Pedro Faria Silveira1; Laurentino Biccas Neto2; Ana Luiza Fernandes Ottoni Porto3; Eduardo Amorim Novais4
DOI: 10.17545/eOftalmo/2024.0006
Este artigo pertence à Edição Especial Seção de Vídeo
ABSTRACT
Microperimetry enables the study of retinal sensitivity in different areas of the macula by integrating each analyzed point into color fundus images. Additionally, it enables the determination of the point of visual fixation and its stability. In this study, we discuss the importance of microperimetry in uveitis, focusing on the main diseases that have been studied to date and correlating them with the findings of the test.
Keywords: Microperimetry; Uveitis; Ophthalmology.
RESUMO
A microperimetria é um exame que permite o estudo da sensibilidade retiniana em diferentes áreas da mácula, integrando cada ponto estudado à imagem fundoscópica da retinografia colorida. Também é capaz de determinar o ponto de fixação visual e sua estabilidade. Neste trabalho, será discutida a importância da microperimetria nas uveítes, abordando as principais doenças estudadas até o momento, correlacionando com o exame e seus achados.
Palavras-chave: Microperimetria; Uveítes; Oftalmologia.
INTRODUCTION
Microperimetry (MP) assesses retinal sensitivity in different areas of the macula as well as visual fixation point and its degree of stability. Unlike other retina evaluation tests that only assess the anatomy, MP is a functional assessment technique that provides a direct correlation with the anatomical findings1. This test is known as fundus-driven perimetry because the results are applied directly to a fundus photograph. During the examination, the device follows the movements of the eye (eye tracking) in order not to interfere with the examination results. Therefore, the sensitivity of a small retinal region can be determined accurately. This test is used for a more detailed functional assessment of the macular region because visual acuity is limited to the function of central fovea, which can often be preserved until more advanced stages of various macular pathologies.
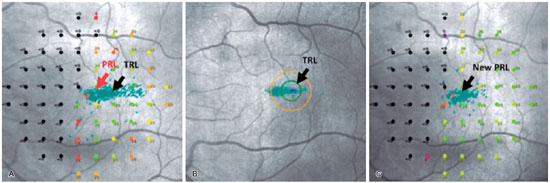
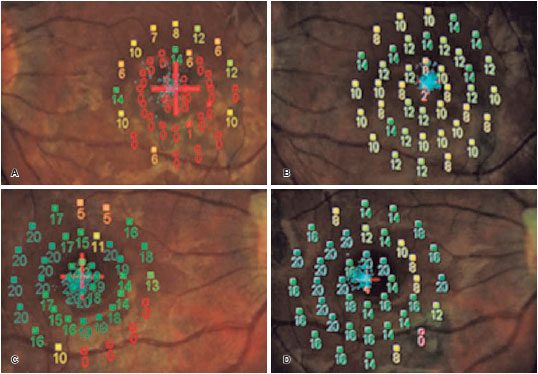
Modern MP can compensate for these limitations by repeatedly testing the sensitivity of different areas of the macular region and is useful in the following conditions: retinal dystrophies, age-related macular degeneration, macular edema, glaucoma, and uveitis. Additionally, the device conducts the visual rehabilitation technique called biofeedback, after which patients who have developed eccentric fixation due to some loss of foveal definitive sensitivity have their visual acuity improved by replacing the existing preferred retinal locus (PRL) with a trained retinal locus (TRL) that provides better visual performance (Figure 1).
This study focuses on discussing the usefulness of MP in uveitis, addressing the main diseases that have been studied to date using this test and its findings.
USEFULNESS IN DIFFERENT UVEITIC CONDITIONS
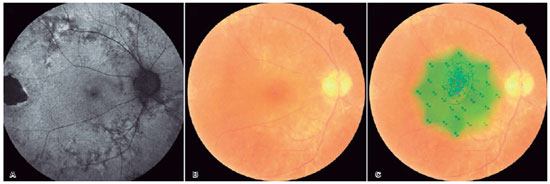
In patients with macular edema due to uveitis, foveal thickening has a significant impact on visual acuity and retinal sensitivity. Eyes with mild macular edema on optical coherence tomography (OCT), even with normal visual acuity, show reduced sensitivity, and microperimetry is useful in the early detection of visual dysfunction. The higher the amount of intraretinal fluid, the lower is the retinal sensitivity. An important previously described fact is that improvement in sensitivity is usually slower than anatomical improvement in OCT and visual acuity after treatment and resolution of the edema3. Furthermore, MP can help patients with relatively normal macular anatomy but develop low vision due to eccentric fixation (Figure 2).
