Sidney Julio Faria e Sousa1; Rosália Antunes Foschini2; Fernando Chahud3
DOI: 10.17545/eoftalmo/2017.104
ABSTRACT
We report a case of a juvenile xanthogranuloma in a 7-year-old girl on the corneoscleral limbus. It presented as a massive, unsightly, nodular lesion that prevented the patient from completely closing her left eye. We were able to excise the lesion completely, leading to a successful outcome. Histopathology examination with immunohistochemical staining established the diagnosis. As far as we know, this is the most extensive xanthogranulomatous limbal lesion reported in the literature.
Keywords: Neoplasms; Xanthogranuloma, Juvenile; Histiocytes.
RESUMO
Relatamos um caso excepcional de xantogranuloma juvenil em uma menina de 7 anos de idade, manifesto por uma lesão nodular antiestética de grandes proporções no limbo corneoescleral, que a impedia de fechar o olho esquerdo. O exame histopatológico e a coloração imuno-histoquímica estabeleceram o diagnóstico. São também apresentados os detalhes que levaram a um resultado bem-sucedido. Até onde chega o nosso conhecimento, esta é a maior lesão xantogranulomatosa do limbo apresentada na literatura até a presente data.
Palavras-chave: Neoplasias; Xantogranuloma Juvenil; Histiócitos.
RESUMEN
Relatamos un caso excepcional de xantogranuloma juvenil en una niña de 7 años de edad, que se ha presentado por una lesión nodular antiestética de grandes proporciones en el limbo corneoescleral, lo cual le impedía cerrar el ojo izquierdo. El examen histopatológico y la coloración inmunohistoquímica establecieron el diagnóstico. Asimismo, se presentan los detalles que llevaron a un resultado exitoso. Hasta donde llega nuestro conocimiento, ésta es la mayor lesión xantogranulomatosa en el limbo presentada en la literatura hasta la presente fecha.
Palabras-clave: Neoplasias; Xantogranuloma Juvenil; Histiocitos.
INTRODUCTION
Juvenile xanthogranuloma (JXG) is a rare granulomatous disorder characterized by proliferation and accumulation of non-Langerhans histiocytes in a variety of body tissues. It can develop at any age and in any organ system. Typically, JXG manifests as a single, sharply circumscribed, rubbery, tan-orange papule or nodule on the skin of the face, neck, or upper trunk of young children. Lesions are typically 3–10 mm in size and regress over time.1 Skin lesions rarely require treatment, although large visceral masses usually benefit from chemotherapy.2
The most frequent site of extracutaneous JXG lesions is the iris of infants, where it often causes hyphema, glaucoma, and blindness. Other sites of ocular involvement are the conjunctiva, sclera, limbus, uvea, retina, optic nerve, and orbit.3 Limbal lesions are less likely to be harmful to the eye, and they may occur over a wider age range, from childhood through adulthood.4
Histologic studies of JXG lesions demonstrate that these reactive granulomas contain giant multinucleated macrophages, lymphocytes, eosinophils, and histiocytes with foamy xanthomatous cytoplasm arranged in a storiform pattern. Touton multinucleated giant cells are characteristic of JXG and are present in 85% of cases.5 On immunohistochemistry, the majority of these cells are heavily labeled with the macrophage marker CD68 but are not immunoreactive to neuroprotein S-100 or cell surface glycoprotein CD1a, both markers of Langerhans histiocytes.6-8
We report the case of a child with a disfiguring ocular JXG of the corneoscleral limbus.
CASE REPORT
A 7-year-old girl presented with a pink-orange nodular lesion on the inferonasal corneoscleral limbus of the left eye that had been evolving over the course of 3 months. She complained of mild ocular irritation and the unsightly appearance of the lesion. The mother attributed the problem to an ocular injury from a bamboo stick that had occurred 8 months before the lesion developed. The patient had no family history of skin disorders.
Ophthalmic examination revealed a large, smooth, solid, nodular mass covered by dilated blood vessels that was firmly attached to the globe (Figure 1A, B). The lesion (14.3 × 9.6 × 8.8 mm) prevented complete closure of the left eye. Slit-lamp and funduscopic examinations were unremarkable. Visual acuity was 20/20 OD and 20/40 OS.
