Gabriela Tomaz Martinho1; Guilherme Vieira Peixoto1; Caio Cezar Toledo de Conti1; Rafael Stefano Pivatto Ferro2; Roberta Pereira de Almeida Manzano2
DOI: 10.17545/eOftalmo/2023.0038
ABSTRACT
This report describes a case of choroidal neovascularization secondary to acute retinal pigment epitheliitis. Observations: A 29-year-old woman presented with acute blurring of her vision and metamorphopsia in her right eye lasting for 1 month. She had experienced a similar episode in 2017, with spontaneous resolution. Examination through ophthalmoscopy, optical coherence tomography, and optical coherence tomography angiography revealed findings indicative of choroidal neovascularization secondary to acute retinal pigment epitheliitis of the right eye. Examination of the left eye yielded normal results. The patient received two intravitreal injections of aflibercept, leading to complete resolution of the subretinal fluid and reduction of the size of choroidal neovascularization. This is the first reported case of choroidal neovascularization secondary to acute retinal pigment epitheliitis.
Keywords: Choroidal neovascularization; Acute retinal pigment epitheliitis; Retina
RESUMO
O objetivo deste estudo é relatar um caso de neovascularização de coroide secundária a epitelite pigmentar retiniana aguda. Paciente do sexo feminino, de 29 anos, apresentou baixa de visão aguda e metamorfopsia no olho direito por 1 mês. Relatou que um episódio semelhante havia ocorrido em 2017, com resolução espontânea. À oftalmoscopia, tomografia de coerência óptica e angiografia por tomografia de coerência óptica, foram observados achados semelhantes a neovascularização da coroide secundária a epitelite pigmentar retiniana aguda do olho direito. O exame do olho esquerdo apresentouse normal. A paciente foi tratada com duas injeções intravítreas de aflibercepte, com resolução total do fluido sub-retiniano e diminuição do tamanho da neovascularização da coroide. Não há uma descrição anterior semelhante de um caso de neovascularização de coroide secundária à epitelite pigmentar retiniana aguda na literatura.
Palavras-chave: Neovascularização de coroide; Epitelite pigmentar retiniana aguda; Retina
INTRODUCTION
Acute retinal pigment epitheliitis (ARPE) is a disease characterized by an idiopathic and self-limiting nature. It mainly occurs in the macular region, resulting in severe and acute central vision loss. The disease mostly affects young and healthy adults, causing retinal pigment epithelium (RPE) lesions1. ARPE regularly resolves spontaneously, frequently with full restoration of visual acuity without further structural or functional consequences1.
Patients typically complain of decreased vision, metamorphopsia, and central scotoma1. Fundus findings typically consist of a fine pigment stippling surrounded by a yellow-white hypopigmented halo in the macula2. Examination using fluorescein angiography (FA) typically shows hyper-fluorescent lesions without leakage2. Optical coherence tomography (OCT) reveals hyper-reflective accumulations (humps) involving inner band and photoreceptor outer segments, as well as disruption of the inner segment and outer segment junction of photoreceptors3. These lesions stretch from the RPE layer toward the outer nuclear layer. Diagnosis is based on symptoms, fundus findings, and complementary examinations.
Owing to its rarity, few cases of ARPE have been reported thus far4. However, choroidal neovascularization (CNV) after an ARPE episode has not been previously reported. Therefore, in this report, we describe the findings of OCT, FA, and fundus examination of a patient who developed CNV 4 years after an episode of ARPE.
CASE REPORT
A 29-year-old female patient visited the clinic for ophthalmologic evaluation due to central vision loss and metamorphopsia in her right eye lasting for 1 month. She had experienced a similar episode in 2017, with spontaneous resolution. She presented visual acuity of 20/60 and 20/20 with best correction on her right and left eye, respectively. The patient denied use of recreational drugs or exposure to laser light or sun gazing.
