Silvana Maria Pereira Vianello1; Isabela Vianello Valle2; Pollyana de Rezende Castilho3; Marina de Oliveira Ramalho Tarbes4; Luiz Henrique Soares Gonçalves de Lima5
DOI: 10.17545/e-oftalmo.cbo/2015.52
ABSTRACT
PURPOSE: To discuss the concepts of central serous chorioretinopathy and to suggest therapeutic recommendations in order to avoid or minimize irreversible damage to the photoreceptors by the disease.
METHODS: A literature review was conducted with the objective to compile peer-reviewed articles available on central serous chorioretinopathy. An analysis of the peer-reviewed articles and description of clinical conditions and mechanisms associated with the disease, treatment options and diagnostic tools and monitoring was made.
RESULTS: The association of the CSC disease with damage of mineralocorticoid receptors in the choriocapillaries, psychological profile and use of glucocorticoids is critical. Treatment options vary with several drugs being used, such as the mineralocorticoid antagonists. Rifampicin, finasteride, metotreaxato and propafenone represent other drugs used for the CSC treatment. Photocoagulation, micropulse laser and modified photodynamic therapy are the preferred local therapies for CSC.
CONCLUSION: This paper describes etiology, associated factors, diagnostic imaging and therapeutic management for acute, chronic and recurrent central serous chorioretinopathy.
Keywords: Pathology. Diagnosis. Physiopathology. Therapeutics
RESUMO
OBJETIVOS: Discutir os conceitos sobre coriorretinopatia serosa central e sugerir recomendações terapêuticas com o objetivo de evitar ou minimizar danos irreversíveis dos fotorreceptores pela doença.
MÉTODOS: foi realizada uma revisão da literatura com o objetivo de integrar e compilar artigos disponíveis sobre coriorretinopatia serosa central. Foi feita uma análise dos artigos e descrição das condições clinicas e mecanismos associados à doença, opções terapêuticas e recursos diagnósticos e de acompanhamento.
RESULTADOS: A associação da doença ocular com alterações nos receptores de mineralocorticoides nos capilares coroideos, perfil psicológico e uso de glicocorticoides é determinante. Opções terapêuticas são variadas e podem ser medicamentosas ou locais, estando o uso dos antagonistas de mineralocorticoides bem embasado. Outras drogas como rifampicina, finasterida, metotrexato, propafenona são discutidas e mostram vantagens limitadas. Fotocoagulação, laser micropulsado e terapia fotodinâmica modificada são as terapias locais preferenciais, com pequena diferença no resultado final. Os antiangiogênicos não tiveram sua efetividade comprovada para todas as apresentações da doença.
CONCLUSÃO: Esse artigo descreve etiopatogenia, fatores associados, diagnóstico por imagens e manejo terapêutico para a coriorretinopatia serosa central nas formas aguda, crônica e recidivada.
Palavras-chave: Patologia. Diagnóstico. Fisiopatologia. Terapia.
CENTRAL SEROUS CHORIORETINOPATHY
Definition
Central serous chorioretinopathy (CSC) is a disease characterized by the detachment of the neurosensory retina, occurring because of serous fluid buildup between the neurosensory retina and the retinal pigment epithelium (RPE), which itself controls the choriocapillaris. Fluid buildup is therefore due to a defect in RPE. (1,2,3) CSC often affects middle-aged men and is referred to as "central" because the lesion is most commonly located in the macular area. (4,5)
Symptoms
In the initial phases of the disease, patients with CSC may present with blurred vision, central scotoma, metamorphopsia, dyschromatopsia, micropsia, hypermetropization, and/or reduced contrast sensitivity. (2,5) Acute CSC is usually self-limiting, and the complete resorption of the subretinal fluid and recovery of visual acuity occur within 3 to 6 months. (2,6) However, decreased contrast sensitivity and dyschromatopsia can continue even after disease resolution. Recurrence has been reported in up to 50% of patients within 5 years. (2,4) The persistence of subretinal fluid and symptoms for more than 6 months can be defined as a chronic case of the disease. (2) Recurrent, chronic CSC has a less favorable visual prognosis and may result in permanent vision loss due to the progressive deterioration of the functions of RPE. (5)
Pathogenesis
