Gustavo Carvalho Pavão; Elvio Ferreira Junior
DOI: 10.17545/eOftalmo/2024.0018
ABSTRACT
This study reports on a 74-year-old woman from Guarulhos, São Paulo, who sought ophthalmic care. She reported gradual loss of visual acuity in her right eye over the past 6 months. She had undergone phacoemulsification surgery with intraocular lens implantation in her right eye approximately 8 years ago. Physical examination revealed a corrected visual acuity of 20/50 and 20/10 in the right and left eye, respectively. Furthermore, biomicroscopy of the right eye revealed a cloudy fluid between the intraocular lens and posterior capsule of the lens. Thus, a diagnosis of late capsular block syndrome was established. Consequently, she was treated through Nd-YAG laser capsulotomy. The patient reported a significant improvement in the visual acuity of her right eye after the treatment, which had increased to 20/13 with correction, and no cloudy fluid was observed on biomicroscopy.
Keywords: Lens capsule; Nd-YAG Laser; Phacoemulsification; Postoperative period; Visual acuity.
RESUMO
Relato de caso de uma paciente de 74 anos, moradora de Guarulhos-SP, que procurou atendimento oftalmológico. Ela relatou uma baixa acuidade visual progressiva no olho direito há cerca de seis meses. A paciente havia se submetido a cirurgia de facoemulsificação com implante de lente intraocular no olho direito há aproximadamente 8 anos. O exame físico revelou uma acuidade visual com correção de 20/50 no olho direito e 20/10 no olho esquerdo. A biomicroscopia do olho direito revelou um líquido turvo entre a lente intraocular e a cápsula posterior do cristalino. O diagnóstico de síndrome do bloqueio capsular tardio foi estabelecido. O tratamento consistiu em capsulotomia com laser Nd-YAG. Em seu retorno após o tratamento, a paciente relatou melhora significativa da acuidade visual do olho direito, que passou para 20/13 com correção. A biomicroscopia revelou a ausência do líquido turvo.
Palavras-chave: Cápsula do cristalino; Facoemulsificação; Período pós-operatório; Nd-YAG Laser; Acuidade visual.
INTRODUCTION
Late capsular block syndrome is a rare complication of cataract surgery with in-the-bag intraocular lens (IOL) placement, characterized by the accumulation of a cloudy fluid between the IOL and posterior capsule. Late capsular block syndrome in the late postoperative period occurs in approximately 0.18% of cases1-3.
Symptomatic patients may experience decreased visual acuity, myopia due to IOL anteriorization, and elevated intraocular pressure (IOP). Most cases can be diagnosed using at a slit lamp, by checking for the presence of cloudy fluid between the IOL and posterior capsule. Most cases require a small capsulorhexis of ≤5mm. Comparison with the contralateral eye helps with establishing a diagnosis, and anterior segment optical coherence tomography, ultrasound biomicroscopy, or Scheimpflug imaging exams can be performed for confirmatory diagnosis4,5.
Possible differential diagnoses should also be considered, including opacification of the posterior capsule, chronic endophthalmitis, and pupillary block glaucoma. In most cases, posterior capsulotomy with a neodymium-doped yttrium aluminum garnet (Nd-YAG) laser is performed, which releases the trapped fluid. However, if the posterior capsule is clear, an incision can be made in the anterior capsule for the fluid to flow into the anterior chamber. In asymptomatic cases, the approach is watchful waiting. Although the prognosis after capsulotomy is good, further steps may be required to address the cloudy fluid. Moreover, an inflammatory reaction and transient increase in IOP can occur after capsulotomy2,6,7.
This study aimed to report a case of late capsular block syndrome, showing the management and treatment process, from the patient's admission to the clinic to the resolution of the condition.
The case was analyzed based on the information collected from the medical records and participant's photographic record.
