Mariana Miyazi1; Kauê Marques Ferreira1; Cristiano Urbano Becker2; Maria Vitória Vicente Cardoso3; Alexandre Xavier da Costa4
DOI: 10.17545/eOftalmo/2024.0005
ABSTRACT
Keratopigmentation commonly known as corneal tattooing, is a surgical technique where micropigments of different colors are injected into the stroma to change its color, and it is an important tool for aesthetic purposes. Keratopigmentation was first recorded by the philosopher Galen several centuries ago as an aesthetic treatment strategy for patients with leukoma. In recent years, major advancements in surgical techniques and pigment quality have remarkably increased the safety and stability of these substances on the cornea, with improved aesthetic outcomes. These advances have led to the expansion of its indications as follows: (a) cosmetic effects on pathological corneas; (b) functional effects such as in cases of photophobia or diplopia due to aniridia, coloboma, and other pathologies; and (c) more recently, cosmetic effect on healthy corneas, aiming to simulate a change in eye color.
Keywords: Keratopigmentation; Corneal opacification; Leukoma treatment.
RESUMO
A ceratopigmentação, conhecida comumente como tatuagem corneana, é uma técnica cirúrgica na qual micropigmentos de diferentes cores são injetados no seu estroma, visando alterar a sua coloração, atuando como uma importante ferramenta para fins estéticos. A ceratopigmentação teve o seu primeiro registro pelo filósofo Galeno, há muitos séculos, como uma estratégia utilizada para o tratamento estético de pacientes com leucomas. Nos últimos anos, grandes melhorias foram realizadas, tanto nas técnicas cirúrgicas quanto na qualidade dos pigmentos utilizados, que aumentaram notavelmente a segurança e a estabilidade destas substâncias na córnea, bem como melhoraram o resultado estético. Tal avanço colaborou com a ampliação de suas indicações, entre elas: (a) efeito cosmético em córneas patológicas; (b) efeitos funcionais, como em casos de fotofobia ou diplopia por aniridia, coloboma e outras patologias; e (c), mais recentemente, como efeito cosmético, em córneas saudáveis, a fim de simular uma mudança na cor dos olhos.
Palavras-chave: Ceratopigmentação; Opacificação corneana; Tratamento do leucoma.
INTRODUCTION
Keratopigmentation (KTP), popularly known as corneal tattooing, is a surgical technique where micropigments of different colors are injected into the corneal stroma to change its color1.
Disfiguring corneal scars not only cause eye problems, such as low visual acuity and photophobia but also cause unaesthetic blemishes that can affect the psychosocial interactions of patients. Different treatment options such as cosmetic contact lenses and evisceration/enucleation with orbital implants and ocular prostheses are available to improve the aesthetic appearance2.
Over the years, KTP has been used for other purposes as follows: (a) cosmetic effect on pathological corneas; (b) functional effects such as in cases of photophobia or diplopia due to aniridia, coloboma, and other pathologies; and (c) more recently, cosmetic effect on healthy corneas, aiming to simulate a change in eye color3. The cosmetic effect in corneal opacities remains the most common indication, with several studies published in the international literature, but it is still relatively unknown in Brazil. KTP is a proven beneficial option as it is a minimally invasive surgical procedure with high patient satisfaction rates, low cost, and high potential accessibility4.
DISCUSSION
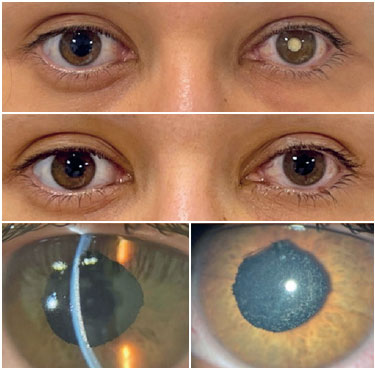
Typically, a leucomatous cornea creates a social stigma in the patient, who often seeks alternative solutions to hide this abnormality and reduce its psychological effects. However, corneas with leukoma are pathological and often intolerant of cosmetic contact lenses or ocular prostheses, and it is common for patients to complain of excessive discomfort caused by the irregular corneal surface. In addition, enucleation and evisceration surgeries are mutilating and have several adverse effects, mainly related to the prosthesis5. Considering the above discussion, KTP is a promising alternative for improving the aesthetics of patients with corneal opacities (Figure 1).