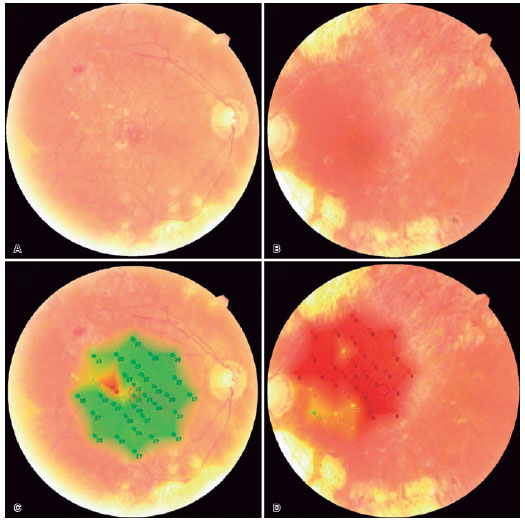
MP is also used to detect recurrence or new inflammatory foci in multifocal uveitis, such as multifocal choroiditis/PIC. It is often difficult to locate these areas of interest using fundoscopy due to the multiple lesions, which are easily identified in a pseudocolor sensitivity map. Moreover, patients with chronic vascular alterations may present low visual acuity with few clinical findings, making MP an important complementary test (Figure 3).
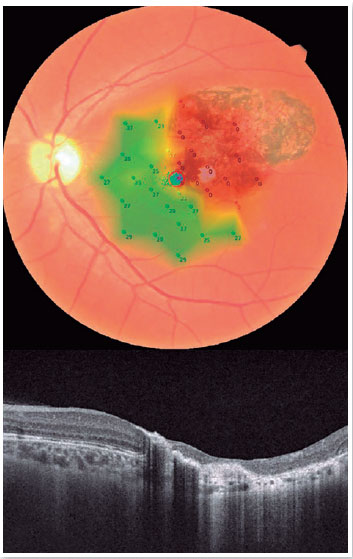
In eyes with macular scars, an important function of MP is to assess potential vision and the fixation pattern before surgical interventions such as pars plana vitrectomy or phacoemulsification with intraocular lens implantation, thereby allowing a better prognosis of vision to be established (Figure 4).
NONINFECTIOUS UVEITIS
Multiple evanescent white dot syndrome (MEWDS)
An increase in the blind spot and a decrease in central sensitivity were observed in some cases when analyzing these patients. However, these findings are not permanent as sensitivity recovers with the resolution of the disease, which is usually self-limiting within a few weeks. In these cases, the benefit of MP is also to correlate the findings with visual acuity and guide the patient's treatment. When the disease is active, patients with low central sensitivity have worse visual acuity4.
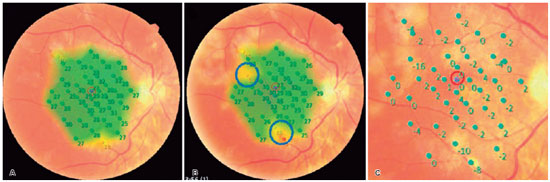
Acute posterior multifocal placoid pigment epitheliopathy
Recovery of visual acuity usually occurs within weeks to months in this pathology, although most patients have visual complaints in the healing phase. In cases where central vision remains intact, MP can be useful for the thorough assessment of residual macular dysfunction. This test shows a significant reduction in macular sensitivity at the beginning of the disease, which improves as the disease progresses. However, persistent loss of sensitivity can occur if changes in retinal structure (confirmed by optical coherence tomography (OCT)) or choriocapillary perfusion (confirmed by angio-OCT) remain in the late stages of the disease5 (Figure 5).
Birdshot chorioretinopathy
This disease is a rare cause of intraocular inflammation and predominantly affects Caucasian women. In the early stages of the disease, characteristic hypopigmented lesions may be absent or poorly defined. As the disease progresses, the lesions become more obvious and atrophic white patches appear. Although they have good central visual acuity on ophthalmological examination, patients often complain of altered color vision, night vision disturbances, and paracentral scotomas. For MP, patients usually have reduced macular sensitivity when the disease is active, which is slightly better than when inactive. However, patients with inactive disease have lower sensitivity than healthy individuals, which demonstrates that sensitivity does not fully recover after an acute condition and that can worsen with relapses and reactivations6.