CASE REPORT
A 74-year-old woman from Guarulhos, São Paulo, attended the outpatient clinic in the ophthalmology department with complaints of gradual loss of visual acuity in her right eye, which started approximately 6 months ago. She denied any other symptoms and had no history of trauma. Her comorbidities were type 2 diabetes mellitus and dyslipidemia. Her ophthalmological history included blepharoplasty in both eyes around 10 years ago, phacoemulsification with IOL implantation in the right eye around 8 years ago, both performed in another ophthalmological service, and phacoemulsification with IOL implantation in the left eye 8 months ago, performed in this hospital complex in Guarulhos, with no complications.
Physical examination revealed uncorrected visual acuity of 20/70 in the right eye and 20/30 in the left eye.
On refraction, the right eye with +0.75 SPH -0.50 CYL 170° had a visual acuity of 20/50, whereas the left eye with +0.25 SPH -1.50 CYL 135° had a visual acuity of 20/10; IOP was 12 mmHg in both eyes.
Biomicroscopy of the right eye (Figure 1) revealed a cloudy fluid between the IOL and the posterior capsule of the lens as well as a small inferior temporal opacity. Her left eye examination was unremarkable. Fundoscopy showed both eyes with clear media, a well-defined optic nerve, vertical excavation of 0.3, a 2:3 vessel ratio, normal macula, and retina attached in all quadrants.
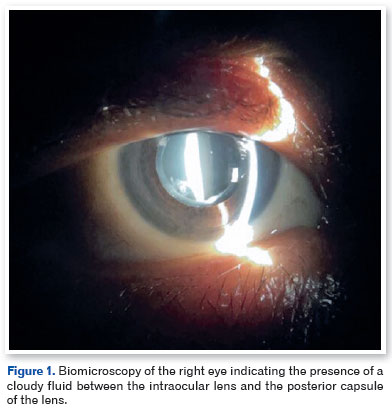
Considering the history of right-eye phacoemulsification 8 years ago and presence of cloudy fluid between the IOL and the posterior capsule on slit lamp examination, a diagnosis of late capsular block syndrome was established.
Nd-YAG laser capsulotomy was performed, and the cloudy fluid was released after two laser emissions (Figure 2). The patient was prescribed dexamethasone eye drops 0.1% every 6 hours for 5 days and brimonidine tartrate 0.2% every 12 hours for 5 days, and was to return for a follow-up in a week.
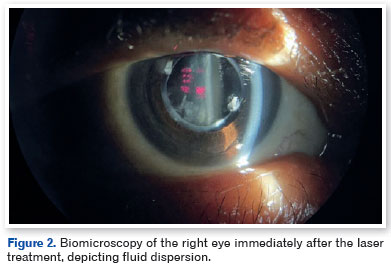
During follow-up, the patient reported a substantial improvement in her vision. Her visual acuity of the right eye without correction improved to 20/30 from the previously reported 20/70. The refraction of the right eye was +1.25 −0.50 180° with an acuity of 20/13, compared to 20/50 previously; IOP remained at 12 mmHg in both eyes.
Furthermore, biomicroscopy of the right eye no longer showed the presence of cloudy fluid. Additionally, the two sites subjected to the laser were visible. Moreover, an inferior temporal opacity was noted, but it did not affect the visual acuity.
DISCUSSION
This case emphasizes late capsular block syndrome as an uncommon but clinically relevant complication following cataract surgery with implantation of an IOL in the capsular bag. Crucial details regarding the late capsular block syndrome have been provided in the Introduction section of this study, and the Discussion will focus on the classification and pathophysiology of the disease.
In 1998 Miyake et al. proposed the following classification for capsular block syndrome: intraoperative, which occurs more frequently in polar and mature cataracts and in eyes with a longer axial length; early postoperative, which usually occurs on the first postoperative day, but can occur up to 2 weeks after surgery; and late postoperative, which tends to be a chronic phenomenon manifesting on average of 3.8 years after surgery8.
