Rafaela Linck; Pedro Cabral de Oliveira Mello; Yasminn Ferrer Farina; Jorge Henrique Cavalcante Tavares; Mário Henrique Camargos de Lima
DOI: 10.17545/eoftalmo/2019.0017
ABSTRACT
Cornea is a common site of trauma, which could be avoided if the correct use of personal protection equipment (PPE) were observed.
OBJECTIVE: To identify the epidemiological profile of patients with occupational corneal foreign bodies treated at the ophthalmological clinic of the Guarulhos Hospital Complex in the State of São Paulo, Brazil.
METHODS: This was a retrospective, non-interventional study with 134 patients who suffered injuries from corneal foreign bodies and who were assisted between July 2017 and June 2018. The following data were assessed: age; gender; occupation; affected eye; number, location, and nature of the foreign bodies; availability and use of PPE at the time of the accident; type of safety goggles used; attempt to remove the foreign body at home; history of this type of trauma; and time elapsed between the accident and seeking specialized care.
RESULTS: Most patients were men (94.78%) and the predominant age group was 19–35 years (41.79%); the right eye was predominantly affected (54.48% of cases). Most patients worked in the processing industry (57.46%). The corneal foreign bodies were mostly made of iron (73.88%) and 59% of the patients wore no PPE at the time of the accident.
CONCLUSION: It is the responsibility of the employers to increase the availability of PPE to implement educational programs and promote inspection.
Keywords: Eye Foreign Bodies; Accidents, Occupational; Cornea; Personal Protective Equipment.
RESUMO
A córnea é um sítio frequente de traumatismo, que poderia ser evitado caso o uso correto dos equipamentos de proteção individual (EPI) fosse respeitado.
OBJETIVO: Identificar o perfil epidemiológico dos pacientes com corpos estranhos corneais ocupacionais atendidos na clínica oftalmológica do Complexo Hospitalar de Guarulhos - São Paulo.
MÉTODO: Estudo retrospectivo, não intervencionista, de 134 pacientes com acidentes por corpos estranhos corneais, atendidos entre julho de 2017 e junho de 2018. Foram avaliados dados referentes à faixa etária, sexo, profissão, olho afetado, quantidade, localização, natureza do corpo estranho, disponibilidade de EPI e de seu uso no momento do acidente e o tipo de óculos utilizados, tentativa de remoção em domicílio, antecedente prévio e tempo de procura por médico especialista.
RESULTADO: A maioria dos pacientes era do sexo masculino (94,78%), com predomínio no grupo etário entre 19 e 35 anos (41,79%), sendo o olho direito acometido em 54,48% dos casos. A principal atividade laboral estava relacionada à indústria de transformação (57,46%), 73,88% dos corpos estranhos corneais eram de ferro e 59% dos casos não estava utilizando EPI no momento do acidente.
CONCLUSÃO: Cabe às empresas ampliar a disponibilidade desses materiais, implantar programas educacionais, além de melhorar a fiscalização.
Palavras-chave: Corpos Estranhos no Olho; Acidentes de Trabalho; Córnea; Equipamento de Proteção Individual.
RESUMEN
La córnea es un lugar frecuente de traumatismo, el cual se podría evitar si se respetara el uso correcto de los equipos de protección individual (EPI).
OBJETIVO: Identificar el perfil epidemiológico de los pacientes con cuerpos extraños corneales ocupacionales con atención en la clínica oftalmológica del Complexo Hospitalario de Guarulhos - São Paulo.
MÉTODO: Estudio retrospectivo, no intervencionista, de 134 pacientes con accidentes por cuerpos extraños corneales, con atención entre julio de 2017 y junio de 2018. Se han evaluado los datos referentes a la edad, sexo, profesión, ojo afectado, cantidad, ubicación, naturaleza del cuerpo extraño, disponibilidad de EPI y su uso en el momento del accidente y el tipo de anteojos utilizados, intento de remoción en el hogar, antecedente y tiempo de búsqueda por un médico especialista.
RESULTADO: La mayoría de los pacientes era del sexo masculino (94,78%), con predominio en el grupo entre 19 y 35 años (41,79%), siendo el ojo derecho acometido en un 54,48% de los casos. La principal actividad laboral estaba relacionada a la industria de transformación (57,46%), 73,88% de los cuerpos extraños corneales eran de hierro y 59% de los casos no estaba utilizando EPI en el momento del accidente.
