Júlia Spolti1; Eduarda Tanus Stefani1; Luana Carbonera Araldi1; Rafael Diego Signor1; João Paulo André Aragon Almanza1; Cesar Gomes da Silveira2
DOI: 10.17545/eOftalmo/2022.0022
ABSTRACT
The ophthalmological manifestations resulting from SARS-CoV-2 infection have been documented in the scientific community, but the knowledge about the related affections to the posterior ocular segment is still scarce. In this study, we report a young patient with visual complaint after a recent COVID-19 infection, showing important retinal hemorrhages and bevacizumab was the treatment of choice, leading to clinical improvement. We highlight the importance of fundoscopic monitoring in post-COVID-19 patients for non-invasive assessment of systemic circulatory patterns.
Keywords: COVID-19, Retinal hemorrhage; SARS-CoV-2 infection.
RESUMO
As manifestações oftalmológicas decorrentes da infecção pelo SARS-CoV-2 estão sendo estudadas no meio científico, entretanto, o conhecimento acerca das afecções relacionadas ao segmento ocular posterior ainda é escasso. Neste trabalho relatamos uma paciente jovem com queixa visual após infecção recente por COVID-19, evidenciando importantes hemorragias retinianas. O uso de bevacizumab foi o tratamento escolhido, levando à melhora do quadro. Destacamos, então, a importância do monitoramento fundoscópico em pacientes pós-COVID 19 para avaliação dos padrões circulatórios sistêmicos de forma não invasiva.
Palavras-chave: COVID-19; Hemorragia Retiniana; Infecção pelo SARS-CoV-2.
INTRODUCTION
In December 2019, the first cases of severe acute respiratory syndrome-coronavirus-2 (SARSCoV2) pneumonia were diagnosed in Wuhan, China. The main clinical manifestations show great variability in signs and symptoms, and some studies have reported ophthalmological findings(1,2). Ocular manifestations of coronavirus disease-2019 (COVID19) are uncommon, with an estimated prevalence of ≤4%(3). The most frequent changes are dry eyes, blurred vision, foreign-body sensation(4), conjunctivitis, epiphora, conjunctival hyperemia, and chemosis(2).
The presentations of this disease in the posterior segment of the eye point to nonspecific lesions, such as hyper-reflective bands at the level of the ganglion cells(5). There are also reports on retinal venous occlusions and macular edema(6). This report presents a case of presumptive retinal vein occlusion shortly after COVID19 infection(6,7).
CASE REPORT
In September 2020, a 32-year-old woman sought care owing to the presence of dark “spots” in the left eye (OS) for approximately 3 days. She had experienced a mildly symptomatic SARS-CoV-2 infection 1 month prior to the onset of visual symptoms. COVID-19 was diagnosed with molecular testing using the polymerase chain reaction technique. No lesions were seen on chest computed tomography, and blood test findings were normal, without signs of coagulopathy. The patient’s clinical history had no comorbidities, and she denied a history of trauma, smoking, or use of any drugs with risk of a thromboembolic event. There was no need for hospitalization because of COVID-19.
On examination, she presented a corrected visual acuity (VA) of 20/20 in the right eye (OD) and 20/100 in OS. Biomicroscopic examination was within normal limits, without anterior chamber reaction and with an intraocular pressure of 10 mmHg in both eyes (OU). On fundus examination, an increased and asymmetric excavation was observed in OD. In OS, preretinal and vitreous bleeding could be observed, which affected the upper and lower retinal arcade, proximal to the disk, with vitreitis. Optic disk edema was also present. An optical coherence tomography (OCT) of the macula and optic disk in OU (Figures 1 and 2) was performed on the same day, which showed a swollen optic disk, preretinal bleeding in the upper and lower arcades proximal to the disk, and punctual bleeding in the terminal arcades, with no macular edema.
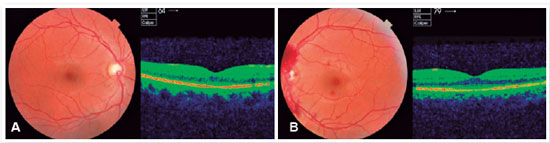
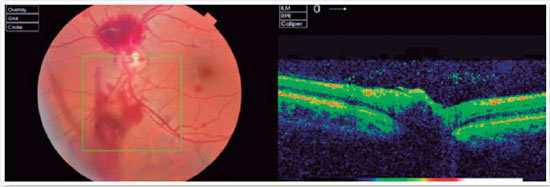
Under the diagnostic hypothesis of venous hemiocclusion, treatment with bevacizumab (Avastin®; Genentech, Inc., San Francisco, CA, USA) 1.5 mg was instituted, aiming to reduce vasculitis and pathological angiogenesis, because no protocol had been established for this kind of condition at the time. On a return consultation 1 week later, the patient reported improvement. OCT showed a significant decrease in the area of bleeding, with improvement in VA. The VA observed before the diagnosis of the retinal event was restored: 20/20 OD and 20/60 OS (Figures 3 and 4). It should be noted that the patient’s best VA in OS since 2018 had been 20/60 owing to amblyopia in OS.