KTP techniques describe different ways of injecting pigments to the corneal stroma and, in general, can be divided into superficial and stromal, according to Jorge L Alio3,6. Superficial techniques can be divided into manual and automated, and intrastromal techniques can be divided into manual and femtosecond-assisted.
In most studies, the pigments are the same as those used in skin tattoos. In some countries, records of specific pigments being used for the cornea exist with different amounts of lactic acid, propanediol, and micronized pigments of different colors6.
According to the Brazilian legislation, the equipment and inks used in tattooing must be registered with the Health Surveillance Agency to guarantee the user's safety and avoid the use of harmful substances. The requirements for registration that must be met for the pigment to be classified as a long-term surgically implantable or invasive product are presented in Resolution RDC 55 of 20087.
In Brazil, as no pigment has been specifically registered for use on the cornea, pigments registered for staining the skin are used for KTP, as they are a Class 3 product in Anvisa's risk classification (long-term surgically implantable or invasive product)7. The pigments should preferably be of mineral origin, indelible, easily sterilizable, nonirritatable to the cornea, opaque to light, and miscible in water but not soluble in water8. With the properties mentioned above, it is possible to achieve a higher safety profile for the use of a pigment in the cornea and greater stabilization in the tissue.
Manual superficial keratopigmentation
This was one of the first techniques used in KTP before the development of automated devices. It involves the use of the tip of a sterile needle, usually a 25-G needle, covered with the pigment to be used. Next, several tangential punctures are sequentially made in the corneal stroma, similar to a micropuncture. Different colors of pigment can be used to achieve the desired effect.
Automated superficial keratopigmentation
Automated superficial KTP uses the same principle as the previous technique, i.e., staining the cornea through tangential punctures in the corneal stroma. The difference lies in the use of an electronic device that automatically performs the micropunctures (Figure 2). Depending on the device used, one can configure the length of the needle that is exposed in each puncture, the frequency of the shots, and the number of needles used in each shot. Reports indicate needles with 3–5 tips are usually used in this technique to simulate the iris and with one tip to simulate the pupil and limbal area9 (Figure 3).
Manual intrastromal keratopigmentation
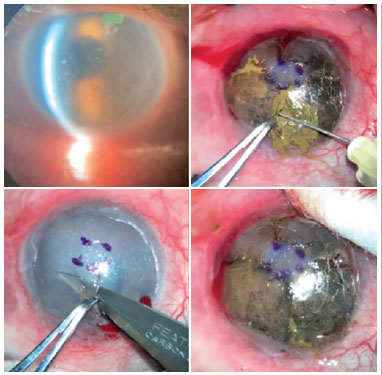
The basic concept of this technique is a superficial lamellar dissection of the cornea, with direct intrastromal application of the pigment (Figure 4). The central corneal area, which will simulate the pupil, is outlined with a dermapen, and then, a 3-mm arcuate incision is made at 10 o'clock and approximately 150 µm deep, followed by the dissection of a central pocket and the deposition of black pigment (Figure 5). To simulate the color of the iris, radial corneal incisions are made at 3, 6, 9, and 12 o'clock from the outer edge of the pupillary area dyed black to the periphery of the cornea, which are deeper, at approximately 200 µm. Then, the pigment with a color matching that of the patient's contralateral eye is deposited8. Because the dye is applied directly to the stroma, the results are more satisfactory in terms of color distribution and stability; however, complications may arise owing to the risk of irregular tissue dissection or secondary corneal perforation10.
This technique is usually quicker than the manual superficial technique and gives the pigmented cornea a natural appearance, although it requires the surgeon to possess superior surgical skills. In addition, it is associated with a less symptomatic postoperative recovery process because the surface of the cornea only has a few cuts, and the staining pigments are not exposed to the tear film11.
Femtosecond laser-assisted intrastromal keratopigmentation
In this technique, the femtosecond laser is used to create the intrastromal tunnels where the pigments are injected to simulate the color of the iris and the pupil. Alió et al. (2011) used this technique on a 25-year-old patient who reported intense photophobia and presented significant iris atrophy on physical examination, with anatomical deformation of the iris and pupil. Three months after the procedure, the patient exhibited no symptoms of photophobia and with an excellent aesthetic outcome12. However, the major challenge of using this technique is its high cost and the actual availability of the technology6,8.