Multifocal choroiditis and punctate inner choroidopathy
MP shows a significant reduction in sensitivity during the activity phase of these diseases. Depending on the severity of inflammation, photoreceptor changes can be irreversible, causing atrophic chorioretinal scarring and consequently irreversible loss of sensitivity. However, if the inflammation and damage of the outer retina and photoreceptors is mild, the sensitivity and vision of the affected area can be recovered after the end of the acute phase7. The recurrent nature of this disease makes MP a valuable tool for identifying areas of recurrence or new lesions, which can be difficult even with biomicroscopy or OCT analysis.
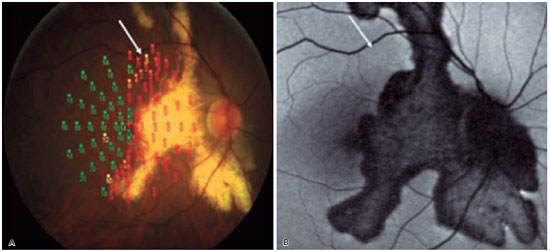
Serpiginous choroiditis
Serpiginous choroiditis is a rare condition characterized by chronic and recurrent inflammation of the choroid and retinal pigment epithelium (RPE), usually bilateral. Visual impairment is caused by primary lesions or secondary choroid neovascularization of the macular region. On MP, areas of active lesions showed reduced sensitivity (Figure 6) and areas of chorioretinal atrophy showed profound loss of sensitivity. There is a loss of relative sensitivity in the margins of the lesions. In cases in which the lesions do not affect the fovea, good sensitivity is maintained with central and stable fixation. Areas underlying the active lesion, which appear normal on fundoscopy, may show a loss of relative sensitivity (Figure 7). This may be associated with a perfusion defect in the choriocapillaris, which can be identified using indocyanine green angiography8. MP is an excellent tool for determining stability or detecting progression of the affected areas.
Behcet's disease
The duration of ocular inflammation correlates significantly with visual acuity, but not with perimetric sensitivity in the fovea or macula in this disease. Perimetric sensitivity is generally more preserved than visual acuity after repeated eye inflammation. Importantly, MP findings and retinal thickness do not correlate, because the disease can present with a thicker macula (in cases where there is more diffuse vasculitis with macular hyperpermeability) or a thinner one (in cases of occlusive vasculitis with an increased macular nonperfusion area)9.
Vogt-Koyanagi-Harada syndrome
This chronic, bilateral, autoimmune inflammatory disease that causes panuveitis shows a reduction in diffuse retinal sensitivity, even in eyes with recovered visual acuity, when assessed by MP. Persistent decrease in sensitivity may reflect dysfunction of photoreceptors attributable to subretinal fluid during the acute phase, in which multiple exudative detachments occur. This photoreceptor dysfunction may be secondary to diffuse pathological changes in the choroid or the RPE. Therefore, visual acuity assessment alone significantly underestimates the involvement of photoreceptors and the existing subclinical macular dysfunction in this disease10.
INFECTIOUS UVEITIS
Ocular bartonellosis
This disease classically presents with initial neuroretinitis with subsequent macular star formation and can have various other forms of presentation such as subretinal lesions, intermediate uveitis, and angiomatous lesions. In the acute phase, MP shows reduced sensitivity that can fully recover if treated early with appropriate antibiotic therapy11.
Ocular toxoplasmosis
In the acute stage, retinitis causes loss of sensitivity, which may persist once the condition has resolved due to the formation of a chorioretinal scar. Macular sensitivity is usually normal in cases of scarring without involvement of the macula. However, in cases of central scarring, patients present with scotoma and most develop eccentric fixation with PRL close to the edge of the scar. The use of MP and the determination of the fixation point in these patients may be important for subsequent biofeedback techniques12.
Ocular syphilis and ocular tuberculosis
In acute posterior placoid chorioretinitis (syphilis) or choroiditis (tuberculosis), a significant decrease in microperimetric sensitivity was observed at the site of inflammation, most certainly due to damage to the photoreceptor layer. If the infection is treated early and correctly, there can be a significant recovery of the ellipsoid zone and, consequently, of macular sensitivity. However, if treatment is delayed, permanent damage is possible13.
