Ana Luisa Romero Braga1; Cesar Pereira de Araujo2; Arnaldo Furman Bordon2
DOI: 10.17545/eOftalmo/2024.0019
ABSTRACT
Retinal vein occlusion is the second most common retinal vascular disease and is an important cause of poor vision. Retinal vein occlusion is subdivided into branch retinal vein occlusion and central retinal vein occlusion. A retrospective study by the IRIS registry showed a global prevalence of central retinal vein occlusion of 4.67 million (0.13%) in people between 30 and 89 years old. Only 0.5% of the cases were <25 years old, 2.7% between 25 and 45 years old, and 24.3% between 45 and 65 years old. The etiology, pathogenesis, treatment, clinical presentation, and prognosis of young and elderly patients with central retinal vein occlusion are different. Therefore, the diagnosis and treatment of central retinal vein occlusion depend on the patient's characteristics and risk factors. The etiology and severity of the disease should be identified as early as possible for immediate treatment in young patients. We present a central retinal vein occlusion case in a healthy young patient presented with subhyaloid hemorrhage without neovascularization.
Keywords: Retinal vein occlusion; Retinal vein; Retinal diseases.
RESUMO
A oclusão de veia retiniana é a segunda doença vascular retiniana mais comum e é uma importante causa de baixa de visão. A oclusão de veia retiniana é subdividida em oclusão de ramo da veia da retina e oclusão de veia central da retina (OVCR). Um estudo retrospectivo do IRIS registry mostrou prevalência global da oclusão de veia central da retina de 4,67 milhões (0,13%) em pessoas com idade entre 30 e 89 anos. Apenas 0.5% dos casos tinham menos de 25 anos, 2.7% entre 25 e 45 anos, 24.3% entre 45 e 65 anos. A etiologia, patogênese, tratamento, quadro clínico apresentado e prognóstico entre pacientes jovens e idosos com oclusão de veia central da retina são diferentes. Assim, o diagnóstico e o tratamento da oclusão de veia central da retina devem depender das características e dos fatores de risco do paciente. Idealmente, a etiologia e a gravidade da doença devem ser identificadas o mais cedo possível para o início imediato do tratamento direcionado em pacientes jovens. Apresentamos um caso de oclusão de veia central da retina em um paciente jovem saudável cursando com hemorragia sub-hialoidea sem neovascularização associada.
Palavras-chave: Oclusão de veia retiniana; Veia retiniana; Doenças retinianas.
INTRODUCTION
Retinal vein occlusion (RVO) is the second most common retinal vascular disease and is an important cause of poor vision1. RVO is subdivided into branch RVO (BRVO) and central RVO (CRVO)1. A retrospective study by the IRIS registry showed epidemiological analyses indicating that the global prevalence of RVO, BRVO, and CRVO reached 28.06 (0.77%), 23.38 (0.64%) and 4.67 million (0.13%), respectively, in people between 30 and 89 years old in 2015, whereas the five groups combined and the 10-year cumulative incidences of RVO were 0.86% and 1.63%, respectively2. Only 0.5% of the cases were <25 years old, 2.7% between 25 and 45 years old, 24.3% between 45 and 65 years old, and 70.3% between 65 and 85 years old (forming the largest group), and 2.2% for ≥85 years old due to the low number of registrations on the platform analyzed2.
The etiology of CRVO is multifactorial. Systemic arterial hypertension, diabetes mellitus, hyperlipidemia, and vascular diseases are important risk factors in patients >50 years old3. In young adults, it includes less common causes such as hypercoagulable status, hyperviscosity syndromes, and diseases related to infectious or noninfectious vasculitis4. Hypercoagulability is frequently reported as a risk factor in young adults, particularly due to the increased prevalence of resistance to activated protein C and deficiency of anticoagulant proteins, such as C, S, and antithrombin III5. High levels of homocysteine and anticardiolipin antibodies are also considered factors for venous thrombosis in these patients6. Other associated risk factors are collagen vascular diseases, such as systemic lupus erythematosus, sarcoidosis, and systemic vasculitis7.
One study has reported an association of CRVO in young people with primary open-angle glaucoma, ocular hypertension, pigmentary glaucoma, and pigment dispersion syndrome8. The prevalence of glaucoma and CRVO in patients in this age group has been reported to be lower than in older patients, ranging from 0% to 7%8. Diurnal fluctuation in intraocular pressure has been found in these patients who developed CRVO, and abnormal intraocular pressure may be an important risk factor8.
The condition presented in young adults has been reported to be, in most cases, mild and nonischemic, with good visual outcomes, in addition to patients presenting a good general state of health during follow-up9. However, some authors have reported that CRVO in young people does not necessarily have a mild presentation and may be associated with a poor visual prognosis and associated systemic diseases10,11.
This study aimed to report a CRVO case in a young patient presented with subhyaloid hemorrhage without neovascularization.
CASE REPORT
The patient was male, white, 27 years old, complaining of sudden and painless loss of visual acuity (VA) in the right eye (OD) for 1 day. He had no history of ophthalmological or systemic diseases, trauma, physical exertion, or use of illicit and legal substances, such as medications, supplements, and weight loss drugs.