CONCLUSIÓN: Cabe a las empresas ampliar la disponibilidad de dichos materiales, implantar programas educacionales, además de mejorar la fiscalización.
Palabras-clave: Cuerpos Extraños en el Ojo; Accidentes de Trabajo; Córnea; Equipo de Protección Personal.
INTRODUCTION
The cornea is a common site of trauma because of its location and its function in eye protection1. Ocular accidents have a social, psychological, and economic impact as a result of their high frequency and because they predominantly affect the working-age population. Work accidents account for the majority of cases of ocular trauma2. In Brazil alone, 10% of occupational accidents are ocular injuries, and superficial corneal foreign bodies are the most common cause of preventable eye injury3.
Superficial corneal foreign bodies account for 74% of cases of ocular trauma and 72% to 91.85% of cases occur in the work environment4.
An injury involving a foreign body on the surface of the cornea consists in a closed eye injury that does not cause eye perforation. These cases usually show a good clinical course, but may lead to more serious problems, such as infectious keratitis and its complications.
The objective of the present study was to analyze the epidemiology of the patients treated for occupational injury involving corneal foreign bodies at the ophthalmological clinic of the Guarulhos Hospital Complex, in the city of Guarulhos, State of São Paulo, Brazil. It attempts to contribute with epidemiological data related to ocular injury to facilitate the institution of preventive measures.
MATERIALS AND METHODS
This was a retrospective, non-interventional study with 134 patients who suffered injuries from corneal foreign bodies and who were treated at the ophthalmological clinic of the Guarulhos Hospital Complex between July 2017 and June 2018. The sample consisted of self-referral patients at this clinic and treatment was performed by ophthalmologists.
The study was conducted using semi-structured interviews and the following data were obtained: age; gender; occupation; affected eye; number and location of corneal foreign bodies; nature of the foreign body; availability of personal protection equipment (PPE); use of safety goggles at the time of the accident and type of goggles used (wide-vision, single-hazard, and overlay); attempt to remove the foreign body at home; history of this type of trauma; and time elapsed between the accident and seeking specialized care.
Age was divided into the following groups: 1) 0–18 years; 2) 19–35 years; 3) 36–50 years; and 4) over 50 years. The following foreign body locations were considered in this study: 1) central cornea (central 3.0 mm); 2) superior cornea; 3) inferior cornea; 4) nasal cornea; and 5) temporal cornea. The professional activities were grouped based on a modification of the classification proposed by the Brazilian Institute of Geography and Statistics (IBGE), as follows: 1) workers of the processing industry; 2) workers of the agricultural industry; 3) workers of the construction industry; 4) household workers; 5) trade and service workers; 6) workers of the transportation sector; 7) students/minors, and 8) workers with other activities. With regard to the nature of the foreign body, the following classification was adopted: 1) iron, 2) wood, 3) glass, 4) steel, 5) chemical products, and 6) others. Workers of the fishing industry and the financial and civil service sectors were included in the “workers of other industries” group, because there were few cases. Returning patients who had already been assisted on the previous days and patients with corneal foreign bodies of non-occupational origin were excluded from the study. The collected data were entered in Microsoft Excel® spreadsheets and were subsequently used as a database.
RESULTS
A total of 134 individuals with occupational corneal foreign bodies were studied between July 2017 and June 2018, of which 127 (94.78%) were men and 7 (5.22%) were women.
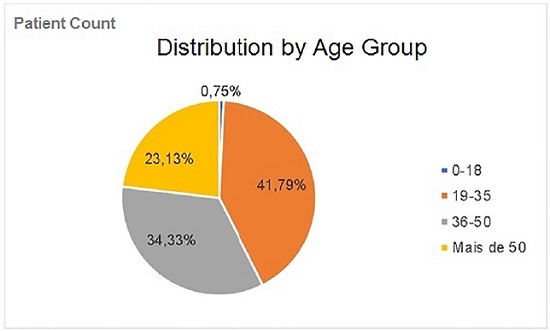
With regard to age, the group 19–35 years accounted for 41.79% of the cases (Graph 1).
The right eye and the left eye were affected respectively in 54.48% and 45.52% of cases. There were no accidents involving both eyes simultaneously. With regard to the use of safety goggles at the time of the accident, 79 individuals wore no PPE (Table 1). Eighty-nine patients (66.42%) reported the availability of PPE in the workplace at the time of the accident, and 34 patients (25.37%) did not follow the recommendations for use.
