Elaine Fonseca Bastos Goulart1; Francisco de Paula Bueno de Azevedo2; Deborah Chein Bueno de Azevedo3; Jocimar Lanes Lima4; Telma Abdalla de Oliveira Cardoso5
DOI: 10.17545/eOftalmo/2017.109
ABSTRACT
This article presents a narrative literature review regarding the use of telemedicine related to low vision or subnormal vision in people with loss of function due to any ocular condition. The survey conducted in May 2017 collected a total of 125 articles. After the duplications were removed, 62 articles remained and four relevant articles were selected. Real-time tele-ophthalmology has the potential to reduce the costs and limitations of coverage of services associated with (traditional) face-to-face consultation. Some studies using only the basic videoconference technology present results favoring telemedicine when compared to studies with more advanced telephthalmology equipment.
Keywords: Neoplasias; Xantogranuloma Juvenil; Histiócitos.
RESUMO
Este artigo apresenta uma revisão narrativa de literatura a respeito do uso da telemedicina relacionada à baixa visão ou visão subnormal, em pessoas com perda de função devido a qualquer condição ocular. A pesquisa realizada em maio de 2017 coletou um total de 125 artigos. Após retirada das duplicações restaram 62 artigos e foram escolhidos quatro artigos relevantes. A teleoftalmologia em tempo real tem o potencial de reduzir os custos e limitações de cobertura de serviços associados à consulta presencial (tradicional). Alguns estudos utilizando apenas a tecnologia básica de videoconferência apresentam resultados que favorecem a telemedicina quando comparados a estudos com equipamento mais avançado de teleoftalmologia.
Palavras-chave: Baixa visão; Telemedicina; Deficiência Visual.
RESUMEN
Este artículo presenta una revisión narrativa de literatura en lo que se refiere al uso de la telemedicina relacionada a la baja visión o visión subnormal en personas con pérdida de función debido a cualquier condición ocular. La investigación que ha sido realizada en mayo de 2017 recolectó un total de 125 artículos. Tras el retiro de las duplicaciones, quedaron 62 artículos, de los cuales cuatro se eligieron como artículos relevantes. La teleoftalmología en tiempo real tiene el potencial de reducir los costos y limitaciones de cobertura de servicios asociados a la consulta presencial (tradicional). Algunos estudios que utilizan solamente la tecnología básica de videoconferencia presentan resultados favorables respecto a la telemedicina cuando se comparan a estudios realizados con equipo más avanzado de teleoftalmología.
Palabras-clave: Baja Visión; Telemedicina; Transtornos de la vision.
INTRODUCTION
There are an estimated 285 million people with visual impairment worldwide, and 246 million of them have low vision.1 According to the World Health Organization (WHO), a person with low vision is one who has functional impairment even after clinical and/or surgical treatment and has a visual acuity of less than 20/60 and greater than 20/400 or a visual field of less than 20o from the point of fixation in the better eye with the best correction.2
People with early-stage low vision may require less magnification, benefiting in some cases from the observer simply moving closer to the reading material. It may also be easier to use assistive technologies and to maintain more prolonged contact with the specialist, lowering or preventing stress, anxiety, or depression, which interfere with visual rehabilitation3.
Telehealth is related to activities associated with healthcare, wherein information services, technologies, and telecommunications are used for health promotion. Some studies distinguish between telemedicine and telehealth, with the former being restricted to the provision of services only by physicians.4 Telemedicine promotes access for people in remote areas where specialized healthcare is unavailable5 and can benefit people with low vision through real-time internet-based remote consultations with the ophthalmologist (teleophthalmology) as well as rehabilitation with optical, non-optical, and electronic aids (visual telerehabilitation), reducing the time and cost of transporting the visually impaired person and their companions and contributing to social inclusion.
Some teleophthalmology applications are screening for diabetic retinopathy and retinopathy of prematurity, anterior segment imaging (corneal diseases or lesions, cataract, hyphema, and uveitis), glaucoma screening, low vision consultation, and teleguidance (surgical procedures).