Several factors are associated with CSC. The growing understanding of molecular events that trigger choroidal vasodilation has revealed that the impaired activation of mineralocorticoid receptors in the choroidal endothelium by aldosterone or glucocorticoids induces the upregulation of potassium channels and leads to the vasodilation and relaxation of the muscle cells of the choroidal vasculature. Therefore, choroidal thickening (or “pachychoroid”) is frequently observed in acute or chronic CSC. (3)
There is a likely association of this disease with an increase in the serum levels of endogenous and exogenous corticosteroids. (7) The aggravation of pre-existing cases of CSC and induction of CSC after treatment with glucocorticoids or after the intraocular injection of triamcinolone have all been described, information that reinforces this hypothesis. (7)
Genetic studies support the hypothesis of genetic predisposition to the disease; however, a specific pattern has not been demonstrated. (8)
Myopia, chorioretinal thinning, and atrophy in the myopic eye are all protective factors. (9)
Diagnosis
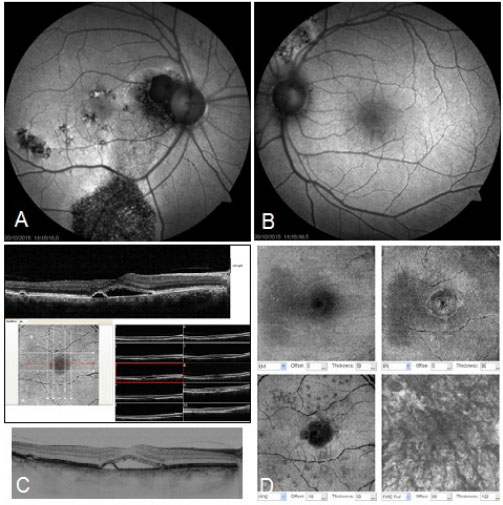
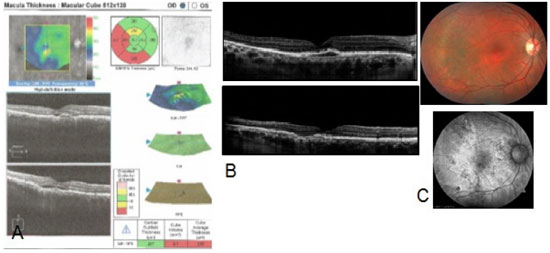
Imaging findings are important tools for diagnosing the disease and understanding its pathophysiology. The clinical examination of CSC is based on imaging findings obtained using fluorescein angiography, indocyanine green angiography, spectral domain optical coherence tomography (OCT), autofluorescence, and OCT angiography, all of which contribute to a better understanding of the disease.
Fluorescein angiography: Findings in acute CSC include the focal leakage of fluorescein through RPE, leading to the subretinal accumulation of the dye. Leak patterns observed include the “smokestack” and "inkblot”. (7) The former pattern is characterized by increased hyperfluorescence with a slight lateral diffusion, producing a mushroom-type image, whereas the latter pattern appears as a progressive increase in hyperfluorescence from a central point. These leak patterns are distributed in a wide ring-shaped area at a distance of 5 mm from the fovea. These examinations identify the initial focus of leakage in conditions involving multiple foci and also serve to guide laser treatment. (8)
Indocyanine green angiography: This is the gold standard for evaluating choroidal vasculature. The early stage is characterized by a delay in the filling of arteries and capillaries of the choroid and hypofluorescent areas. The intermediate stage is characterized by dilated veins in areas corresponding to atrophic or elevated pigment epithelium shown via OCT. Choroidal vascular hyperpermeability is represented by hyperfluorescent areas with cloudy contours. The final stage is characterized by the persistence of hyperfluorescence in the form of rings. Similar choroidal changes have been observed in more than 50% of unaffected eyes. (8) This method is useful when fluorescein angiography results seem to be normal or inconclusive. (7)
Spectral domain OCT: Changes in the choroid involve an increase in vessel diameter and thickness, which corroborates the hypothesis of increased choroidal permeability. (7) Alterações no EPR incluem presença de fissuras, hipertrofia ou atrofia comuns na doença crônica com degeneração macular cistoide. As alterações no sítio de extravasamento levam a elevação do epitélio pigmentado. Alterações na retina neurossensorial caracterizam-se por alongamento de fotorreceptores na doença aguda; cistos intrarretinianos podem se formar ao longo dos anos e depósitos sub-retinianos hi perref letivos frequentemente acumulam-se abaixo da área de descolamento. (8)
Autofluorescence: This is used to evaluate changes in RPE. The pattern observed in acute CSC includes hyperautofluorescence at the leakage site, indicating hyperfunction of RPE and an increase in the volume of the subretinal fluid. Areas of hypoautofluorescence can also be observed in acute CSC, a finding that supports the hypothesis of a focal defect in the pigment epithelium and the detachment of local cells. In contrast, hypoautofluorescence observed in chronic CSC is a sign of RPE dysfunction or atrophy. (7) The chronic pathognomonic form exhibits multiple descending tracts (gravitational tracks due to vertical and descending topography) with decreased autofluorescence, usually starting from the optic disc and macula, surrounded by a thin hyperautofluorescent contour. These tracts appear to result from continuous movements of the residual subretinal fluid. (8)
OCT angiography: This is used in the diagnosis of secondary subretinal neovascular membranes and the evaluation of the structure and flow of the choriocapillaris. It can also be useful in refractory and chronic CSC with the persistence of fluid.