VA was 20/200 in the OD and 20/20 in the left eye (OS). The anterior segment was normal in both eyes (OU). Fundus examination in the OD showed a blurred optic disc, venous engorgement in the four quadrants, increased vascular tortuosity, flame-shaped hemorrhages, dot and blot hemorrhages and Roth spots in the four quadrants, macula edema, and subhyaloid hemorrhage in the nasal quadrant (Figure 1). The OS was normal. Optical coherence tomography (OCT) showed macula edema, serous neurosensory retinal detachment, and central thickness (CST) of 869 µm (Figure 2). Fluorescein angiography (FA) showed no evidence of ischemia in areas without hemorrhage (Figure 3).
Laboratory tests were as follows: blood glucose and lipid levels, platelet count, blood count, coagulation tests, bleeding time, proteins S and C, antithrombin, homocysteine level, factor V Leiden, prothrombin, anticardiolipin antibodies and lupus anticoagulant, erythrocyte sedimentation rate, and C-reactive protein. Infectious tests were as follows: VDRL, FTA-ABS, anti-HIV, anti-bartonella, and toxoplasmosis IgG and IgM; all tests were normal. The patient underwent a cardiological evaluation: analysis of blood pressure values, carotid Doppler ultrasound, electrocardiogram, and echocardiogram; all tests were within normal limits.
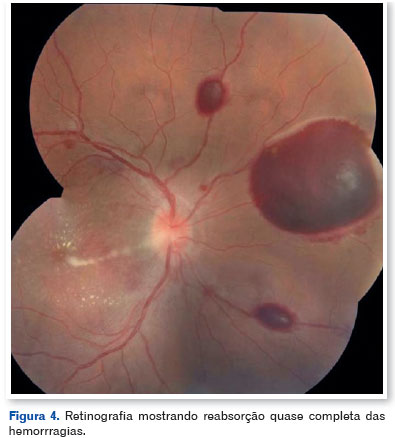
The patient was treated with three consecutive monthly injections of bevacizumab (off-label use), starting at 72h after initial care and diagnosis and 96h after the onset of symptoms. Five months after the onset of the symptoms, VA was 20/30 in the OD, and there was an almost complete resorption of hemorrhages (Figure 4). Fundus exam at the last follow-up did not demonstrate the presence of neovessels after complete absorption of hemorrhages. The CST was 172 µm, with reduced thickness of the neurosensory retina in the nasal fovea and slight disruption of the ellipsoid zone on the nasal side of the foveola (Figure 5).
DISCUSSION
Subhyaloid macular bleeding is a very rare complication caused by the occlusion of central or branch retinal veins, vascular malformations, trauma, or Valsalva maneuvers. We report a young, healthy patient with an uncommon presentation of subhyaloid hemorrhage without neovascularization associated with central vein occlusion. In the last follow-up, the patient presented a fundus exam with no neovessels, proving their absence after the clearing of hemorrhages. Atypical central vein occlusions may be a rare cause of subhyaloid macular hemorrhage12.
Due to the differences related to CRVO risk factors between young and elderly patients, local and systemic causes must be investigated and treated promptly. Similar to elderly patients, fundus exams in young patients may show increased tortuosity and venous dilation, cystoid macular edema, multiple retinal hemorrhages, optic disc edema, neovascularization formation, and vitreous hemorrhage, among others. The diagnosis of ischemic versus nonischemic CRVO becomes very important. Clinical manifestations of the ischemic form include significant loss of VA, visual field abnormalities, retinal hemorrhage and edema, and cotton wool spots. FA showed extensive areas of nonperfused capillaries and decreased B-wave amplitude on electroretinography. The nonischemic form is the most common in young patients and presents with a milder condition, with best corrected VA (BCVA) better than 20/200, mild or absent relative pupillary defect, lower incidence of cystoid macular edema, thinner central retinal thickness, and no disruption of external limiting membrane, ellipsoid zone, and retinal pigment epithelium3,12,13.
Age is correlated with choroidal thickness. A thicker choroid in young patients may reflect an improvement in the outer retina. Therefore, an ischemic injury in young patients results in a faster recovery due to greater resistance to the initial insult, no abnormalities of retinal pigment epithelial and endothelial cells of retinal capillaries, intact blood-retinal barrier, and less release of factors, such as vascular endothelial growth factor (VEGF). The severity of the obstruction may vary in patients of different ages8.
Tests such as FA and OCT can help diagnose and monitor clinical findings and response to treatment. FA detects neovascularization and nonperfused areas in the posterior pole and peripheral retina. OCT is useful for identifying macular edema. Furthermore, it allows the evaluation of retinal layers and helps to evaluate changes in macular edema after treatment11.
Because the risk factors for CRVO in young patients are distinct, individualized therapy for different etiologies and long-term monitoring are critical. Generally, observation with regular follow-up is the best management for young patients with nonischemic CRVO with preserved vision and no associated macular edema. Patients who present macular edema with decreased VA must be treated with intravitreal injection of anti-VEGF medications or intraocular injection of steroids. Laser retinal photocoagulation can be performed in cases with extensive nonperfused areas in the retina and retinal or iris neovascularization12.