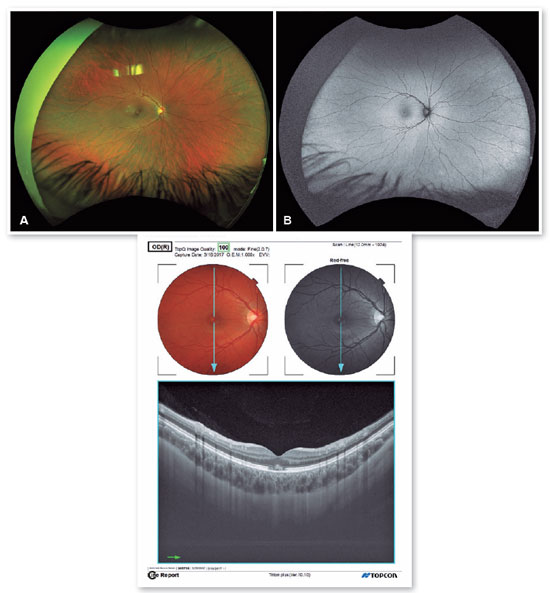
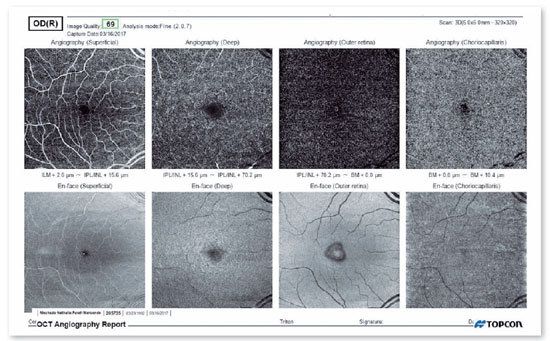
Fundus photographs captured in 2017 showed a hypopigmented round-shaped macular lesion, alongside yellow-white spots in the fovea (Figure 1A). An autofluorescence fundus image revealed irregular hyperautofluorescent areas (Figure 1B). Spectral domain OCT (SD-OCT) images showed hyper-reflective accumulations (humps), which involved the outer segment of the photoreceptor layer and inner RPE layer. Moreover, disruption of the inner segment and outer segment junction of photoreceptors was observed (Figure 1C). En face OCT showed cockade-like appearance (Figure 2), and OCT angiography performed in 2017 did not indicate CNV (Figure 2). At that time, the patient was diagnosed with ARPE, and the condition was spontaneously resolved.
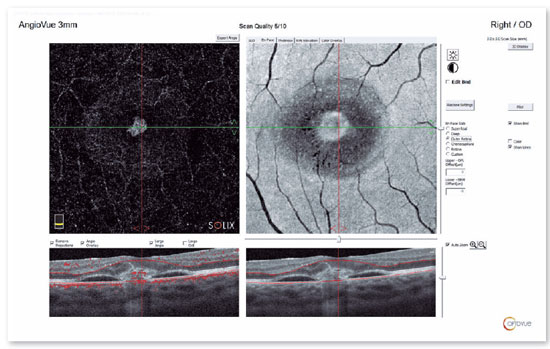
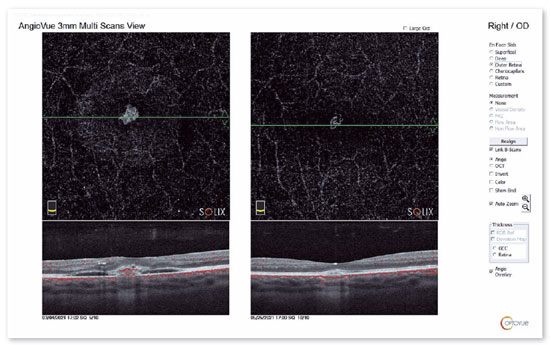
In 2021, she presented with subretinal fluid on OCT and CNV on OCT angiography (Figure 3). She was treated with two intravitreal injections of aflibercept (Eylea) for two consecutive months, resulting in complete resolution of the subretinal fluid (Figure 4), reduction of the size of CNV, and improvement of visual acuity (i.e., 20/25). At 11 months after treatment, there was no disease recurrence.
DISCUSSION
ARPE is a rare macular disease; consequently, the details of its physiopathology are unknown, warranting further investigation. In addition, the trigger factor of the disease remains unclear. Viral infection is detected in 25.9% of cases, and this may trigger the disease in some patients5. A previous study suggested a female predominance, unilateral involvement, and an excellent visual prognosis of ARPE. These findings are consistent with the case described in this article. Although uncommon, disease recurrence has been reported in one case6.
With the advancement of OCT technology, it has been demonstrated that this disease may originate from the outer retinal areas, rather than merely from the RPE4. OCT findings suggested that the initial lesion in ARPE is possibly located at the level of the photoreceptor outer segment and RPE4.The main finding in the present case was a dome-shaped hyper-reflective lesion at the photoreceptor outer segment and inner RPE layer. Our patient presented with CNV 4 years following the initial manifestation of the disease. This finding may support the speculation that ARPE is a post-inflammatory response of the outer segment of photoreceptors and the RPE.
A differential diagnosis for our case is acute fovealitis. This condition exhibits a similar ophthalmoscopic appearance to that of ARPE, with fine pigment stippling surrounded by a yellow-white hypopigmented halo in the macula; however, it is associated with different OCT findings7. On OCT, acute fovealitis appears as loss of visibility or blurring of the interdigitation and ellipsoid zones or plumes of hyper-reflectivity extending from the level of the ellipsoid zone through the outer nuclear layer and the Henle’s layer of the fovea7. These lesions resolve rapidly and are not linked to residual pigmentary changes. Therefore, it is speculated that these lesions are the result of transient inflammation exclusively of foveolar cellular components7.