With the advancement of technology, the most recent studies on KTP have shown increasingly promising aesthetic outcomes with automated and femtosecond-assisted techniques13,14. This technique is reported to be more precise and safer, based on tunnel formation and good wound healing, and it is well tolerated by patients11. However, maximum reports in literature exist on the manual superficial and intrastromal KTP techniques, showing favorable outcomes, including when used in combination8 (Figure 6). In Brazil, in the first case series recently published on the subject, eight patients answered a survey on their aesthetic satisfaction with the KTP procedure after a two-year follow-up. The survey included questions related to postoperative discomfort and the social impact following surgery with the manual intrastromal KTP technique performed either alone or in combination with the manual superficial KTP technique. All patients were extremely satisfied with the results; 75% reported minimal postoperative discomfort, and all patients reported a significant improvement in social and personal well-being8.

With regard to femtosecond-assisted KTP, recent studies have described the use of the technique in patients with healthy eyes to simulate a change in the apparent eye color10. In nonhealthy eyes, there are reports of KTP performed with this technique for situations such as correction of iris defects12, Urretz-Zavalia syndrome12, leukocoria, and corneal opacities13, with no evidence of changes in patients' vision or astigmatism11.
The surgical complications of KTP are multifactorial in origin, although they may be more related to the surgeon's learning curve. In a recent retrospective study, 234 eyes of 204 patients were evaluated for complications following the different KTP techniques. The percentage of complications regarding all procedures between 2002 and 2016 was 12.82%. Among functional complications, photophobia was the most frequent complication (49% of patients), usually occurring on the first postoperative day, but with 81% of cases resolving 6 months postoperatively. Regarding organic complications, color change over time was the most frequently reported problem (19% of patients), with an average time to color change of around 4.6 years3. However, one advantage of the KTP technique is that it allows retouching, and thus, permitting new color corrections over time.
In addition, other complications observed to a lesser extent in the published studies include neovascularization, corneal perforation, incomplete coverage of the opacity, corneal reopacification, and hypo- or hyperpigmentation. In the case series recently published by our group, no chronic complaints related to the surgery were reported, and no retouch was necessary during the 2-year follow-up8.
Histopathology
Electron microscopy images showed no granules in the extracellular matrix, demonstrating that these particles can be actively captured and retained within the cell membrane of keratocytes for a prolonged period, with studies indicating up to 61 years following surgery15.
Similar results were obtained with micronized mineral pigments, that is, no evidence of pigment effusion, color change, stromal inflammation, or corneal neovascularization was observed10. In a study focused on determining the tolerance and toxicity of the micronized mineral, using a black color obtained from iron oxide, hematoxylin-eosin (H&E) staining was used to analyze the histological sections using the standard protocol, and the histological analysis was performed using the Nikon Eclipse E400 microscope. After 3 months of follow-up, the corneal epithelium was intact, with no ulcers, erosions, or edema. No hyperplasia or atrophy was observed and the normal thickness of the epithelium was preserved (3–5 cells). In addition, the corneal stroma in pigmented eyes and controls showed no signs of stromal scarring or fibrosis. The shape of collagen fibers was maintained and no exaggerated adhesion was found between these fibers16. The histopathological examination corroborated the clinical findings in terms of inflammation. No pigment diffusion or color changes occurred throughout the study, and no cases of corneal neovascularization were noted17.
With regard to Nankeen ink particles, a study by Fujita et al.(15) showed that injecting Nankeen ink particles and polystyrene latex spheres into the corneal stroma of rabbits led to these particles undergoing endocytosis by corneal fibroblasts within 3–4 days of injection; moreover, all these particles were kept unchanged for 6 months.
Therefore, it can be concluded that KTP is a minimally invasive surgical procedure and a proven beneficial alternative for the aesthetic improvement of dysfunctional eyes, although relatively unknown in Brazil. The authors have reported excellent stability of the pigmentation pattern during follow-up, with no signs of ocular toxicity, thus deeming it a good surgical option, and the different techniques should be personalized according to each case.
Consideration should be given to the fact that disfiguring corneal opacities can damage self-confidence and self-esteem, negatively impacting the patient's quality of life. Therefore, in addition to being a functional treatment alternative, KTP should be considered an essential line of restorative treatment for these patients. Further studies should be conducted to improve KTP techniques and the materials and pigments used for corneal implants.
REFERENCES
1. Pitz S. Corneal tattooing: an alternative treatment for disfiguring corneal scars. Br J Ophthalmol. 2002;86(4):397-9.
2. Srirampur A, Kalwad A, Mansoori T, Kola P. Simple and novel technique of using lampblack soot as a corneal tattoo for disfiguring corneal opacities. Indian J Ophthalmol. 2021;69(12): 3748-51.