Most studies showed that young patients with CRVO have a better visual prognosis after treatment. However, Dewan et al. showed no difference in the BCVA and central retinal thickness after anti-VEGF therapy between elderly and young patients14. Koh et al. reported that baseline BCVA, severity of baseline retinopathy (amount of retinal hemorrhage and venous tortuosity), the presence of optic disc edema, and the presence or absence of diabetes were associated with visual prognosis in young patients with CRVO, with BCVA as the best predictor of good visual prognosis15.
This study described a young patient with CRVO who had the unusual finding of subhyaloid hemorrhage without neovascularization or retinal ischemia during monitoring and resolution of hemorrhages. The etiology, pathogenesis, treatment, clinical presentation, and prognosis of young and elderly patients with CRVO were different. Therefore, the diagnosis and treatment of CRVO must depend on the patient's characteristics and risk factors. The etiology and severity of the disease should be identified as soon as possible for immediate treatment in young patients.
REFERENCES
1. Yau JW, Lee P, Wong TY, Best J, Jenkins A. Retinal vein occlusion: an approach to diagnosis, systemic risk factors and management. Intern Med J. 2008;38(12):904-10.
2. Li Y, Hall NE, Pershing S, Hyman L, Haller JA, Lee AY, et al. Age, Gender, and Laterality of Retinal Vascular Occlusion: A Retrospective Study from the IRIS® Registry. Ophthalmol Retina. 2022;6(2):161-171.
3. Stem MS, Talwar N, Comer GM, Stein JD. A longitudinal analysis of risk factors associated with central retinal vein occlusion. Ophthalmology. 2013;120(2): 362-70.
4. Klein R, Klein BE, Moss SE, Meuer SM. The epidemiology of retinal vein occlusion: the Beaver Dam Eye Study. Trans Am Ophthalmol Soc. 2000;98:133-143.
5. Larsson J, Olafsdottir E, Bauer B. Activated protein C resistance in young adults with central vein occlusion. Br J Ophthalmol. 1996;80(3):200-2.
6. Lahey JM, Tunc M, Kearney J, Modlinski B, Koo H, Johnson RN, et al. Laboratory evaluation of hypercoagulable states in patients with central retinal vein occlusion who are less than 56 years of age. Ophthalmology. 2002;109(1):126-31.
7. Fong AC, Schatz H, McDonald HR, Burton TC, Maberley AL, Joffe L, et al. Central retinal vein occlusion in young adults (papillophlebitis). Retina. 1992;12(1):3-11.
8. Gupta V, Sony P, Sihota R. Bilateral retinal venous occlusion in pigmentary glaucoma. Graefes Arch Clin Exp Ophthalmol. 2005;243(7):731-3.
9. Walters RF, Spalton DJ. Central retinal vein occlusion in people aged 40 years or less: a review of 17 patients. Br J Ophthalmol. 1990;74(1):30-5.
10. Kuo JZC, Lai CC, Ong FSC, Shih CP, Yeung L, Chen TL, et al. Central retinal vein occlusion in a young Chinese population: risk factors and associated morbidity and mortality. Retina. 2010;30(3):479-84.
11. Frucht J, Yanko L, Merin S. Central retinal vein occlusions in young adults. Acta Ophthalmol (Copenh). 1984;62(5):780-6.
12. Zhang XT, Zhong YF, Xue YQ, Li SQ, Wang BY, Zhang GQ, et al. Clinical Features of Central Retinal Vein Occlusion in Young Patients. Ophthalmol Ther. 2022;11(4):1409-1422.
13. Fong ACO, Schatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol. 1993;37(6):393-417.
14. Dewan KS, Hentati F, Greenlee TE, Conti TF, Chen AX, Hom GL, et al. Age-related differences in presentation and outcomes of anti-VEGF treatment of retinal vein occlusion. Can J Ophthalmol. 2021;56(2):96-104.
15. Koh YY, Lai CC, Wu WC, Hwang YS, Chen KJ, Wang NK, et al. Baseline clinical features predict visual outcome in young patients with central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2020;258(7):1367-77.
AUTHORS INFORMATIONS |
|
 |
» Ana Luisa Romero Braga https://orcid.org/0009-0004-9650-0612 https://lattes.cnpq.br/6717821233133489 |
 |
» Cesar Pereira De Araujo https://orcid.org/0000-0002-0827-2153 https://lattes.cnpq.br/1815185382812685 |
 |
» Arnaldo Furman Bordon https://orcid.org/0000-0002-2742-2102 https://lattes.cnpq.br/3104904682273027 |
Funding: No specific financial support was available for this study.
Project number and institution responsible for the opinion of the Research Ethics Committee: CAAE: 76824223.4.0000.0088 / Hospital Oftalmológico de Sorocaba.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
March 27, 2024.
Accepted on:
June 14, 2024.