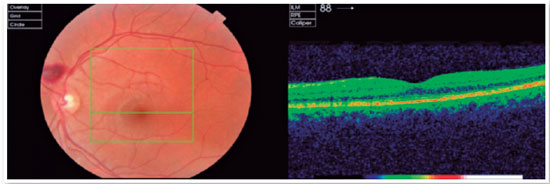
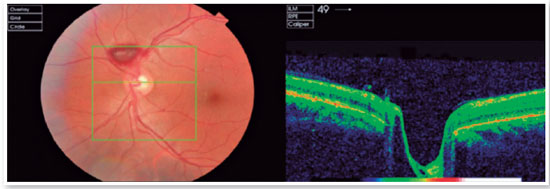
One month after diagnosis, there was an improvement in OS, with no more hemorrhage and 20/60 vision, with other ophthalmological examination standards unchanged and within the normal range. VA remained 20/20 in OD.
DISCUSSION
COVID19 is mainly characterized by symptoms of cough, fever, dyspnea, and pneumonia(1), but it may be related to other clinical outcomes not yet well elucidated in the literature, as in the case of the patient reported in this study. Little is known about ophthalmologic involvement, especially retinal lesions, although there are already reports on punctual hemorrhage and central retinal vein occlusion in COVID-19(8,9). In the present report, hemorrhage was observed proximal to the optic disk, in addition to optic disk edema.
According to the current literature, these alterations are characteristic of retinal venous occlusion. In most cases, this condition is found in people over 40 years of age, and more frequently in elderly people over 60 years of age(10). It is characterized by unilateral vision loss after engorgement and dilatation of retinal veins, followed by retinal hemorrhage and areas of ischemia(10). Hemorrhage extends from the optic nerve head to the periphery of the retina; candle flame-shaped hemorrhages, which are mostly superficial, and cotton-wool spots, which represent ischemia, can also be observed. Less frequently, macular and optic nerve edema are present(11).
Currently, it is suggested that COVID-19 infection may a predisposing factor for thrombotic events(12). Studies have already put forth the hypothesis that the involvement of the retinal microvasculature seen in patients with COVID19 may be a result of the disease and consequently lead to significant ophthalmological manifestations, with a potential risk of retinal vascular complications(8,9,13,14).
It is known that the involvement of the microvasculature can cause eye diseases owing to the fact that the retinal circulation is a terminal arterial system(14). However, mechanisms that explain vascular damage in COVID19 are still not well understood. Two main hypotheses are being studied: first, a state of pseudovasculitis as a result of viral infiltration into endothelial cells(15), and second, a condition of hypercoagulability characterized by disseminated intravascular coagulation(16,17).
These characteristics make the correlation between the COVID19 infection and the retinal manifestations found in the present case plausible, according to the literature(8,9,13,14).
Immunobiologicals are being used to treat the complications of COVID19, not acting directly on the cause (virus) or on the state of hypercoagulability but rather on the body’s response to infection, such as vasculitis, pathological angiogenesis, and increased cytokine levels(18,19).
The proposed treatment aimed to protect the subretinal space from damage caused by hemorrhage and consequent insidious or sudden edema. Therefore, anti-vascular endothelial growth factor medication was administered to treat vasculitis and pathological angiogenesis, thereby reducing leaks, edema, inflammatory complexes, hemorrhages, and neovascular phenomena(6,8,19).
There is evidence of retinal vascular involvement in cases of COVID19 infection, including postvaccine events, because thrombotic events are known to be involved in the pathophysiology of the disease(20). The ophthalmological findings in this case coincide with those reported in most current studies; however, the appearance of vitreous hemorrhage a short time after the infection stands out, thereby suggesting deposits of immune complexes causing occlusion of the retinal vessels(6,21,22).
REFERENCES
1. Guan W, Ni Z, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-1720.
2. Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of Ocular Findings of Patients with Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020; 138(5):575-578.
3. Lawrenson JG, Buckley RJ. COVID-19 and the eye. Ophthalmic Physiol Opt. 2020;40(4):383-388.
4. Chen L, Deng C, Chen X, Zhang X, Chen B, Yu H, et al. Ocular manifestations and clinical characteristics of 535 cases of COVID-19 in Wuhan, China: A cross-sectional study. Acta Ophthalmologica. 2020;98(8):e951-e959.
5. Ortiz-Egea JM, Ruiz-Medrano J, Ruiz-Moreno JM. Retinal imaging study diagnoses in COVID-19: a case report. J Med Case Rep. 2021;15(1):15.
6. Sheth JU, Narayanan R, Goyal J, Goyal V. Retinal vein occlusion in COVID-19: A novel entity. Indian J Ophthalmol. 2020;68(10): 2291-2293.
7. Landecho MF, Yuste JR, Gándara E, Sunsundegui P, Quiroga J, Alcaide AB, et al. COVID-19 retinal microangiopathy as an in vivo biomarker of systemic vascular disease? J Intern Med. 2021; 289(1):116-120.