Figure 1:
Treatment
A conservative approach is advisable, given the self-limiting nature of acute CSC. Patients should be periodically monitored for the resolution of neurosensory retinal detachment, which usually occurs over a period of 3 months. (2,5)
Patients under corticosteroid therapy via any route of administration should be advised of the potential benefit of interrupting treatment. Conditions such as obstructive sleep apnea, the use of phosphodiesterase type 5 inhibitors and sympathomimetic drugs, pregnancy, Cushing's syndrome, and a type A personality should be investigated during the general clinical assessment because case series have reported a correlation between CSC and these conditions. (2,10)
The use of MEK inhibitors for the control of metastatic cancer and exogenous testosterone therapy also appears to be associated with disease onset, and exogenous testosterone therapy has proved to be an independent risk factor for developing the disease. (8,11)
Despite the lack of consensus on the best approach, a range of interventions have been described, particularly for recurrent and chronic CSC. (12)
Drug Therapy
1) Mineralocorticoid Receptor Antagonists:
The introduction of a mineralocorticoid receptor antagonist (MRa) for the treatment of CSC is based on the effect of aldosterone and its receptors on pathogenic mechanisms and choroidal hyperpermeability.
The use of spironolactone and eplerenone (mineralocorticoid antagonists that act by binding to vascular mineralocorticoid receptors) has been proposed for the systemic treatment of acute and chronic CSC, with reports of significant anatomical and functional improvement in three case series, one randomized clinical trial, and one retrospective study. (13)
All groups evaluated exhibited marked improvement in subfoveal fluid volume, macular thickness, subfoveal choroidal thickness, and visual acuity, with a slower response in CSC patients with signs of descending tracts in the pigment epithelium.
The therapeutic response to mineralocorticoid antagonists observed in previous studies is consistent with the involvement of mineralocorticoids in the pathological mechanism of CSC. In addition, there was no difference in therapeutic blocking between spironolactone and eplerenone. (2,3)
Side effects were minimal; they included gynecomastia, erectile dysfunction, hyperkalemia, and changes in blood pressure levels; these symptoms were resolved after the discontinuation of therapy and were less frequent with the use of eplerenone. (2)
The criteria for contraindications of the use of MRas include pregnancy, kidney, liver or heart failure, hyperkalemia, and the use of angiotensin-converting enzyme inhibitors, anti-inflammatory non-steroidal drugs, lithium, or CYO3A4 inhibitors. (2,13)
2) Other Drug Classes:
Topical anti-inflammatory nonsteroidal agent (0.1% propafenone): The results of 26 patients treated with 0.1% propafenone versus those treated with a control indicated a statistically significant improvement in visual acuity and subretinal fluid as well as a reduction in the thickness of the choroid and central macula in the group treated with propafenone. (12) However, the differences in CSC recurrence rate between these groups were not statistically significant.