In conclusion, the importance of MP for uveitis evaluation is increasingly recognized. It is well known that, in addition to visual acuity test, several macular disorders require more precise functional assessments. MP, together with modern imaging techniques, provides numerous physiological insights into pathological macular conditions. Therefore, with advances in technology, it is believed that the test will be used more extensively, including more studies on other causes of uveitis, to help ophthalmologists diagnose, treat, and monitor their patients.
REFERENCES
1. Molina-Martin A, Perez-Cambrodi RJ, Pinero DP. Current Clinical Application of Microperimetry: A Review. Semin Ophthalmol. 2018;33(5):620-8.
2. Misawa M, Pyatova Y, Sen A, Markowitz M, Markowitz SN, Reber M, et al. Innovative vision rehabilitation method for hemianopsia: Comparing pre- and post audio-luminous biofeedback training for ocular motility improving visual functions and quality of life. Front Neurol. 2023 Apr 11:14:1151736.
3. Khochtali S, Tugal-Tutkun I, Fardeau C, Maestri F, Khairallah M. Multimodality Approach to the Diagnosis and Assessment of Uveitic Macular Edema. Ocul Immunol Inflamm. 2020;28(8):1212-22.
4. Boscarino MA, Johnson TM. Microperimetry in multiple evanescent white dot syndrome. Can J Ophthalmol. 2007;42(5):743-5.
5. Scarinci F, Varano M, Parravano M. Resilience of the Photoreceptors in Posterior Multifocal Placoid Pigment Epitheliopathy Observed by Microperimetry over Time. Ocul Immunol Inflamm. 2022;30(2):379-85.
6. Giuliari GP, Pujari S, Shaikh M, Marvell D, Foster CS. Microperimetry findings in patients with birdshot chorioretinopathy. Can J Ophthalmol. 2010;45(4):399-403.
7. Munk MR, Jung JJ, Biggee K, Tucker WR, Sen HN, Schmidt-Erfurth U, et al. Idiopathic multifocal choroiditis/punctate inner choroidopathy with acute photoreceptor loss or dysfunction out of proportion to clinically visible lesions. Retina. 2015;35(2):334-43.
8. Pilotto E, Vujosevic S, Grgic VA, Sportiello P, Convento E, Secchi AG, et al. Retinal function in patients with serpiginous choroiditis: a microperimetry study. Graefes Arch Clin Exp Ophthalmol. 2010;248(9):1331-7.
9. Takeuchi M, Iwasaki T, Kezuka T, Usui Y, Okunuki Y, Sakai J, et al. Functional and morphological changes in the eyes of Behcet's patients with uveitis. Acta Ophthalmol. 2010;88(2):257-62.
10. Abu El-Asrar AM, Al-Mezaine HS, Hemachandran S, Hariz R, Kangave D. Retinal functional changes measured by microperimetry after immunosuppressive therapy in patients with Vogt-Koyanagi-Harada disease. Eur J Ophthalmol. 2012;22(3):368-75.
11. Rosa PAC, Nakayama LF, Bergamo VC, Kuroiwa DAK, de Moraes NSB. Bartonella hanselae retinitis patient evaluated with multimodal retinal exams. Int J Retina Vitreous. 2020;6(1):54.
12. Antunes-Foschini RMS, Ho W, Messias A. Eccentric fixation patterns, clinical findings, and reading speed in patients with bilateral toxoplasmic macular retinochoroiditis. Arq Bras Oftalmol. 2018;81(5):401-7.
13. Abu El-Asrar AM, Al-Mezaine HS. Anti-tuberculous therapy combined with systemic corticosteroids improves retinal sensitivity in patients with active presumed tuberculous choroiditis. Int Ophthalmol. 2010;30(5):567-76.
AUTHORS INFORMATIONS |
|
 |
» Pedro Faria Silveira http://lattes.cnpq.br/4969860864122926 https://orcid.org/0009-0004-3991-902X |
 |
» Laurentino Biccas Neto http://lattes.cnpq.br/1354359730220772 https://orcid.org/0000-0003-2047-3983 |
 |
» Ana Luiza Fernandes Ottoni Porto http://lattes.cnpq.br/2352731863516981 https://orcid.org/0000-0003-4984-5365 |
 |
» Eduardo Amorim Novais http://lattes.cnpq.br/6337616535467985 https://orcid.org/0000-0001-6790-4627 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
October 19, 2023.
Accepted on:
October 22, 2023.