Carlos Eduardo dos Reis Veloso1; Márcio Bittar Nehemy2
DOI: 10.17545/eoftalmo/2018.0010
ABSTRACT
Choroidal neovascularization (CNV) is a rare but potentially severe complication of infectious and noninfectious inflammatory ocular diseases that warrants prompt diagnosis and treatment to prevent the worsening of central visual acuity in affected patients. Fluorescein angiography (FA), optical coherence tomography (OCT), and optical coherence tomography angiography (OCTA) may help to distinguish CNV from the active underlying inflammatory disease. The main forms of treatment available are antiangiogenic therapy, corticosteroid therapy, and immunosuppression.
Keywords: Neovascularization, Pathologic; Uveitis; Choroid.
RESUMO
A neovascularização de coroide (NV) é uma complicação rara mas potencialmente grave das doenças oculares inflamatórias infecciosas e não-infecciosas, que deve ser diagnosticada e prontamente tratada com o intuito de evitar a piora da acuidade visual central nesses pacientes. A angiofluoresceinografia, a tomografia e coerência óptica e a angiotomografia são exames úteis e que podem auxiliar na diferenciação da NVC com a atividade da doença inflamatória subjacente. A terapia anti-angiogênica, a corticoterapia e a imunossupressão são as principais formas de tratamento disponíveis.
Palavras-chave: Neovascularização patológica, Uveíte, Coroide.
RESUMEN
La neovascularización coroidea (NVC) es una enfermedad inusual, pero potencialmente grave de las enfermedades oculares inflamatorias infecciosas y no-infecciosas, que debe diagnosticarse y rápidamente tratarse con el intuito de evitar el empeoramiento de la acuidad visual central en eses pacientes. La angiofluoresceinografía, la tomografía de coerencia óptica y la angiotomografía son exámenes útiles y que pueden auxiliar a distinguir la NVC de la actividad de la enfermedad inflamatoria subyacente. La terapia antiangiogénica, la corticoterapia y la inmunosupresión son los principales medios de cuidado disponibles.
Palabras-clave: Neovascularización Patológica; Uveítis; Coroides.
CNV is a possible complication of infectious and noninfectious inflammatory ocular diseases and may occur in 2%–3% of cases of posterior uveitis.1 In uveitis, inflammatory reactions in the choriocapillaris or retinal pigment epithelium (RPE) may lead to local ischemia, with subsequent production of vascular endothelial growth factor (VEGF) and other cytokines, which in turn may lead to CNV.2 In addition, the inflammatory process damages the RPE-Bruch’s membrane complex, permitting CNV to permeate these layers and reach the subretinal space. Therefore, CNV in uveitis is type 2 (located above the RPE) in most cases, in contrast to CNV in exudative age-related macular degeneration (AMD), where type 1 (below the RPE) is predominant.3
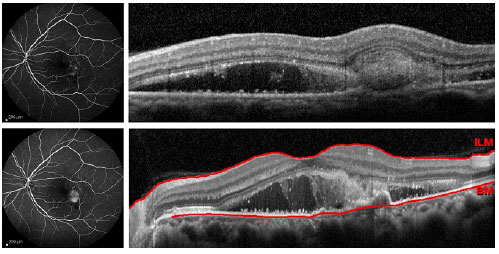
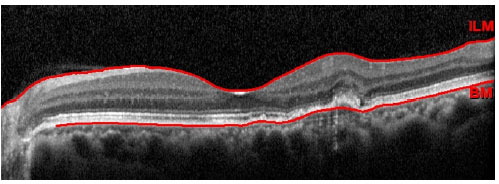
CNV usually affects individuals aged <50 years, and its early diagnosis is essential for the prompt initiation of treatment to prevent fibrosis and permanent loss of central visual acuity in this economically active population.4 CNV may be the first clinical manifestation of uveitis and may be associated with active inflammatory or infectious disease. CNV is subfoveal in 75% of cases but may also occur in the juxtafoveal or extrafoveal regions. This complication usually develops adjacent to retinochoroidal scars or granulomas. The main symptoms of CNV are central scotoma and metamorphopsia, but the patient may be asymptomatic, especially in cases where the affected eye already has low visual acuity owing to the presence of a central or pericentral scar or granuloma.2 The signs of CNV may be subtle and confused with ongoing uveitis. The main complementary examinations useful in distinguishing these clinical signs are FA, indocyanine green angiography (ICGA), OCT, and OCTA. FA shows signs of classic CNV (type 2) involving well-defined late leakage. ICGA shows hyperfluorescence at the site corresponding to the neovascular complex, and OCT shows the neovascular tissue above the RPE.2 Another tomographic finding is the pitchfork sign, which is characterized by vertical hyperreflective projections from the neovascular complex towards the innermost layers of the retina.6 This sign may be present only in cases of inflammatory CNV and allows its differentiation from idiopathic or myopic CNV. Furthermore, type 2 CNV is associated with intraretinal fluid, which is easily detectable on OCT.7 OCTA may be useful in distinguishing between CNV and inflammatory lesions, especially in cases of punctate inner choroidopathy (PIC) and multifocal choroiditis (MFC).8