The aim of this study was to map the “state of the art” or “state of knowledge” of academic research on telemedicine related to low vision and to summarize relevant articles and the quantitative approach of scientific research. The method used was a non-systematic literature review, aiming to identify scientific studies on telemedicine related to low or subnormal vision in people with loss of function due to any eye condition.
METHOD
A non-systematic literature review was conducted on databases such as PubMed, MEDLINE, EMBASE, ClinicalTrials.gov (www.clinicaltrials.gov), and WHO International Clinical Trials Registry Platform (ICTRP) (www.who.int/Ictrp/search/en). No study design filter was used in the electronic searches.
The following search terms were used: “telemedicine” AND “low vision,” “teleophthalmology” AND “low vision,” “telehealth” AND “low vision,” “telerehabilitation” AND “low vision,” “e-health” AND “low vision,” “telemedicine” AND “subnormal vision,” “teleophthalmology” AND “subnormal vision,” “telehealth” AND “subnormal vision,” “telerehabilitation” AND “subnormal vision,” and “e-health” AND “subnormal vision.”
Endnote X8 was used to collect, organize, and store the references and to remove duplicate entries.
The inclusion criteria used to select the articles were as follows: a) not written by the authors of the present study to ensure neutrality and impartiality; b) based on academic studies on telemedicine in which the participants were diagnosed with low vision, as defined by WHO; c) based on studies conducted from 2005 (use of videoconferencing for patients with low vision) to 2017; d) addressing a topic related to the researched keywords; e) written in Portuguese or English, whichever language the authors are most fluent in; f) for which the authors of the present study had access to the full text; and g) based on academic studies in indexed journals.
The exclusion criteria used were a) academic studies prior to the period studied; b) academic articles wherein the objective of the study was not related to the search terms; c) articles written in languages other than Portuguese or English; d) lack of access to the full text to the authors of the present study; and e) academic studies published in non-indexed journals.
Two authors screened the titles and abstracts independently and then screened the articles in full, taking into account the eligibility criteria. Two authors were responsible for the abstracts and two others for the inclusion of the studies. There was no disagreement among the authors.
RESULTS
The survey was conducted in May 2017 and collected a total of 125 articles. After removing duplicate articles, 62 articles remained, and two authors chose four relevant articles (Figure 1), accounting for a total of four summarized articles. After reading the full text of the article, the authors were in full agreement on the selection, considering the inclusion and exclusion criteria.
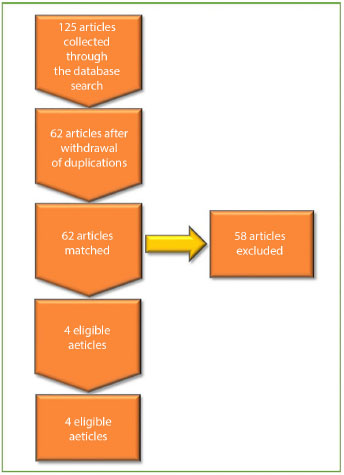
The four eligible articles are summarized in Table 1 (below).
Of these studies, Tang et al. (2005) and Ihrig (2014) made use of clinical videoconferencing (Figure 2) and visual rehabilitation (Figure 3) as follows:

DISCUSSION
Low vision due to conditions such as age-related macular degeneration and diabetic retinopathy makes traveling and driving vehicles difficult and may be a barrier preventing people with visual impairment living in distant or rural locations from having a consultation with the specialist physician and visual rehabilitation facilities.
Teleophthalmology broadens access to low-vision consultations (reducing the need to travel) and enables visual rehabilitation as early as possible, maximizing patient skills, with follow-up focused on training with optical, non-optical, and electronic aids (visual telerehabilitation).
The challenges to be faced are tests unsuitable to be performed through clinical video telemedicine (visual acuity, refraction, ocular health assessment, confrontation visual field, and others) as well as the need to develop a trained team with local primary care ophthalmologists. Teleconsultation is a possibility for health professionals in rural and remote locations using currently available technology. The effectiveness of this interaction, however, depends on the internet transmission speed, especially when needed for remote examination.10
Therefore, low vision consultation and visual telerehabilitation require the results of visual acuity examinations for both near and distance vision and both with and without the best correction, visual field tests (confrontation, either manual or computerized), and other relevant tests; current diagnoses and treatments; as well as equipment and an adequate internet speed.