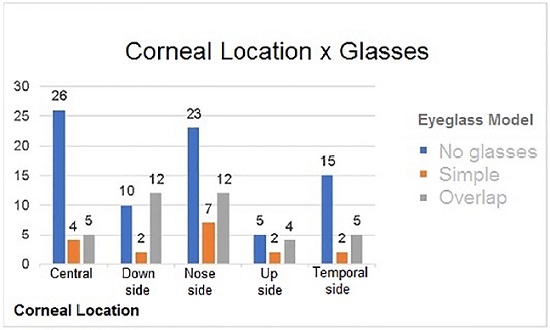
The location of the foreign body in the cornea varied depending on whether the patient was wearing PPE at the time of the injury. When PPE was not worn, the most common location was the central cornea (26 cases). No patient treated at our clinic reported wearing the wide-vision PPE model. In those who reported wearing the single-hazard model (17 cases), the predominant location was the nasal cornea (7 cases), whereas in those wearing overlay goggles (38 cases) the most frequent locations were the nasal and inferior cornea (12 cases each) (Graph 2).
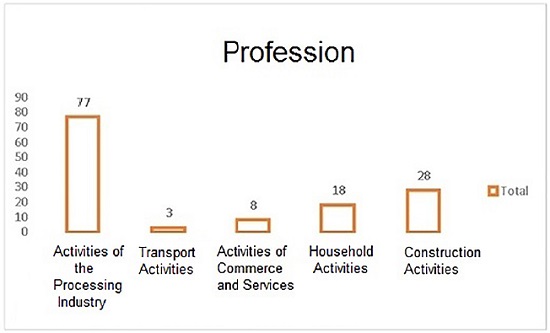
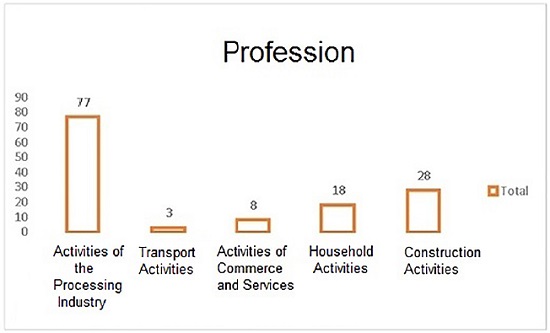
With regard to the patients’ occupation, 57.46% of the individuals were workers of the processing industry (Graph 3). Biomicroscopy showed that 130 patients (97.01%) had a single corneal foreign body and 4 patients (2.99%) had multiple objects.
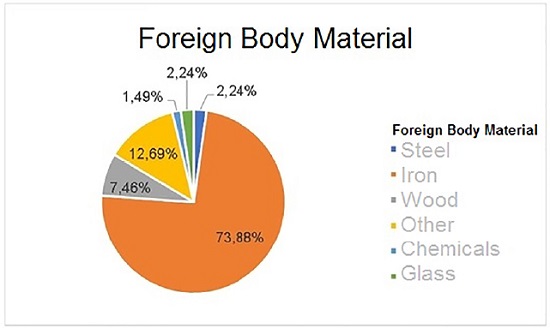
With regard to the nature of the corneal foreign bodies, 73.88% were iron objects and 1.49% were chemical products (Graph 4).
With regard to the time elapsed between the accidents and seeking specialized care, 67 workers (50%) were treated within 24 hours (Graph 5). When questioned about attempting to remove the foreign body at home, 92 patients (68.66%) denied this action and 42 patients (31.34%) confirmed having tried to remove the object themselves.
With regard to the patients’ history of occupational corneal trauma by a foreign body, 56 individuals (58.21%) reported previous occurrences whereas 78 individuals (41.79%) stated that time was the first event.
DISCUSSION
Superficial corneal foreign bodies are the most common type of ocular trauma in Brazil and a very frequent cause of emergency visits4,5,6. They account for 54.6% to 81.8% of all ocular trauma4,7. A study conducted in Scotland in 2009, which was divided into 2 periods, showed that corneal foreign bodies were the most common type of injury, corresponding to 59% and 64% of occupational eye injuries in the first and second periods, respectively8.
