cyst. The treatment of choice was neodymium-doped yttrium aluminum garnet laser with low parameters, leading to regression of the cystic contents and improvement of visual acuity and symptoms. No complications were observed during 6 months of follow-up. The literature does not describe the specific laser therapy for stromal cysts, but this mode of treatment is an alternative to manage this condition. Further prospective studies with a greater number of cases to assess potential benefits and side effects are necessary.
Keywords: Iris Diseases; Laser Coagulation; Iris Neoplasms; Case Reports.
RESUMO
Relata-se um caso de cisto estromal iriano primário tratado com laser em paciente de 62 anos. Paciente do sexo feminino com queixa de sensação de corpo estranho e diminuição da acuidade visual em olho esquerdo, com evolução de dois meses. O exame oftalmológico e complementar demonstrou lesão cística compatível com cisto estromal iriano primário. O tratamento de escolha foi com o laser tipo Neodymium:Yttrium-Aluminum-Garnet com baixos parâmetros, evoluindo com regressão do conteúdo cístico, melhora da acuidade visual e dos sintomas. Não foram observadas complicações em seis meses de acompanhamento. A literatura não revela descrição terapêutica com laserterapia específica para cistos do tipo estromal, sendo este modo de tratamento uma alternativa no manejo da patologia. Estudos prospectivos e com maior número de casos para avaliar os potenciais benefícios e efeitos colaterais são necessários.
Palavras-chave: Doenças da Íris; Fotocoagulação a Laser; Neoplasias da Íris; Relatos de Casos.
RESUMEN
Se relata un caso de quiste estromal de iris primario tratado con láser en paciente de 62 años. Paciente del sexo femenino con quejas de sensación de cuerpo extraño y disminución de la acuidad visual en ojo izquierdo, con evolución de dos meses. El análisis oftalmológico y complementar demostró lesión quística compatible con quisto estromal de iris primario. El tratamiento elegido fue con láser tipo Neodymium:Yttrium-Aluminum-Garnet con bajos parámetros, evolucionando con regresión del contenido quístico, mejora de la acuidad visual y de los síntomas. No se observaron complicaciones en seis meses de seguimiento. La literatura no revela descripción terapéutica con laserterapia específica para quistes del tipo estromal, siendo este modo de tratamiento una opción en el manejo de la patología. Se hacen necesarios estudios prospectivos y con mayor número de casos para evaluar los potenciales beneficios y efectos colaterales.
Palabras-clave: Enfermedades del Iris; Coagulación con Láser; Neoplasias del Iris; Informes de Casos.
INTRODUCTION
Primary iris stromal cysts are uncommon, and clinical management and long-term prognosis of these cysts regarding surgical or conservative approaches need to be investigated, as there is lack of consensus on them. These cysts are defined as structures that emerge within the iris stroma, anteriorly to the iris pigment epithelium, in eyes with no history of surgery or trauma1,2. They are usually unilateral and single, adhering to the epithelium and exhibiting progressive growth3. They have a characteristic clinical appearance with smooth surface, are positive to transillumination, and occasionally present with fluid with suspended particles4,5.
Cystic lesions of the iris represent 21% of all iris tumors and are divided into two broad categories: stromal cysts and pigment epithelial cysts. Stromal tumors developing after surgery or trauma in patients aged >60 years have a prevalence of 11%6; however, their spontaneous occurrence, as observed in the present case, is rare2. In the literature, cases have been reported in which pigment epithelial cysts were treated with laser therapy using low parameters7, but to the best of our knowledge, there is no specific therapeutic description for stromal cysts using this method.
Ultrasonic biomicroscopy is essential for the diagnosis of iris cysts and their differentiation from other anterior-segment lesions that can simulate melanoma and solid tumors8. Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser emerges as an alternative treatment to manage iris cystic tumors.
CASE REPORT
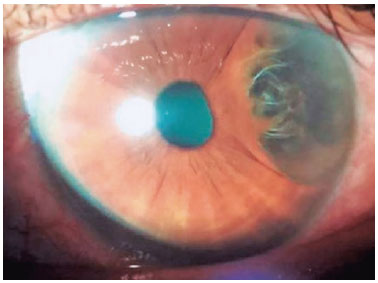
A 62-year-old female patient sought an ophthalmologist due to complaints of foreign body sensation, ocular hyperemia, and mild visual turbidity in her left eye (OS), with no complaints in the right eye (OD). She had no history of surgery or trauma in either eye and had a diagnosis of systemic arterial hypertension, which was being monitored by a cardiologist and was under control. Her best corrected visual acuity was 1.0 logMAR in the OD and 0.9 logMAR in the OS. The examination findings of the anterior segment of the right eye were unremarkable, but the left eye showed a single and exuberant iris cyst positive to transillumination, measuring 5.5mm in vertical diameter and 3.0mm in horizontal diameter, with peripheral insertion, and affecting the temporal third of the left eye (Figure 1).
Specular microscopy of the left eye showed no significant changes in cellularity and cell morphism. The OS daily curve of intraocular pressure showed a mean pressure of 10.2mmHg, with a maximum variation of 2mmHg. Computerized campimetry showed no scotoma defects. Ophthalmoscopy of the posterior pole showed no changes in the macular region, optic nerve, and peripheral retina.
Anterior chamber tomography (Pentacam®, Oculus, Germany) was performed for the left eye, highlighting the cystic features of the lesion and absence of intralesional tumoring (Figure 2).