The leading causes of CNV in uveitis are shown in Table 1. CNV may occur in up to 40% of cases of PIC, in 25%–35% of cases of MFC, and in 15%–35% of cases of serpiginous choroiditis. Previous studies have shown that CNV may occur in up to 19% of cases of ocular toxoplasmosis over time.3,9-12
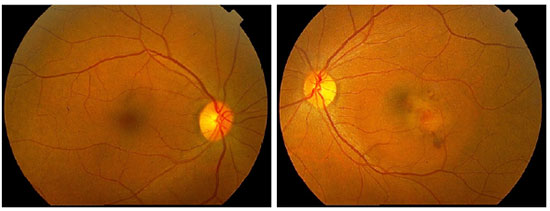
No studies to date provided strong evidence of the effectiveness of treatments of CNV in uveitis. The proposed treatment modalities include observation, surgical removal, laser photocoagulation, intravitreal corticosteroid therapy, photodynamic therapy (PDT), intravitreal injection of anti-VEGF agents, systemic control of intraocular inflammation, and combined therapy. Although the spontaneous resolution of CNV may occur, observation is not recommended because in 75% of untreated patients visual acuity decreases to 20/100.2,13 Surgical removal is possible because the neovascular complex is usually located above the RPE. Therefore, surgery may be performed with relative preservation of the RPE and choriocapillaris. Surgical treatment of CNV is currently in disuse because of the advent of anti-VEGF agents but may be reserved to large and juxtadiscal neovascular complexes, with some studies showing that the surgical results were satisfactory.14,15 Laser photocoagulation may be used in cases of extrafoveal CNV; however, its use should be avoided in cases in which the CNV is juxtafoveal because of the risk of scar expansion after treatment.16 Several studies demonstrated the efficacy of PDT, associated or not with intravitreal corticosteroid therapy, in treating CNV secondary to inflammatory diseases.2 However, with the advent of anti-VEGF agents, PDT has been less frequently used in these cases. In fact, the three currently available antiangiogenic drugs (bevacizumab, ranibizumab, and aflibercept) are safe and effective in treating this type of CNV.17-19 Type 2 CNV is usually smaller and more sensitive to anti-VEGF agents when treatment is instituted early compared with type 1 CNV. Moreover, fewer injections are required for the regression of neovascular complex in these cases.7 Figures 1, 2, and 3 illustrate one case of CNV secondary to dengue, with anatomic and functional improvement after three intravitreal injections of ranibizumab. However, the best treatment regimen or whether cases of CNV secondary to uveitis present a better response to a particular drug are unknown to date. In these cases, antiangiogenic treatment may benefit from future advances in the study of exudative AMD treatment. It is noteworthy that in cases of CNV secondary to infectious uveitis, the treatment specific for the infection should be instituted concomitantly with the treatment of CNV.3,20 In noninfectious uveitis, the systemic control of inflammation with corticosteroid therapy or immunosuppression is critical. This approach is particularly important in cases of demonstrated activity of the underlying disease. However, even in inactive cases, subclinical inflammation may cause CNV, and systemic treatment is justified in these situations. According to some authors, systemic treatment should be the first treatment option in noninfectious cases associated with CNV. However, anti-VEGF agents play an important role in the treatment of noninfectious cases and may be used in conjunction with immunosuppression and corticosteroid therapy.3,21
REFERENCES
1. Baxter SL, Pistilli M, Pujari SS, Liesegang TL, Suhler EB, Thorne JE et al. Risk of choroidal neovascularization among the uveitides. Am J Ophthalmol. 2013;156(3):468-77.
2. D’Ambrosio E, Tortorella P, Iannetti L. Management of uveitis-related choroidal neovascularization: from the pathogenesis to the therapy. J Ophthalmol. 2014;2014:450428.