In this study and in other Brazilian and foreign studies, there was a predominance of ocular trauma in male individuals (94.78%), probably because the higher-risk occupations are held by men and because they are usually less careful during work activities4,7,8,9,10.
The most affected age group was young individuals (19–35 years), which accounted for 41.79% of cases. This is in line with the epidemiology of ocular trauma8, 11. This population corresponds to the working-age group and the possible lack of professional experience may contribute to this statistic3,8,12. Recent studies emphasize that younger individuals are more careless and even neglect the use of safety equipment10.
The right eye was affected in 54.58% of cases. There was no relative difference between the two eyes, a result that was also obtained in the reviewed studies 3,4,7. Biomicroscopy showed that 97.01% of patients had a single corneal foreign body, as did a study conducted in the Brazilian state of Piauí 4. This finding may be explained by the fact that the main material of the foreign bodies was iron, which does not frequently shatter.
In our study, 59% of patients wore no PPE at the time of the accident. This is a lower percentage than that obtained in a study conducted in the Brazilian state of Espírito Santo, in which 82.9% of patients who suffered this type of trauma in the workplace wore no PPE11. This latter result may be explained by the fact that PPE is perceived as being uncomfortable or by the safety regulations being ignored or disregarded by these workers. It is important to note that PPE should not only be technically adequate but also comfortable to wear in the user’s assessment, because facial anatomical variations exist and should be taken into account.
In 2005, only 34.2% of patients who went to the emergency ward of the Federal University of São Paulo stated that they were wearing protection at the time of the trauma, even when PPE was available to them in the workplace13. In our study, 25.37% had PPE available to them but did not follow the recommendations for use.
In one study, although 43% of patients wore goggles at the time of the accident, they still suffered corneal injury14. In another study, 45% of patients had ocular lesions while wearing some form of eye protection9. Similar results were obtained in the present study, with 41% of individuals reporting the use of PPE when the accident occurred.
Despite the limitations of the study design, including the fact that it was not possible to confirm the accuracy of the information given by the interviewed individuals, these results suggest that education campaigns should not just focus on informing about the need to wear PPE and the risk of accidents. It is also necessary to increase inspection and provide safety goggles appropriate for each activity performed by each worker. The accidents that occurred despite the use of protection may be related to protection equipment being inappropriate for a certain task or to its incorrect use. It is also possible that the interviewees gave false answers due to fear that disclosing the information could compromise their employment.
In a study conducted in the Hospital of the Federal University of Santa Catarina, in Southern Brazil, between January 2003 and December 2004, the intermediate corneal location of the injury was the most common (32.7%), followed by the peripheral location (136 cases or 31.4%), and the central location (116 cases or 26.7%) 3. Among patients in Turkey, the central area was also the least affected, with injuries occurring in 16% of individuals14. In our study, the foreign bodies reached the central 3.0 mm of the cornea in 26.11% of the patients.
The distribution of occupational accidents varies according to the degree of development of the region and the socioeconomic characteristics of the area where the study takes place 9. In Botucatu (State of São Paulo), accidents were mostly associated with agricultural activities (29.8%), general services (21.5%), and the metallurgical industry (19.6%)3. By contrast, in our study 57.46% of accident victims were workers of the processing and construction industries (20.90%). A similar result was obtained in the city of Belo Horizonte (State of Minas Gerais, Brazil), i.e., the occupations most involved in ocular trauma in the workplace were metal workers and construction workers (20.9% each), welders (13.3%), and mechanics (10.8%) 15.
With regard to the nature of the corneal foreign bodies, 73.88% were iron metal objects, which are in line with the data obtained by the Federal University of Piauí, where this material accounted for 68.58% of accidents 4.
With regard to the time elapsed between the accidents and seeking assistance in a specialized center, 50% of workers were treated within 24 hours of the accident and 48.51% between 24 hours and 7 days after the accident. In Fortaleza, in the Brazilian state of Ceará, 72% of patients had to wait more than 12 hours to have access to specialized medical care8. Because the Guarulhos Hospital Complex is an ophthalmology reference hospital that also serves neighboring municipalities, it receives a great number of patients who travel there for specialized eye care, which explains the longer time elapsed until they receive care compared to the studies in the reviewed literature. Ophthalmological evaluation after ocular trauma is crucial to initiate adequate treatment, minimize the risks of infection, and favor proper healing.