Finasteride: A review evaluated the use of finasteride for the treatment of CSC in 29 eyes and indicated improvement in visual acuity and reduction in both subretinal fluid and central macular thickness. Its use in the initial treatment of CSC was found to be safe and effective. Total disease resolution occurred in 75.9% of cases, and recurrence after discontinuation occurred in 37.5% of cases. (14)
Oral rifampicin: The effectiveness of oral treatment with rifampicin (300 mg, twice daily for 3 months) in chronic CSC with an average duration of 28.4 months was investigated in a prospective study of 14 eyes. This treatment improved visual acuity, reduced retinal and choroidal thickness, and achieved complete reduction in the subretinal fluid in 42.8% of cases and partial reduction in 64% of cases. Therefore, rifampicin has been proposed as an option for the treatment of chronic CSC. (15)
Oral methotrexate: An uncontrolled clinical study evaluated the effectiveness of oral methotrexate (7.5 mg per week for 12 weeks) in 23 eyes with symptomatic CSC and persistence of subretinal fluid for more than 3 months. There was an improvement in visual acuity, reduced average macular thickness, and complete resolution of the subretinal fluid, with disease resolution in 62% of cases. Toxicity due to the use of this medication was not observed. (16)
Topical Therapy:
Laser photocoagulation was found to be the most commonly used treatment for acute CSC. (2,4) A controlled study has demonstrated the benefits of laser treatment to shorten the neurosensory retinal detachment resolution period compared to the conservative strategy; however, this treatment proved to be ineffective in improving visual acuity and failed to decrease the recurrence rate of the disease. (17) Overall, the rate of post-treatment complications was low, and choroidal neovascularization occurred in the laser application area in fewer than 10% of cases. (8)
The effect of micropulse laser therapy with a diode or yellow laser to minimize retinal morphological changes (particularly paracentral scotoma) was also evaluated. (2) A randomized trial compared this therapeutic modality to argon laser photocoagulation and found a complete reduction in the subretinal fluid in all treated groups after 12 weeks of follow up. (18) A micropulse laser was a better option for improving contrast sensitivity and reducing the scotoma in the treated area.
Photodynamic therapy with verteporfin: This has been used for the treatment of acute, chronic, and recurrent CSC. It is believed that it primarily acts on the pathogenesis of choroidal vascular hyperpermeability. (2,4,19) Previous studies have reported good outcomes, including complete resolution of neurosensory retina displacement in 60% of cases as well as improved vision. (20) However, previous studies have indicated adverse events in the application of photodynamic therapy (PDT) for diffuse CSC, including leukomelanoderma in the treated area, RPE atrophy, decreased choriocapillaris perfusion, and decreased iatrogenic choroidal neovascularization. (2)
Changes in parameters involving treatment with PDT guided by indocyanine green angiography that was necessary in chronic CSC, recurrent CSC, or leakage that does not respond to conservative therapies was found to be safe and effective and have minimal adverse effects on vision. There was significant improvement among groups treated with a micropulse laser or half-fluence PDT (60% reducution when micropulse laser therapy was used versus 66.7% reduction when half-fluence PDT was used); leakage levels were also lower than control group levels (37.5%) in a comparative study for 16 weeks. These results provide evidence of the advantage of these two therapies and the similar outcomes they showed. (21,22)
A comparative study on the use of antiangiogenic intravitreal bevacizumab and modified half-fluence PDT indicated an improvement in visual acuity using both therapies; the rate of recurrence did not significantly differ between the two. Antiangiogenic therapy seems to be an option for treating CSC. However, other studies have not supported these findings and have, in fact, indicated the superiority of modified PDT in light of complete reduction in the subretinal fluid in 88.9% of cases compared to 12.5% of cases in the bevacizumab-treated group.
When compared to simple patient observation, the use of antiangiogenic ranibizumab provided a more rapid absorption of the fluid in all cases and reduced the risk of degeneration of photoreceptors and long-term visual loss. However, in acute CSC, the therapeutic effect was similar to that in a simple observation. In other words, the use of ranibizumab appears to be effective in chronic, recurrent, and refractory CSC.
3) Other Therapies:
Eradication of Helicobacter pylori in acute CSC patients decreased the duration of the disease to 3 months and increased visual acuity; in addition, it decreased the frequency of relapses, scotoma, and metamorphopsia in the long term. The rate of recurrence was 45.6%. These findings indicate the benefits of providing treatment for acute CSC patients. (23)
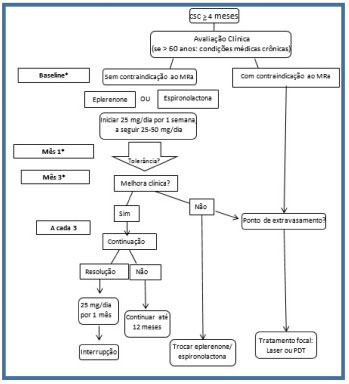
CSC: central serous chorioretinopathy. MRa: mineralocorticoid receptor antagonist. *Monitoring serum potassium levels. Adapted from Daruich A; Transl Vis Sci Technol. 2016 Mar 4;5(2):2.
