Marcela de Cassia Barreira1,2
DOI: 10.17545/eOftalmo/2023.0036
Este artigo pertence à Edição Especial Neuroftalmologia por imagem: acima e além
This study describes a 32-year-old female patient with horizontal binocular diplopia that worsened within a month. Upon admission, her left eye was not moving sufficiently to the left, and both of her eyes were crossed.
She denied any history of previous strabismus, patch use, high hypermetropia during her infancy, and any history of trauma, viral infections, or vaccine shots related to diplopia onset.
She also denied any history of chronic diseases or medication use.
During ophthalmologic examination, she had a visual acuity score of 20/20 in both eyes without correction.
Ocular motility:
During the cover test, esotropia at 25 prism diopters (PD) in primary position was identified.
She exhibited esotropia >50 PD in the left position and no deviation in the right position. When both eyes were open, she turned her head to compensate the diplopia, and when evaluating the versions, we noted an abduction limitation in the left position.
Furthermore, forced duction test showed no signs of restriction in the left medial rectus, whereas a force generation test showed a diminished force in the lateral rectus (Figure 1).
Meanwhile, fundus biomicroscopy was unremarkable.
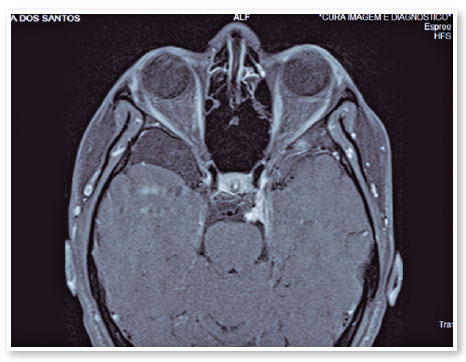
Considering that this young patient had a suspected sixth cranial nerve palsy without risk factors for microvascular paralysis and other related medical histories, an orbit and brain magnetic resonance imaging (MRI) was conducted to evaluate the VI cranial nerve path.
The magnetic resonance imaging (MRI) revealed a compressive lesion at the left cavernous sinus with meningioma characteristics, which justified our findings (Figure 2).
Every time we encounter a patient with an incomitant strabismus with suspected nerve paralysis, we have to follow certain steps for a more precise diagnosis. The first step is acquiring a complete anamnesis to determine when the symptoms started and how fast they progressed, and to determine the risk factors and patient’s history of medications, other systemic symptoms, or diseases that could possibly lead to the correct diagnosis. Thereafter, we conduct a complete ocular examination, which includes inspection, visual acuity, pupil reaction, ocular motility, and version and duction tests. Forced duction, force generation, and saccadic velocity tests, can be performed to exclude signs of restriction. Finally, fundus biomicroscopies are conducted.
In patients aged over 50 years with uncontrolled diabetes or hypertension showing an isolated oculo
motor paralysis, we first suspect microvascular paralysis1. Hence, we should closely monitor such patients and avoid performing any imaging right away. In all other cases and in patients with other symptoms associated with paralysis, computed tomography, MRI, or computed tomography angiography is mandatory, depending on medical judgment2.
REFERENCES
1. Elder C, Hainline C, Galetta SL, Balcer LJ, Rucker JC. Isolated Abducens Nerve Palsy: Update on Evaluation and Diagnosis. Curr Neurol Neurosci Rep. 2016;16(8):69.
2. Chi SL, Bhatti MT. The diagnostic dilemma of neuro-imaging in acute isolated sixth nerve palsy. Curr Opin Ophthalmol. 2009;20(6):423-9.
AUTHOR INFORMATION
Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
June 7, 2023.
Accepted on:
June 12, 2023.