Other differential diagnoses include solar retinopathy and unilateral acute idiopathic maculopathy with similar lesions or OCT findings. Solar retinopathy refers to rare ocular lesions resulting from unprotected solar gazing8. It is typically a bilateral disease, although unilateral and asymmetrical manifestations may occur. Fundus examination can show a small yellow spot at the fovea with gray granular pigmentation circling the yellow lesion8. SD-OCT may show disorganized material at the layer between the RPE and photoreceptor inner/outer segment (IS/OS) interface. Furthermore, fundus autofluorescence shows hypo-autofluorescence corresponding to a IS/OS junction defect8. This is encircled by a hyperautofluorescent ring, which differs from pseudovitelliform dystrophy, that manifests similarly on fundus examination.
Unilateral acute idiopathic maculopathy is an inflammatory disease of the outer retina and RPE of the macula9. Fundus examination shows grayish lesions at the level of the RPE affecting the fovea10. The OCT examination typically reveals disruption of the photoreceptor IS/OS layer and deposition of hyper-reflective subretinal debris material9.
ARPE and FA were first described through transmission hyper-fluorescence, which did not show leakage in the macular hypopigmented areas2. This finding was corroborated by other case reports3. SD-OCT imaging typically reveals abnormally increased reflectivity on the outer nuclear layer and RPE layers, hyper-reflective accumulations (humps) involving the inner band and photoreceptor outer segments, without sub-RPE, subretinal, or intraretinal fluid accumulation3. These findings support the idea that the primary area of inflammation is in the outer retinal layers, especially in the interdigitation zone, ellipsoid zone, and external limiting membrane, rather than the RPE5. The main finding in our case was the hump that stretched from the RPE to the external limiting membrane, with disruption of the ellipsoid zone and interdigitation zone.
This is the first reported case of secondary CNV after ARPE. Considering the inflammatory pathophysiology, this outcome is possible.
ARPE is a benign self-limiting disease that affects the macula. It frequently resolves with full restoration of visual acuity, without permanent visual impairment. Nevertheless, following the occurrence of CNV, it can lead to severe visual loss and a reduction in the functional status and quality of life of patients. The present case indicates that CNV is a possible and serious outcome after ARPE. Multimodal imaging, early detection, and accurate diagnosis are essential for the appropriate treatment of patients and the prevention of unfavorable visual outcomes.
REFERENCES
1. Gundogan FC, Diner O, Tas A, Ilhan A, Yolcu U. Macular function and morphology in acute retinal pigment epithelitis. Indian J Ophthalmol. 2014;62(12):1156-8
2. Baillif S, Wolff B, Paoli V, Gastaud P, MaugetFaÿsse M. Retinal fluorescein and indocyanine green angiography and spectraldomain optical coherence tomography findings in acute retinal pigment epitheliitis. Retina. 2011;31(6):1156-63.
3. Hsu J, Fineman MS, Kaiser RS. Optical coherence tomography findings in acute retinal pigment epitheliitis. Am J Ophthalmol. 2007;143(1):163-5.
4. Puche N, Offret O, Bernard JA, BeharCohen F. A case of acute retinal pigment epithelitis: Spectral domain optical coherence tomography time course and physiopathologic hypothesis. Clin Ophthalmol. 2010 Sep 20;4:1029-33.
5. Kılıç R. Acute retinal pigment epitheliitis: a case presentation and literature review. Arq Bras Oftalmol. 2021;84(2):186-90.
6. Toledo JJ, García JR, Asencio M, Schlincker A, López A. Recurrent acute retinal pigment epitheliitis: spectral domain optical coherence tomography and optical coherence tomography angiography features. Retin Cases Brief Rep. 2021;15(2):174-5.
7. Moraes RT, Vianna RN, Souza EC, Moraes LS. Clinical Variants of Presumed Acute Fovealitis. Retinal Cases Brief Rep. 2022; 16(6):754-8.
8. Bruè C, Mariotti C, De Franco E, Fisher Y, Guidotti JM, Giovannini A. Solar retinopathy: a multimodal analysis. Case Rep Ophthalmol Med. 2013;2013:906920.
9. Dompieri RC, Manzano RPA, Frazão MAM, Kurimori HY, Chao JCT, Lui ACF. Unilateral acute idiopathic maculopathy secondary to yellow fever disease: a case report. Am J Ophthalmol Case Rep. 2019 May 9;15:100464.
10. de la Fuente MA, Cuadrado R. Unilateral acute idiopathic maculopathy: angiography, optical coherence tomography and microperimetry findings. J Ophthalmic Inflamm Infect. 2011;1(3):125-127.
AUTHORS INFORMATIONS





Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
February 2, 2023.
Accepted on:
March 15, 2023.