Ultrasound biomicroscopy revealed the cystic nature of the lesion and showed particles suspended in its content, which moved in the intralesional space during the dynamic examination (Figure 3).

The patient underwent a single session with a 532-nanometer (nm) Nd:YAG laser (Iridex Corporation, Mountain View, California, United States of America) to rupture the edge of the lesion (cystotomy) and drain its contents. The parameters used were low in comparison with the ones reported in the literature for argon laser photocoagulation. To disrupt the iris stroma, two 280-mW shots were performed for 0.2s, aiming at a 50-μm target located in the lower part of the cyst. One drop of 0.2% brimonidine was administered 30 min before the procedure. The patient's condition improved without any immediate postoperative complications or intraocular pressure changes. She was evaluated weekly during the first month. Thirty days postoperatively, she reported improvement in ocular discomfort, and her left eye visual acuity had improved from logMAR 0.79 to logMAR 1.00. At the end of the sixth month of follow-up, the patient presented no symptoms of discomfort or foreign body sensation and maintained a visual acuity of logMAR 1.00. Figure 4 shows the appearance of the anterior chamber 6 months after photocoagulation, with a partial reduction in cystic volume and a slight increase in pupillary diameter in the temporal region.

DISCUSSION
Iris cysts can be classified into primary or secondary, and cystic lesions arise from the pigment epithelium of the iris or from the tissue stroma1,2. Stromal cysts represent only 11% of primary cysts, and they may be congenital or acquired6. The accumulated experience on the treatment of this condition is mostly based on case reports or small case series3,5,10-12. Most cases of acquired iris cysts are reported in children and young adults aged up to 40 years, accounting for 65% of cases6. Primary iris stromal cysts normally remain stable in adults, but exhibit a tendency for growth and visual axis impairment in children13. No predilection for either sex has been described9,12, and the typical involvement is unilateral, with a single cystic lesion affecting mainly the lower and temporal regions of the iris1.
Stromal cysts have a characteristic clinical appearance with smooth surface, are positive to transillumination, and occasionally present with fluid with suspended particles14,15. The lesion can gradually grow and rupture, leading to a secondary clinical picture of iritis, photophobia, pain, and increased intraocular pressure. This feature should be especially paid attention to in newborns, in whom cysts can manifest within the first weeks of life, causing photophobia and buphthalmos16.
Although the pathogenesis of these cysts remains controversial, most of them result from a separation of the epithelial layers of the iris; however, the spontaneous cyst observed in the present case arose from trapped superficial ectodermal cells within the stroma, suggesting an embryological origin and its consequent classification as a primary stromal iris cyst. Paridaens et al. reported high-molecular-weight keratin and absence of S100 proteins using mono- and polyclonal antibodies, indicating an ectodermal rather than neuroectodermal surface (Figure 5)17.