Intraoperative capsular block syndrome is highly associated with hydrodissection with high-pressure irrigation and a small capsulorhexis, which increases the risk of posterior capsule rupture2.
Capsular block syndrome in the early postoperative period is associated with incomplete removal of the viscoelastic material posterior to IOL; moreover, the risk factors for the late postoperative period are largely unknown. According to Miyaki et al., fibrosis occurs along the entire circumference of the capsular opening created by the continuous circular capsulorhexis and IOL, resulting in a chamber with milky-white fluid accumulation. Additionally, in a study by Kim et al., an association was observed with 4-haptic IOLs, specifically the Bausch + Lomb Akreos Adapt, compared to modified C-loop lenses. Another associated risk factor was an axial length of ≥25mm3.
The mechanism through which the fluid enters this cavity is still uncertain; however, there are two hypotheses. First, a study by Zacharias proposes that rapid eye movement produces a unidirectional flow into the capsular bag similar to a valve. Second, an osmotic pressure gradient created by the remaining inflammatory or cortical fibrinous material forces the fluid in3,9.
In summary, this case report highlights the importance of effective diagnosis and treatment of late capsular block syndrome after cataract surgery with IOL implantation. A 74-year-old woman with gradual loss of visual acuity in her right eye was successfully treated with Nd-YAG laser capsulotomy, and had a substantial improvement her visual acuity. This report emphasizes the need to consider this syndrome as a possible cause of visual deterioration in patients long after cataract surgery, and highlights the importance of proper diagnosis and treatment for improving the patient's quality of life.
REFERENCES
1. Cautela KA, Passos AF, Mendes AG. Síndrome do bloqueio capsular tardio - relato de dois casos. Rev Bras Oftalmol. 2014; 73(1):50-54.
2. Patel AS, Masters JS, Tripathy K, DelMonte DW, Mammo DA, Anderson D. Capsular Bag Distension Syndrome. 2023. EyeWiki, American Academy of Opthalmology
3. Kim HK, Shin JP. Capsular block syndrome after cataract surgery: clinical analysis and classification. J Cataract Refract Surg. 2008;34(3):357-63.
4. Yang HY, Kao SC, Tsai CC, Yu WK. Late capsular blockage syndrome: Clinical and anterior segment optical coherence tomography characteristics. J Chin Med Assoc. 2022;85(7):799-803.
5. Gupta K, Bhattacharjee H, Deshmukh S. Scheimpflug imaging in the late postoperative capsular bag distension syndrome. TNOA J Ophthalmic Sci Res 2019;57(4):332-3.
6. Wendrix G, Zeyen T. Late-onset capsular bag distension syndrome after cataract surgery: 2 case- reports. Bull Soc Belge Ophtalmol. 2006;(301):67-9.
7. Eifrig DE. Capsulorhexis-related lacteocrumenasia. J Cataract Refract Surg 1997;23(3):450-4
8. Miyake K, Ota I, Ichihashi S, Miyake S, Tanaka Y, Terasaki H. New classification of capsular block syndrome. J Cataract Refract Surg. 1998;24(9):1230-1234.
9. Zacharias J. Early postoperative capsular block syndrome related to saccadic-eye-movement-induced fluid flow into the capsular bag. J Cataract Refract Surg. 2000;26(3):415-9.
AUTHORS INFORMATIONS |
|
 |
» Gustavo Carvalho Pavão https://orcid.org/0000-0002-7360-1902 https://lattes.cnpq.br/2844123930995427 |
 |
» Elvio Ferreira Junior https://orcid.org/0000-0002-1438-9761 https://lattes.cnpq.br/7081972557503867 |
Funding: No specific financial support was available for this study.
Project number and institution responsible for the opinion of the Research Ethics Committee: CAAE: 73807723.3.0000.5388 by Complexo Hospitalar Padre Bento de Guarulhos (CHPBG).
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
November 10, 2023.
Accepted on:
July 30, 2024.