8. Walinjkar JA, Makhija SC, Sharma HR, Morekar S, Natarajan S. Central retinal vein occlusion with COVID-19 infection as the presumptive etiology. Indian J Ophthalmol. 2020;68(11):2572-2574.
9. Yahalomi T, Pikkel J, Arnon R, Pessach Y. Central retinal vein occlusion in a young healthy COVID-19 patient: A case report. Am J Ophthalmol Case Rep. 2020 Dec;20:100992.
10. Jonas JB, Monés J, Glacet-Bernard A, Coscas G. Retinal vein occlusions. Dev Ophthalmol. 2017;58:139-167.
11. Schmidt-Erfurth U, Garcia-Arumi J, Gerendas BS, et al. Guidelines for the Management of Retinal Vein Occlusion by the European Society of Retina Specialists (EURETINA). Ophthalmologica. 2019;242(3):123-162.
12. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian CD, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakaks EP, Gibson CM,Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH, Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group onPulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75(23):2950-2973.
13. Abrishami M, Emamverdian Z, Shoeibi N, Omidtabrizi A, Daneshvar R, Rezvani TS, et al. Optical coherence tomography angiography analysis of the retina in patients recovered from COVID-19: a case-control study. Can J Ophthalmol. 2021;56(1):24-30.
14. Ho D, Low R, Tong L, Gupta V, Veeraraghavan A, Agrawal R. COVID-19 and the Ocular Surface: A Review of Transmission and Manifestations. Ocul Immunol Inflamm. 2020;28(5):726-734.
15. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418.
16. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost. 2020;18(4):844-847.
17. Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020 Jul;191:145-147.
18. Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, et al. Bevacizumab plus Irinotecan, Fluorouracil, and Leucovorin for Metastatic Colorectal Cancer. N Engl J Med. 2004;350(23):2335-42.
19. Michels S, Rosenfeld PJ, Puliafito CA, Marcus EN, Venkatraman AS. Systemic bevacizumab (Avastin) therapy for neovascular age-related macular degeneration: Twelve-week results of an uncontrolled open-label clinical study. Ophthalmology. 2005; 112(6):1035-47.
20. Avery RL, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA, Giust MJ. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113(3):363-372.
21. Haritoglou C, Kook D, Neubauer A, Wolf A, Priglinger S, Strauss R, et al. Intravitreal bevacizumab (Avastin) therapy for persistent diffuse diabetic macular edema. Retina. 2006;26(9):999-1005.
22. Duabetic Retinopathy Clinical Research Network, Scott IU, Edwards AR, Beck RW, Bressler NM, Chan CK, Elman MJ, Friedman SM, Greven CM, Maturi RK, Pieramici DJ, Shami M, Singerman LJ, Stockdale CR. A Phase II Randomized Clinical Trial of Intravitreal Bevacizumab for Diabetic Macular Edema. Ophthalmology. 2007;114(10):1860-7.
23. Schaal KB, Höh AE, Scheuerle A, Schütt F, Dithmar S. Bevacizumab zur Therapie des Makulaödems Infolge Venöser Retinaler Gefäßverschlüsse. Ophthalmologe. 2007;104(4):285-9.
24. Priglinger SG, Wolf AH, Kreutzer TC, Kook D, Hofer A, Strauss RW, et al. Intravitreal bevacizumab injections for treatment of central retinal vein occlusion: Six-month results of a prospective trial. Retina. 2007;27(8):1004-12.
25. Damico FM. Angiogênese e doenças da retina. Arq Bras Oftalmol. 2007;70(3):547-553.
26. Sahebnasagh A, Nabavi SM, Kashani HRK, Abdollahian S, Habtemariam S, Rezabakhsh A. Anti-VEGF agents: As appealing targets in the setting of COVID-19 treatment in critically ill patients. Int Immunopharmacol. 2021;101(Pt B):108257.
27. Silva LSCD, Finamor LPS, Andrade GC, Lima LH, Zett C, Muccioli C, et al. Vascular retinal findings after COVID-19 vaccination in 11 cases: a coincidence or consequence? Arq Bras Oftalmol. 2022; 85(2):158-165.
28. Giampietro BV, Dutra S, Oliveira RVC, Biancardi AL, Veloso V, Curi ALL. Ophthalmological Findings in Patients with SARS-CoV-2 Infection Examined at the National Institute of Infectious Diseases - INI/Fiocruz. Ocul Immunol Inflamm. 2021 Oct 14:1-4.
29. Shiroma HF, Lima LH, Shiroma YB, Kanadani TC, Nobrega MJ, Andrade G, et al. Retinal vascular occlusion in patients with the Covid-19 virus. Int J Retina Vitreous. 2022;8(1):45.
AUTHOR’S INFORMATION




Funding: No specific financial support was available for this study
Conflict of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 12, 2022.
Accepted on:
October 11, 2022.