Isabella Cristina Borges Pio1; Christine Lanssoni Zucatti1,2; André Araújo Pinheiro1,2; Breno Hermann Ferreira Gondim1
DOI: 10.17545/eOftalmo/2023.0013
ABSTRACT
Ocular ischemic syndrome is caused by chronic ocular hypoperfusion due to the obstruction of the internal or common carotid artery. The associated ocular symptoms mainly include low vision and pain. Ocular damages are usually irreversible, and the treatment is based on the associated complications. A 69-year-old man with hypertension complained of sudden visual impairment in the left eye since 1 day. Based on his eye examination, he had the visual acuity of counting fingers at 3 meters in the left eye; moreover, he had diffuse retinal pallor, a cherry red spot in the macula, diffuse vascular narrowing, and Hollenhorst plaque at the bifurcation of the inferior temporal arcade according to the results of funduscopy. Accordingly, he was diagnosed with central retinal artery occlusion in the left eye. After 25 days, he presented again with the complaint of pain in the left eye and precordialgia, and carotid doppler findings revealed 70%–80% and 50% stenosis of the right and left internal carotid arteries, respectively. On examination, he presented with changes indicative of ocular ischemic syndrome. Further, the patient was admitted for cardiac catheterization and ophthalmologic follow-up. Ocular ischemic syndrome is caused by severe stenosis of the internal or common carotid artery. Moreover, it is mainly caused by atherosclerosis and is associated with high mortality. Notably, ischemic eye syndrome is the first manifestation of internal carotid stenosis in ≤69% of the cases, which highlights the importance of early diagnosis by the ophthalmologist.
Keywords: Ocular Ischemic Syndrome; Central Retinal Artery Occlusion; Carotid Obstruction.
RESUMO
A síndrome ocular isquêmica (SOI) é uma condição de hipoperfusão ocular crônica causada por obstrução da carótida interna ou da carótida comum. Os sintomas oculares incluem principalmente a baixa de visão e dor. Geralmente as alterações oculares são irreversíveis e feito o tratamento de suas complicações. Masculino 69 anos, hipertenso apresentando baixa visual súbita em olho esquerdo há 1 dia. Ao exame apresentava acuidade visual no olho esquerdo conta dedos a 3m e palidez difusa de retina, mácula em cereja, estreitamento vascular difuso e placa de Hollenhorst na bifurcação da arcada temporal inferior na fundoscopia. Diagnosticado como oclusão de artéria central da retina em olho esquerdo. Após 25 dias, retornou com dor no olho esquerdo e precordialgia, trazendo angiotomografia de carótidas com estenose de 70-80% da carótida interna direita e 50% a esquerda. Ao exame apresentava alterações indicativas de síndrome ocular isquêmica. Paciente internado para cateterismo cardíaco e seguimento oftalmológico. A síndrome ocular isquêmica é decorrente da estenose grave da artéria carótida interna ou comum. É causada principalmente por aterosclerose e está associada a alta mortalidade. Vale ressaltar que a síndrome ocular isquêmica é primeira manifestação da estenose da carótida interna em até 69% dos casos, o que reforça a importância do diagnóstico precoce pelo oftalmologista.
Palavras-chave: Síndrome Ocular Isquêmica; Oclusão Artéria Central Retina; Obstrução Carotídea.
Ocular ischemic syndrome (OIS) is a condition of chronic ocular hypoperfusion caused by severe stenosis of the internal or common carotid artery. It is mainly caused by atherosclerosis and is unilateral in 80% of the cases1,2. Moreover, it is predominantly observed in men aged >50 years1,2 and is associated with high mortality, which is estimated to reach 40% in 5 years2,3.
The main symptom of OIS is vision impairment, which is usually gradual and may be associated with pain. In addition, other alterations can be found, such as irian and iridocorneal angle neovessels, anterior chamber reaction, decrease in or abolition of photomotor reflex, dilated episcleral vessels, retinal hemorrhages, microaneurysms, and cholesterol embolization occlusion causing retinal hypoperfusion1-5.
Despite the presence of angle neovessels, the patient may not present with increased intraocular pressure because of the decreased production of aqueous humor1,4,5.
The treatment of OIS is multidisciplinary, and the main objective of the treatment is cardiovascular and neurological treatment.
In OIS, the ocular damages are usually irreversible, and the ophthalmologic treatment is based on complications, such as neovascular glaucoma3-5.