Figure 3:
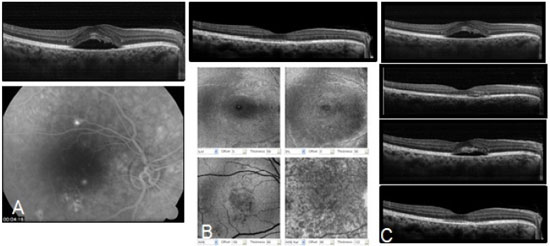
Figure 4:
CONCLUSION
Therapeutic approaches to CSC are challenging. Despite the relatively benign course of CSC, its recurrent and chronic nature is not well understood. Treatment aims to shorten the course of the disease, minimize irreversible damage, control relapses, and prevent chronicity. The suggested therapeutic strategies attempt to simplify the management of CSC; however, a detailed analysis of imaging tests may indicate the need for the use of other approaches on a case-by-case basis.
REFERÊNCIAS
1. Putnam CM, Vang SS. Modified Photodynamic Therapy Treatment of Central Serous Chorioretinopathy. Optom Vis Sci [Internet]. 2016 Apr 7 [cited 2016 May 8]; http://doi.org/10.1097/OPX.0000000000000864
2. Iacono P, Battaglia Parodi M, Falcomatà B, Bandello F. Central Serous Chorioretinopathy Treatments: A Mini Review. Ophthalmic Res [Internet]. 2015 Jan [cited 2016 May 8];55(2):76-83. http://doi.om/10.1159/000441502
3. Daruich A, Matet A, Dirani A, Gallice M, Nicholson L, Sivaprasad S, et al. Oral Mineralocorticoid-Receptor Antagonists: Real-Life Experience in Clinical Subtypes of Nonresolving Central Serous Chorioretinopathy With Chronic Epitheliopathy. Transl Vis Sci Technol [Internet]. 2016 Mar [cited 2016 May 8];5(2):2. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4782825/7toohpmcentrez
4. Abouammoh MA. Advances in the treatment of central serous chorioretinopathy. Saudi J Ophthalmol Off J Saudi Ophthalmol Soc [Internet]. Jan [cited 2016 May 8];29(4):278-86. http://doi.org/10.1016/i.siopt.2015.01.007
5. Wang M, Munch IC, Hasler PW, Prünte C, Larsen M. Central serous chorioretinopathy. Acta Ophthalmol [Internet]. 2008 Mar [cited 2016 Apr 19];86(2):126-45. http://doi.org/10.1111/j.1600-0420.2007.00889.x
6. Ross A, Ross AH, Mohamed Q. Review and update of central serous chorioretinopathy. Curr Opin Ophthalmol [Internet]. 2011 May [cited 2016 May 8];22(3):166-73. http://doi.org/10.1097/ICU.0b013e3283459826
7. Liegl R, Ulbig MW. Central serous chorioretinopathy. Ophthalmol J Int d'ophtalmologie Int J Ophthalmol Zeitschrift fur Augenheilkd [Internet]. 2014 Jan [cited 2016 Feb 9];232(2):65-76. http://doi.org/10.1159/000360014
8. Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog Retin Eye Res [Internet]. 2015 Sep [cited 2016 Mar 16];48:82-118. http://doi.org/10.1016/i.preteyeres.2015.05.003
9. Manayath GJ, Arora S, Parikh H, Shah PK, Tiwari S, Narendran V. Is myopia a protective factor against central serous chorioretinopathy? Int J Ophthalmol [Internet]. 2016 Jan [cited 2016 May 8];9(2):266-70. http://doi.org/10.18240/¡¡o.2016.02.16
10. Fraunfelder FW, Fraunfelder FT. Central serous chorioretinopathy associated with sildenafil. Retina [Internet]. 2008 Apr [cited 2016 May 8];28(4):606—9. http://doi. org/10.1097/IAE.0b013e31815ec2c8
11. Nudleman E, Witmer MT, Kiss S, Williams GA, Wolfe JD. Central serous chorioretinopathy in patients receiving exogenous testosterone therapy. Retina [Internet]. 2014 Oct [cited 2016 May 8];34(10):2128-32. http://doi.org/10.1097/IAE.0000000000000198
12. Salehi M, Wenick AS, Law HA, Evans JR, Gehlbach P. Interventions for central serous chorioretinopathy: a network meta-analysis. Cochrane database Syst Rev [Internet]. 2015 Jan [cited 2016 May 8];12:CD011841. http://doi.org/10.1002/14651858.CD011841.pub2