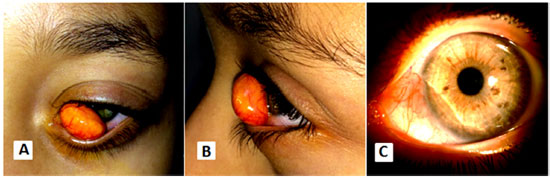
We excised the lesion from the eye under general anesthesia, leaving a thinned stromal area 2.2 mm wide in the inferonasal cornea (Figure 1C). For 3 weeks postoperatively, the patient used dexamethasone 0.1% eye drops four times daily. Pachymetry performed 2 months after surgery showed that the corneal thickness at the thinnest point of the area previously occupied by the lesion was 350 µm. Scheimpflug images obtained with a Pentacam (Pentacam, Oculus, Wetzlar, Germany) showed that the epithelial layer accounted for one-third of the corneal thickness, indicating compensatory thickening. Corneal aberrations were ten times larger in the left eye than in the right eye. Cycloplegic refraction was +1.50 −0.25 × 125 in the right eye and +0.75 −0.75 × 120 in the left eye. The best-corrected visual acuity was 20/20 in the right eye and 20/25 in the left eye.
Histologic analysis showed that the lesion had pushing margins and a well-circumscribed surface covered by a cornea-like epithelium. The nodule was walled in by a 2-mm-wide strip of stretched corneal stroma on the corneal side and by a 3-mm-wide band of conjunctival tissue on the opposite side (Figure 2A). The lesion consisted mainly of an aggregation of foamy histiocytes pervaded by multinucleated giant cells of the Touton type (Figure 2B). The histiocytes had oval nuclei with dispersed chromatin, tiny nucleoli, partially lipidized cytoplasm, and no atypia. A small number of mature lymphocytes and eosinophils were also present. Immunohistochemical tests were positive for the histiocyte markers CD68 and CD163 (Figure 2C) but negative for S-100 and CD1a. The Ki-67 proliferation index was very low (less than 3%). Gömöri’s methenamine silver stain for fungi and a Ziehl-Neelsen stain for mycobacteria were negative. These findings led to the diagnosis of JXG. On the patient’s most recent visit about 2 years postoperatively, there was no evidence of tumor recurrence.

DISCUSSION
The unusually large lesion of the present case was causing functional, visual, and cosmetic problems, requiring a prompt solution. It most closely resembled a dermoid cyst or a dermolipoma, but we discarded those possibilities because of the acquired nature of the mass. Consequently, the preoperative differential diagnosis included fibroma, neurofibroma, histiocytosis, and neoplasms of the macrophage-dendritic cell lineages.8,9 Because of the peculiarities of the case, we decided on full excision the tumor. As there was a possibility there would be no corneal tissue beneath the tumor, we ordered a donor corneoscleral button, but its use was not required.
We began the dissection of the lesion from the scleral side and had no difficulty in detaching it from the underlying sclera. We then shifted to the corneal surface and found that it adhered firmly to the stroma. It was difficult to determine the precise plane that would allow for full excision of the tumor while removing as little of the cornea as possible. Figure 2A shows the interface between the JXG lesion and the cornea in this area. Assuming that the vision of the left eye was 20/20 before the mass began growing, it is plausible that the postoperative visual acuity of 20/25 was due to surgically-induced optical aberration of the cornea. There are options other than surgery for treatment of such a lesion, including irradiation10, topical steroids11, and intralesional injection of triamcinolone acetonide12. However, we think surgical excision was the right choice, even if it indeed led to a reduction in visual acuity. The consensus in the literature is that the best treatment for JXG is simple excision or excision plus lamellar grafting.4,13
The lack of cellular atypia and the low proliferation index suggested that the lesion was benign. The immunohistochemical profile was typical of non-Langerhans histiocytes, with positivity for CD68 and CD163 but negativity for S-100 and CD1a. These results ruled out a diagnosis of Langerhans cell histiocytosis (LCH). The lesion was also negative for fungi and mycobacteria, which excluded the involvement of these infectious agents. The presence of partially lipidized cytoplasm was consistent with the short clinical history; older lesions present with more extensive lipidization.