In our study, 31.34% of patients attempted to remove the foreign bodies by themselves before seeking our assistance. The percentage in Turkey was higher (52%). An accident involving corneal foreign bodies may, by itself, lead to infections, and attempts to remove the foreign body by oneself using potentially traumatic instruments increase the risk of corneal infection and, consequently, the risk of compromising visual quality 14.
CONCLUSION
The availability of PPE was shown to be high; however, faults in equipment adequacy and the inspection of its use were the factors involved in the occurrence of accidents. In workplaces with a high risk of eye injury, making PPE available without verifying its effectiveness and its correct use by the employees is not enough. Brazil lacks a culture of prevention and tends to act primarily on damage control after an occupational accident has occurred, which maximizes costs and morbidity associated with these events.
REFERENCES
1. Cohen J, Carvalho RC, Romão E. Trauma ocular por acidente de trabalho em Manaus (AM). Rev Bras Oftalmol. 1994;53(2):149-52.
2. Ullern M. [Ocular trauma]. Rev Prat. 1995 feb;45(4):431-5.
3. Netto AA, Wayhs LF, Rodrigues IK, Astolfi M, Neumaier R, Aguiar UJ. Estudo de 434 casos de corpos estranhos corneais no Hospital Universitário da Universidade Federal de Santa Catarina. ACM Arq Catarin Med. 2006 abr/jun;35(2):56-62.
4. Leal FAM, Silva e Filho AP, Neiva DM, Learth JCS, Da Silveira DB. Trauma ocular ocupacional por corpo estranho superficial. Arq Bras Oftalmol. 2003 jan;66(1):57-60.
5. Spada FR, Rodrigues EB, Grumann Jr A, Cunha ET. Corpo estranho de córnea: relação com a atividade profissional. Rev Bras Oftalmol. 2000;59(1):36- 9.
6. Ramakrishnan T, Constantinou M, Jhanji V, Vajpayee RB. Corneal metallic foreign body injuries due to suboptimal ocular protection. Arch Environ Occup Health. 2012;67(1):48-50.
7. Kara-José Jr N, Oliveira-Neto JC, Silva ALB, Schellini SA. Acidentes oculares ocupacionais - ocorrência em Botucatu, no período de 1988 a 1992. Arq Bras Oftalmol. 1994;57:389-93.
8. Matos AG, Cavalcante RG, de Francesco Figueiredo T, de Freitas Chaves M, Bandeira MFP, de-Souza FA. Profile of occupational eye injury at an ophthalmologic emergency department. Rev Bras Med Trab. 2017;15(4):329-32.
9. Netto AA, Thiesen EB, Silvano RE, Müller TP, Siewert MC, Basso G. Perfil epidemiológico de 144 pacientes portadores de corpos estranhos subtarsais no Hospital Universitário da Universidade Federal de Santa Catarina. ACM Arq Catarinen Med. 2006;35(4):97-103.
10. Aguilar F. Repercusiones socioeconómicas de las lesiones por cuerpos extraños. Salud Publica México. 1985;27(1):66-70.
11. Milanez M, Saraiva PGC, Barcellos NN, Saraiva FP. Epidemiological and occupational profile of eye trauma at a referral center in Espírito Santo, Brazil. Rev Bras Oftalmol. 2017 feb;76(1):7-10.
12. Tzelikis PFDM, Diniz CM, Alvim HDS, Gonçalves RM, Araújo Júnior ARD, Trindade FC. Perfil do paciente com trauma ocular atendido no Hospital São Geraldo da Universidade Federal de Minas Gerais. Rev Bras Oftalmol. 2002 dez;61(12):885-891.
13. Gerente VM, Melo GB, Regatiei CVS, Alvarenga LS, Martins EN. Trauma ocupacional por corpo estranho corneano superficial. Arq Bras Oftalmol. 2008 mar/abr;71(2):149-52.
14. Ozkurt ZG, Yuksel H, Saka G, Guclu H, Evsen S, Balsak S. Metallic corneal foreign bodies: an occupational health hazard. Arq Bras Oftalmol. 2014 apr;77(2):81-83.
15. Gonçalves RM, Diniz CM, Alvim HS. Trauma ocular por acidente de trabalho. Rev Bras Oftalmol. 2003;62(3):199-203.

Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
October 14, 2018.
Accepted on:
April 11, 2019.