3. Alio JL, Al-Shymali O, Amesty MA, Rodriguez AE. Keratopigmentation with micronised mineral pigments: complications and outcomes in a series of 234 eyes. Br J Ophthalmol. 2018;102(6):742-7.
4. Karslıoğlu MZ. Keratopigmentation: Is it a miracle or an adventure? Beyoglu Eye J. 2020;5(1):32-7.
5. Bohman E, Rassmusen MLR, Kopp ED. Pain and discomfort in the anophthalmic socket. Curr Opin Ophthalmol. 2014;25(5):455-60.
6. Alio JL, Sirerol B, Walewska-Szafran A, Miranda M. Corneal tattooing (keratopigmentation) with new mineral micronised pigments to restore cosmetic appearance in severely impaired eyes. Br J Ophthalmol. 2009;94(2):245-9.
7. Brasil. Agência Nacional de Vigilância Sanitária. Resolução da Diretoria Colegiada - RDC nº 55 de 6 de agosto de 2008. Dispõe sobre o registro de produtos utilizados no procedimento de pigmentação artificial permanente da pele, e dá outras providências. Brasília, DF, agosto de 2008.
8. Xavier LDO, Becker CU, Salomão HMN, Costa AX. Ceratopigmentação (tatuagem corneana): utilização de técnicas combinadas para melhora estética em olhos de pacientes com opacidades corneanas. Rev Bras Oftalmol. 2022;81:e0031.
9. Al-Shymali O, Rodriguez AE, Amesty MA, Alió JL. Superficial Keratopigmentation: An Alternative Solution for Patients With Cosmetically or Functionally Impaired Eyes. Cornea. 2018;38(1):54-61.
10. Hasani H, Es'haghi A, Rafatnia S, Alilou S, Abolmaali M. Keratopigmentation: a comprehensive review. Eye. 2020;34(6): 1039-46.
11. D'Oria F, Abu-Mustafa SK, Alio JL. Cosmetic Change of the Apparent Color of the Eye: A Review on Surgical Alternatives, Outcomes and Complications. Ophthalmol Ther. 2022;11(2):465-77.
12. Alió JL, Rodriguez AE, Toffaha BT, Piñero DP, Moreno LJ. Femtosecond-assisted keratopigmentation for functional and cosmetic restoration in essential iris atrophy. J Cataract Refract Surg. 2011;37(10):1744-7.
13. Yin HY, Walter KA. Long-Term Outcome of Femtosecond Laser-Assisted Keratopigmentation: Using Intacs Channels for Precise Pigment Deposition Within the Cornea. Cornea. 2021;40(10):1330-5.
14. Ferreira KM, Magalhães ALP, Miyazi M, Cordeiro FM, Costa AX. Keratopigmentation and retrobulbar filling with hyaluronic acid for the aesthetic treatment of an enophthalmic blind eye. Int J Med Ophthalmol. 2023;5(2):24-27.
15. Fujita H, Ueda A, Nishida T, Otori T. Uptake of India ink particles and latex beads by corneal fibroblasts. Cell Tissue Res. 1987; 250(2):251-5.
16. Rodríguez A, Alió JL, María Amesty, Mohamed El Bahrawy. Text and Atlas on Corneal Pigmentation. Jaypee Brothers Medical Publishers (P) Ltd. eBooks. 2015.
17. Sirerol B, Walewska-Szafran A, Alio JL, Klonowski P, Rodriguez AE. Tolerance and Biocompatibility of Micronized Black Pigment for Keratopigmentation Simulated Pupil Reconstruction. Cornea. 2011;30(3):344-50.
AUTHORS INFORMATIONS |
|
 |
» Mariana Miyazi https://orcid.org/0000-0002-7665-4786 http://lattes.cnpq.br/5247882616068391 |
 |
» Kauê Marques Ferreira https://orcid.org/0009-0000-4823-7689 http://lattes.cnpq.br/3599697677705811 |
 |
» Cristiano Urbano Becker https://orcid.org/0000-0002-8982-6268 http://lattes.cnpq.br/5641845252660611 |
 |
» Maria Vitória Vicente Cardoso https://orcid.org/0000-0002-1578-8895 http://lattes.cnpq.br/5472622126304060 |
 |
» Alexandre Xavier da Costa https://orcid.org/0000-0002-9929-8358 http://lattes.cnpq.br/3978094045616220 |
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
June 24, 2022.
Accepted on:
January 21, 2024.