In the presence of abnormal histiocytic proliferation, the diagnosis of JXG is good news, because the majority of these lesions are benign.4,9 LCH is the most dreaded diagnosis of a lesion resembling a xanthogranuloma. It manifests as foci of proliferating antigen-presenting histiocytes in different body tissues with potentially devastating consequences. If a lesion is diagnosed as LCH, patients should undergo a thorough clinical examination, laboratory testing, and bone and brain imaging to rule out systemic involvement.8
The presence of inflammatory and giant cells in histiocytic infiltrates of JXG suggests an inflammatory origin. Some form of local irritation would presumably have occurred to trigger the proliferation and accumulation of activated macrophages.14 Given that our patient had sustained an injury to her left eye several months before the lesion developed, it is possible that that injury led to formation of the JXG.
This case demonstrates that JXG lesions on the corneoscleral limbus may present as disfiguring, disabling nodular growths. Prompt removal of these lesions can be done efficiently as a straightforward method of diagnosis and treatment. To our best knowledge, this is the most extensive limbal xanthogramulatous lesion reported thus far in the literature.
REFERENCES
1. Lewis JR, Drummond GT, Mielke BW, Hassard DT, Astle WF. Juvenile xanthogranuloma of the corneoscleral limbus. Can J Ophthalmol. 1990;25(7):351-4.
2. Gadner H, Heitger A, Grois N, Gatterer-Menz I, Ladisch S. Treatment strategy for disseminated Langerhans cell histiocytosis. DAL HX-83 Study Group. Med Pediatr Oncol. 1994;23(2):72-80. https://doi.org/10.1002/mpo.2950230203
3. Zimmerman LE. Ocular lesions of juvenile xanthogranuloma. Nevoxanthoedothelioma. Am J Ophthalmol. 1965;60(6):1011-35. https://doi.org/10.1016/0002-9394(65)92808-4
4. Chaudhry IA, Al-Jishi Z, Shamsi FA, Riley F. Juvenile xanthogranuloma of the corneoscleral limbus: case report and review of the literature. Surv Ophthalmol. 2004;49(6):608-14. https://doi.org/10.1016/S0039-6257(04)00136-5
5. Dehner LP. Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003;27(5):579-93. https://doi.org/10.1097/00000478-200305000-00003
6. Sonoda T, Hashimoto H, Enjoji M. Juvenile xanthogranuloma. Clinicopathologic analysis and immunohistochemical study of 57 patients. Cancer. 1985;56(9):2280-6. https://doi.org/10.1002/1097-0142(19851101)56:9<2280::AID-CNCR2820560923>3.0.CO;2-L
7. Zelger B, Cerio R, Orchard G, Wilson-Jones E. Juvenile and adult xanthogranuloma. A histological and immunohistochemical comparison. Am J Surg Pathol. 1994;18(2):126-35. https://doi.org/10.1097/00000478-199402000-00002
8. Saxena T, Kumar K, Sen S, Tandon R. Langerhans cell histiocytosis presenting as a limbal nodule in an adult patient. Am J Ophthalmol. 2004;138(3):508-10. https://doi.org/10.1016/j.ajo.2004.04.029
9. Park SH, Rah SH, Kim YH. Juvenile xanthogranuloma as an isolated corneoscleral limbal mass: a case report. Korean J Ophthalmol. 2003;17(1):63-6.
10. Nordentoft B, Andersen SR. Juvenile xanthogranuloma of the cornea and conjunctiva. Acta Ophthalmol (Copenh). 1967;45(5):720-6.
11. Ashmore ED, Wilson MW, Morris WR, Hill DA, Rodriguez-Galindo C, Haik BG. Corneal juvenile xanthogranuloma in a 4-month-old child. Arch Ophthalmol. 2003;121(1):117-8.
12. Hermel M, Donner A, Remky A. New treatment option for adult-onset limbal xanthogranuloma. Cornea. 2010;29(1):113-6.
13. Kontos G, Borooah S, Khan A, Fleck BW, Coupland SE. The epidemiology, clinical characteristics, histopathology and management of juvenile- and adult-onset corneoscleral limbus xanthogranuloma. Graefes Arch Clin Exp Ophthalmol. 2016;254(3):413-20.
14. Harvey P, Lee JA, Talbot JF, Goepel JR. Isolated xanthogranuloma of the limbus in an adult. Br J Ophthalmol. 1994;78(8):657-9.



Funding: No specific financial support was available for this study.
CEP Approval: Not applicable
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
June 23, 2017.
Accepted on:
October 17, 2017.