Hélia Soares Angotti
DOI: 10.17545/e-oftalmo.cbo/2015.44
The pathogenesis of pterygium is strongly correlated with ultraviolet light exposure, dryness, chronic inflammation, and wind and dust exposure. Substances that cause irritation are also considered predisposing factors for the elastic degeneration of stromal collagen and subepithelial fibrovascular tissue.
The prevalence of this condition progressively increases toward the equator line.
The medical community and literature consider conjunctival transplantation the best surgical method for the correction of pterygium. Here we report the experience of our research team in performing amniotic membrane grafting in approximately 6,000 cases since 1996. The advantages of this method include sparing of the patient's conjunctiva, the achievement of a recurrence rate similar to that with free conjunctival transplantation ± 4%, an aesthetic appearance similar to or better than that with transplantation, and the continuous supply of amniotic tissue. The techniques used in the past 4 years include parabulbar anesthesia with L-bupivacaine, wide excision of the pterygium body, removal of the pterygium head via dissection or pulling out, application of mitomycin 0.02% for 2 min, thorough washing of the area with saline, and use of glue to fix the amniotic membrane patch.
Cases of primary, recurrent, or extensive pterygium, as well as double pterygium (nasal or temporal), which require the use of a large amount of tissue, are easily corrected with amniotic membrane patches but cannot be treated with conjunctival patches because of the amount of tissue required.
Amniotic membrane patches are prepared using placentas obtained from cesarean deliveries in patients who received full prenatal care and who were tested for hepatitis, syphilis, and HIV. The patches are placed onto pieces of filter paper and stored in a refrigerator, soaked in a solution of antibiotic and glycerin 100%, and later hydrated with either saline or Ringer's solution during surgery. The amniotic membrane should be placed on the stromal side of the eye surface (graft), and this surface can serve as a basal membrane for the growth of new conjunctival tissue, with a template indistinguishable from that of the normal conjunctiva.
The postoperative procedures include the use of occlusive dressing as well as eyedrops and a topical steroid-antibiotic combination for 3 days, and the use of eyedrops and a topical combination for 1 week after dressing removal.
The controversies in pterygium surgery include the following:
Anesthesia: The types include retrobulbar, peribulbar, parabulbar (our recommendation), subconjunctival, topical, and general anesthesia. After years of testing multiple modalities, we have demonstrated that parabulbar anesthesia using 3 mL of L-bupivacaine without additives yields a little more comfort in the postoperative period characterized by intense symptoms.
Postoperative period: We use nonsteroidal anti-inflammatory drugs in conjunction with paracetamol/codeine, oral dipyrone (every 4 hours), and an occlusive dressing with a topical steroid-antibiotic combination for 3 or 4 days, after that, the dressings are removed, and the eye drops and topical combination are used for 7 days. Subsequently, only a lubricant and a low-penetration corticosteroid, such as Fenometalona or loteprednol etabonate, are used.
Glue or sutures: The use of glue or sutures for the fixation of patches (conjunctival and amniotic) is controversial. The sole use of glue, preferably Tissucol® (a combination of fibrinogen, aprotinin, and thrombin from Baxter®), for 3 years has yielded the best results. However, we used nylon 10-0 sutures for several years before using glue. Some surgeons use four stitches in addition to glue; however, our experience dictates that suturing is not required when the amniotic membrane is glued.
Amniotic membrane: The amnion, is the inner portion of the amniotic membrane and has an avascular stromal matrix. The amniotic membrane has a composition similar to that of the conjunctiva, and it is considered an ideal substrate to ensure the growth of conjunctival tissue, as well as to support a conjunctival patch in cases where frequent recurrence demands full-fledged surgical treatment.
Amniotic tissue is used to reconstruct the conjunctiva in pterygium exeresis and other conjunctival lesions because it facilitates epithelization, does not change the phenotype of the conjunctiva, reduces inflammation, and stimulates vascularization and scarring, which are critical events after pterygium surgery. It is also important to note the easy availability of this tissue and the possibility of preservation of the conjunctiva for other procedures, including conjunctival flap covering and glaucoma surgery; in addition, the use of this tissue yields excellent aesthetic and functional results and a low recurrence rate.
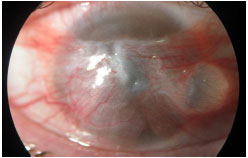
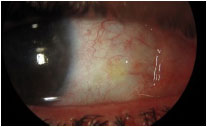
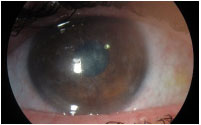
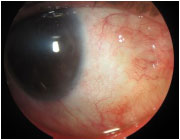
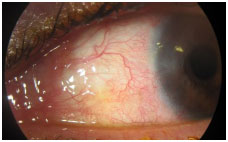
Figures 1 to 8 show a case of extensive pterygium, which covered the cornea of both eyes, albeit the left eye less extensively, and the outcome.



Funding source: none declared.
Research Ethincs Committee Opinion: N/A.
Conflicts of interest: the authors declare no conflicts of interest associated with this study.
Received on:
February 4, 2016.
Accepted on:
February 11, 2016.