Notably, OIS is the first manifestation of internal carotid stenosis in ≤69% of the cases1, highlighting the importance of early diagnosis by the ophthalmologist, which directly impacts the survival of the patient, as seen in the case presented below.
A 69-year-old man with hypertension and dyslipidemia presented to the ophthalmic emergency room (ER) with sudden vision loss in the left eye (OS) since 1 day.
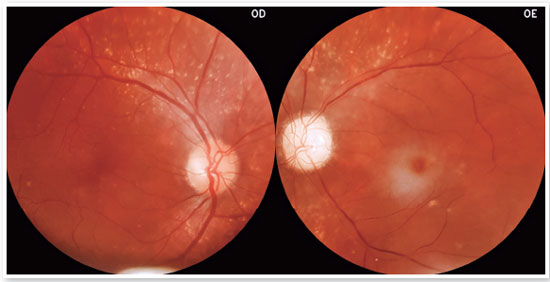
On examination, he presented with visual acuity (VA) of 20/20 in the right eye (OD) and counting fingers at 3 meters in the OS. Tonometry and optical coherence tomography biomicroscopy findings were normal. OS fundoscopy revealed diffuse retinal pallor, stained papillae, cherry macula, diffuse vascular narrowing, Hollenhorst plaque at the bifurcation of the inferior temporal arcade, and diffuse drusen (Figure 1).
At the first presentation, he was diagnosed with central retinal artery occlusion in the OS. Hypotensive measurements were performed and a cardiovascular evaluation was requested; however, the patient was lost to follow-up.
After 25 days, he returned to the ER with pain in the left eye and precordialgia for 3 days; further, OCT revealed macules with edema of the inner retinal layers in the left eye (Figure 2), and carotid doppler findings revealed 70%–80% and 50% stenosis of the right and left internal carotid arteries, respectively.
His examination also indicated VA of hand movement in the OS, and tonometry results revealed that intraocular pressures in the OD and OS were 10 and 20 mmHg, respectively. Further, OS biomicroscopy (Figure 3) revealed dilated episcleral and conjunctival vessels, the anterior chamber reaction of grade 1+, irian neovessels, and decreased photomotor reflex.
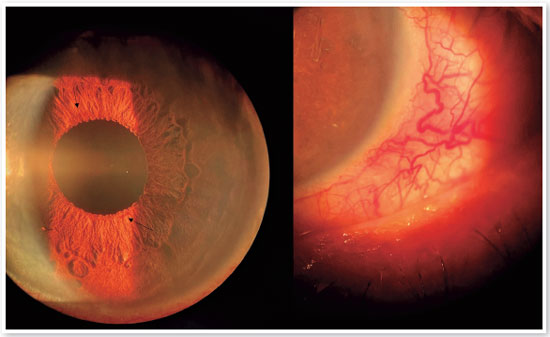
OS funduscopy also revealed intense papillary pallor and maintained retinal appearance compared with the first presentation.
Subsequently, the patient was diagnosed with OIS in the left eye and admitted for further cardiovascular evaluation.
During hospitalization, he underwent catheterization, indicating severe coronary artery disease, and angioplasty with stent placement.
An additional evaluation revealed neovascular glaucoma in the left eye with an intraocular pressure of 37 mmHg; further, panretinal photocoagulation treatment was initiated.
REFERENCES
1. Terelak-Borys B, Skonieczna K, Grabska-Liberek I. Ocular ischemic syndrome - a systematic review. Med Sci Monit. 2012; 18(8):RA138-RA144.
2. Moura FC, Takahashi VKT, Minelli E. Ischemic ocular syndrome simulating unilateral diabetic retinopathy: case report and literature review. Rev. Bras. Oftalmol. 2012;71(4):250-2.
3. Vazirani JA, Zadeng Z, Dogra MR; Gupta A. Ocular ischemic syndrome. Indian J Ophthalmol. 2014; 62(5):658-60.
4. Malhotra R, Gregory-Evans K. Management of ocular ischaemic syndrome. Br J Ophthalmol. 2000;84(12):1428-31.
5. Arcieri ES, Costa VP. Síndrome ocular isquêmica associada a glaucoma neovascular: relato de um caso. Arq. Bras. Oftalmol. 2001;64(3):255-7

Funding: No specific financial support was available for this study.
Conflict of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
December 6, 2022.
Accepted on:
January 21, 2023.