Real-time teleophthalmology has the potential to reduce the costs and limitations of service coverage associated with (traditional) face-to-face consultation. Some studies using only basic videoconferencing technology11,12 are similar in terms of the results of diagnostic accuracy, which favor telemedicine when compared with studies using more advanced teleophthalmology equipment.13,14
Due to the difficulties faced by people with visual impairments without habilitation/rehabilitation and the interest in telemedicine as a means of reducing the travel barrier, enabling an increase in accessibility, future studies to explore the potential of telemedicine as a platform to provide remote services to people with low vision are promising. In addition to promoting partnerships with national and international institutions, such studies may also form collaborative networks and develop a structure of innovation and sustainability in telemedicine for solution research and development.
REFERENCES
1. World Health Organization - WHO. Visual impairment and blindness. [cited 2017 Jun 18]. Available from: http://www.who.int/mediacentre/factsheets/fs282/en/
2. World Health Organization - WHO. Vision 2020 the Right to Sight. Global Iniciative for the elimination of avoidable blidness: Action plan 2006-2011. [cited 2017 Jun 18]. Available from: http://apps.who.int/iris/handle/10665/43754
3. Gartner S, Schwartz SG, Scott IU. Collaborating with low vision specialists: Knowing when to refer to a low vision expert may enable patients with vision impairment to lead more independent, happier lives. Retina Today. 2016 Sep;74-6.
4. World Health Organization - WHO. Telemedicine. Opportunities and developments in Member States. Report on the second global survey on eHealth Global Observatory for eHealth series - Volume 2. [cited 2017 Jun 18]. Available from: http://www.who.int/goe/publications/goe_telemedicine_2010.pdf
5. Sharma LK, Rajput M. Telemedicine: socio-ethical considerations in the Indian milieu. Med Leg J. 2009;77(Pt 2):61-5.
6. Tang RA, Morales M, Ricur G, Schiffman JS. Telemedicine for eye care. J Telemed Telecare. 2005;11(8):391-6.
7. Crossland MD, Silva RS, Macedo AF. Smartphone, tablet computer and e-reader use by people with vision impairment. Ophthalmic Physiol Opt. 2014;34(5):552-7.
8. Ihrig C. Rural Healthcare Pilot Clinic: Low Vision Clinical Video Telehealth. Optometric Education. 2014;40(1):14-6.
9. Bittner AK, Wykstra SL, Yoshinaga PD, Li T. Telerehabilitation for people with low vision. Cochrane Database Syst Rev. 2015;8:CD011019.
10. Tan IJ, Dobson LP, Bartnik S, Muir J, Turner AW. Real-time teleophthalmology versus face-to-face consultation: A systematic review. J Telemed Telecare. 2017;23(7):629-38.
11. Rayner S, Beaconsfield M, Kennedy C, Collin R, Taylor P, Murdoch I. Subspecialty adnexal ophthalmological examination using telemedicine. J Telemed Telecare. 2001;7 Suppl 1:29-31.
12. Dawson E, Kennedy C, Bentley C, Lee J, Murdoch I. The role of telemedicine in the assessment of strabismus. J Telemed Telecare. 2002;8(1):52-5.
13. Tan JC, Poh EW, Srinivasan S, Lim TH. A pilot trial of tele-ophthalmology for diagnosis of chronic blurred vision. J Telemed Telecare. 2013;19(2):65-9.
14. Tanabe N, Go K, Sakurada Y, Imasawa M, Mabuchi F, Chiba T, et al. A remote operating slit lamp microscope system. Development and its utility in ophthalmologic examination. Methods Inf Med. 2011;50(5):427-34.





Funding: No specific financial support was available for this study.
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
July 25, 2017.
Accepted on:
December 6, 2017.