3. Neri P, Lettieri M, Fortuna C, Manoni M, Giovannini A. Inflammatory Choroidal Neovascularization. Middle East Afr J Ophthalmol. 2009;16(4):245-251.
4. Roy R, Saurabh K, Bansal A, Kumar A, Majumdar AK, Paul SS. Inflammatory choroidal neovascularization in Indian eyes: etiology, clinical features, and outcomes to anti-vascular endothelial growth factor. Indian J Ophthalmol. 2017;65(4):295-300.
5. Cordero-Coma M, Pérez E, Calleja S, García Ruiz de Morales JM. Toxoplasmic retinochoroiditis: relapse vs choroidal neovascular membrane. Arch Soc Esp Oftalmol. 2010;85(12):410-3.
6. Hoang QV, Cunningham ET Jr, Sorenson JA, Freund KB. The “pitchfork sign” a distinctive optical coherence tomography finding in inflammatory choroidal neovascularization. Retina. 2013;33(5):1049-55.
7. Freund KB, Zweifel SA, Engelbert M. Do we need a new classification for choroidal neovascularization in age-related macular degeneration? Retina. 2010;30(9):1333-49.
8. Astroz P, Miere A, Mrejen S, Sekfali R, Souied EH, Jung C, et al. Optical coherence tomography angiography to distinguish choroidal neovascularization from macular inflammatory lesions in multifocal choroiditis. Retina. 2018;38(2):299-309.
9. Bowling B. Uveitis. In: Bowling B, editor. Kanski’s clinical ophthalmology. China: Elsevier; 2016. p. 395-455.
10. Veloso CE, Schmidt-Erfurth U, Nehemy MB. Choroidal neovascularization induced by immunogenic alteration of the retinal pigment epithelium in dengue fever. Case Rep Ophthalmol. 2015;6(1):18-23.
11. Atmaca LS, Simsek T, Batioglu F. Clinical features and prognosis in ocular toxoplasmosis. Jpn J Ophthalmol. 2004;48(4):386-91.
12. Skorska I, Soubrane G, Coscas G. Toxoplasmic choroiditis and subretinal neovessels. J Fr Ophtalmol. 1984;7(3):211-8.
13. Veloso CE, Costa RA, Oréfice JL, Oréfice F. Spontaneous involution of choroidal neovascularization secondary to rubella retinopathy. Eye. 2007;21(11):1429-30.
14. Lit ES, Kim RY, Damico DJ. Surgical removal of subfoveal choroidal neovascularization without removal of posterior hyaloid: A consecutive series in younger patients. Retina. 2001;21(4):317-23.
15. Almony A, Thomas MA, Atebara NH, Holekamp NM, Del Priore LV. Long-term follow-up of surgical removal of extensive peripapillary choroidal neovascularization in presumed ocular histoplasmosis syndrome. Ophthalmology. 2008;115(3):540-545.
16. Bhende M, Ahmed AS. Management of inflammatory CNV. In: Biswas J, Majumder PD, editors. Uveitis: An Update. New Delhi: Springer; 2016. p. 108-117.
17. Mansour AM, Arevalo JF, Fardeau C, Hrisomalos EN, Chan WM, Lai TY. Three-year visual and anatomic results of administrating intravitreal bevacizumab in inflammatory ocular neovascularization. Can J Ophthalmol. 2012;47(3):269-74.
18. Korol AR, Zborovska O, Kustryn T, Dorokhova O, Pasyechnikova N. Intravitreal aflibercept for choroidal neovascularization associated with chorioretinitis: a pilot study. Clin Ophthalmol. 2017;20(11):1315-1320.
19. Rouvas A, Petrou P, Douvali M, Ntouraki A, Vergados I, Georgalas I, Markomichelakis N. Intravitreal ranibizumab for the treatment of inflammatory choroidal neovascularization. Retina. 2011;31(5):871-9.
20. Hegde S, Relhan N, Pathengay A, Bawdekar A, Choudhury H, Jindal A, Flynn HW Jr. Coexisting choroidal neovascularization and active retinochoroiditis - an uncommon presentation of ocular toxoplasmosis. J Ophthalmic Inflamm Infect. 2015;12:5-22.
21. Cerquaglia A, Fardeau C, Cagini C, Fiore T, LeHoang P. Inflammatory Choroidal Neovascularization: Beyond the Intravitreal Approach. Ocul Immunol Inflamm. 2017. 4:1-6.

Funding: No specific financial support was available for this study
CEP Approval: not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
May 15, 2018.
Accepted on:
June 13, 2018.