13. Ghadiali Q, Jung JJ, Yu S, Patel SN, Yannuzzi LA. CENTRAL SEROUS CHORIORETINOPATHY TREATED WITH MINERALOCORTICOID ANTAGONISTS: A ONE-YEAR PILOT STUDY. Retina [Internet]. 2016 Mar [cited 2016 May 8];36(3):611-8. http://doi.org/10.1097/IAE.0000000000000748
14. Moisseiev E, Holmes AJ, Moshiri A, Morse LS. Finasteride is effective for the treatment of central serous chorioretinopathy. Eye (Lond) [Internet]. 2016 Apr 8 [cited 2016 May 8]; http://doi.org/10.1038/eye.2016.53
15. Shulman S, Goldenberg D, Schwartz R, Habot-Wilner Z, Barak A, Ehrlich N, et al. Oral Rifampin treatment for longstanding chronic central serous chorioretinopathy. Graefe's Arch Clin Exp Ophthalmol = Albr von Graefes Arch fur Klin und Exp Ophthalmol [Internet]. 2016 Jan [cited 2016 May 8];254(1):15-22. http://doi.org/10.1007/s00417-015-2989-z
16. Abrishami M, Mousavi M, Hosseini S-M, Norouzpour A. Treatment of Chronic Central Serous Chorioretinopathy with Oral Methotrexate. J Ocul Pharmacol Ther [Internet]. 2015 Oct [cited 2016 May 8];31(8):468-75. http://doi.org/10.1089/jop.2014.0173
17. Lim JW, Kang SW, Kim Y-T, Chung SE, Lee SW. Comparative study of patients with central serous chorioretinopathy undergoing focal laser photocoagulation or photodynamic therapy. Br J Ophthalmol [Internet]. 2011 Apr [cited 2016 Apr 13];95(4):514-7. http://doi.org/10.1136/bjo.2010.182121
18. Verma L, Sinha R, Venkatesh P, Tewari HK. Comparative evaluation of diode laser versus argon laser photocoagulation in patients with central serous retinopathy: a pilot, randomized controlled trial [ISRCTN84128484]. BMC Ophthalmol [Internet]. 2004 Jan [cited 2016 May 8];4:15. http://doi.org/10.1186/1471 -2415-4-15
19. Ober MD, Yannuzzi LA, Do D V, Spaide RF, Bressler NM, Jampol LM, et al. Photodynamic therapy for focal retinal pigment epithelial leaks secondary to central serous chorioretinopathy. Ophthalmology [Internet]. 2005 Dec [cited 2016 May 8];112(12):2088-94. http://doi.org/10.1016/j.ophtha.2005.06.026
20. Yannuzzi LA, Slakter JS, Gross NE, Spaide RF, Costa DLL, Huang SJ, et al. Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina [Internet]. 2003 Jun [cited 2016 May 8];23(3):288-98. http://www.ncbi.nlm.nih.gov/pubmed/12824827
21. Kretz FTA, Beger I, Koch F, Nowomiejska K, Auffarth GU, Koss MJ. Randomized Clinical Trial to Compare Micropulse Photocoagulation Versus Half-dose Verteporfin Photodynamic Therapy in the Treatment of Central Serous Chorioretinopathy. Ophthalmic Surg Lasers Imaging Retina [Internet]. 2015 Sep [cited 2016 May 8];46(8):837-43. http://doi.org/10.3928/23258160-20150909-08
22. Tseng C-C, Chen S-N. Long-term efficacy of half-dose photodynamic therapy on chronic central serous chorioretinopathy. Br J Ophthalmol [Internet]. 2015 Aug [cited 2016 May 8];99(8):1070-7. http://doi.org/10.1136/bjophthalmol-2014-305353
23. Zavoloka O, Bezditko P, Lahorzhevska I, Zubkova D, Ilyina Y. Clinical efficiency of Helicobacter pylori eradication in the treatment of patients with acute central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol [Internet]. 2016 Mar 16 [cited 2016 May 8]; http://doi.org/10.1007/s00417-016-3315-0




Fonte de financiamento: declaro não haver.
Conflicts of interest: The authors declare that there are no conflicts of interest associated with this publication
Received on:
May 9, 2016.
Accepted on:
May 11, 2017.