Ultrasound biomicroscopy plays an essential role in the diagnosis of iris cysts and their differentiation from other anterior-segment lesions that simulate melanoma and solid tumors. Primary cysts of the iris pigment epithelium and ciliary body are characterized by a thin, regular, smooth wall with medium reflectivity and anechoic content. Iris stromal cysts protrude into the anterior chamber and have a thicker wall18. In a case series with 108 adult patients, in which differential diagnoses for cystic lesions of the anterior segment were analyzed, only one case was identified as a stromal cyst, demonstrating the low frequency of this condition.(8)
In literature, cases have been reported in which pigment epithelial cysts were treated with laser therapy using low parameters,(16) but there is no specific therapeutic description for stromal cysts using this method. The accurate diagnosis of iris cysts and their correct etiological classification are crucial for an intervention that alleviates symptoms and improves visual acuity. Nd:YAG laser emerges as an alternative treatment to manage this condition, and prospective studies with a greater number of cases are needed to assess the potential benefits and side effects of this therapy.
REFERENCES
1. Rao A, Gupta V, Bhadanghe Y, Sharma R, Shields JA. Iris cysts: a review. Semin Ophthalmol. 2011 Jan;26(1):11-22.
2. Lois N, Shields CL, Shields JA, Mercado G, Potter P. Primary iris stromal cysts. A report of 17 cases. Ophthalmology. 1998 Jul;105(7):1317-1322.
3. Capó H, Palmer E, Nicholson DH. Congenital cysts of the iris stroma. Am J Ophthalmol. 1993 Aug;116(2):228-32.
4. Shields JA. Primary cysts of the iris. Trans Am Ophthalmol Soc. 1981;79:771-809.
5. Shields J, Shields C, Lois N, Mercado G. Iris cysts in children: classification, incidence and management. Br J Ophthalmol. 1999 Mar;83(3):334-8.
6. Shields CL, Kancherla S, Patel J, Vijayvargiya P, Suriano MM, Kolbus E, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology. 2012;119(2):407-14.
7. Costa JCL, Montenegro ACP, Santos AV, Dias MBC, Dias TJ, Stenio R. Symptomatic primary iris cysts treated with frequency-doubled Nd:YAG laser photocoagulation. Rev Bras Oftalmol. 2017;76(4):198-201.
8. Marigo FA, et al. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999 Nov;106(11): 2131-35.
9. Shields JA, Kline MW, Augsburger JJ. Primary iris cysts: review of the literature and report of 62 cases. Br J Ophthalmol. 1984 Mar;68(3):152-166.
10. Sugar HS, Nathan LE. Congenital epithelial cysts of the iris stroma. Ann Ophthalmol. 1982 May;14(5):483-5.
11. Coburn A, Messemer EP, Boniuk M, Font RL. Spontaneous intrastromal iris cyst: a case report with immunohistochemical and ultrastructural observations. Ophthalmology. 1985 Dec; 92(12):1691-95.
12. Mullaney J, Fitzpatrick C. Idiopathic cyst of the iris stroma. Am J Ophthalmol. 1973 Jul;76(1):64-8.
13. Georgalas I, Petrou P, Papaconstantinou D, Brouzas D, Koutsandrea C, Kanakis M. Iris cysts: a comprehensive review on diagnosis and treatment. Surv Ophthalmol. 2018 May/Jun;63(3):347-64.
14. Shields JA, Shields CL, Lois N, Mercado G. Iris cysts in children: classification, incidence and management. Br J Ophthalmol. 1999;83(3):334-8.
15. Shields CL, Arepalli S, Lally EB, Lally SE, Shields JA. Iris stromal cyst management with alcohol-induced sclerosis in 16 patients. JAMA Ophthalmol. 2014 Jun;132(6):703-8.
16. Shields CL, Shields PW, Manalac J, Jumroendararasame C, Shields JA. Review of cystic and solid tumors of the iris. Oman J Ophthalmol. 2013 Sep;6(3):159-64.
17. Paridaens AD, Deuble K, McCartney AC. Spontaneous congenital non-pigmented epithelial cysts of the iris stroma. BrJ Ophthalmol. 1992 Jan;76(1):39-42.
18. Ayres B, Allemann N, Nakanami C, Adan CBD. Cistos primários do epitélio pigmentar da íris e corpo ciliar: aspectos de biomicroscopia ultra-sônica. Arq Bras Oftalmol. 2000 Oct;63(5):337-343.



Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
May 2, 2019.
Accepted on:
August 13, 2019.