Patrícia Gomes Silva1; Natália Carvalho1; Livia Cristina Rios1; Pablo Felipe Rodrigues2; Nelson Chamma Capelanes1,2; Bernardo Kaplan Moscovici1,2
DOI: 10.17545/eOftalmo/2021.0031
ABSTRACT
Two cases of patients with hyperopia with high kappa angles were described. We used different excimer laser platforms in each case to treat the refractive error. Also, we used different ablation profiles (wavefront-guided and optimized) and centration points (pupil center and halfway between corneal apex and pupil center).
Keywords: Cornea; Refractive surgery; Excimer laser; Corneal topography; Hyperopia.
RESUMO
Dois casos de pacientes com hipermetropia com ângulo kappa grande foram descritos. Diferentes plataformas de laser excimer foram usadas em cada caso para tratar o erro de refração. Além disso, diferentes perfis de ablação foram utilizados (guiados e otimizados pelo Wavefront) e pontos de centralização (centro da pupila e a metade da distância entre o ápice da córnea e o centro pupilar).
Palavras-chave: Córnea; Cirurgia refrativa; Laser excimer; Topografia da córnea; Hipermetropia.
INTRODUCTION
We are at a time when the demand for visual quality has risen to a high level of excellence. Patients seeking laser refractive correction expect this and want changes in their quality of life. Refractive surgeries for farsightedness are still challenging and widely discussed1-15.
Determining the treatment center is very important in refractive surgery. With recent advances, the kappa angle has become an important consideration for improving visual results. The kappa angle is defined as the angle between the visual axis and the pupillary axis11. The pupillary axis is the line that passes through the center of the pupil perpendicular to the cornea. The visual axis connects the fovea with the attachment point. It is clinically identified by nasal displacement of the corneal light reflex and the center of the pupil. Farsighted patients tend to have a large kappa angle, which can lead to alignment errors during photoablation in refractive laser surgery12,13. A larger kappa angle increases the risk of decentralization because of the increased distance between the pupillary center and the visual axis. Also, the pupillary center changes with pupil size under different lighting conditions. Off-center ablation can induce astigmatism and leave visual deficits such as distortion, diplopia, change in brightness, and reduced visual acuity in the patient14,15. It is recommended in these cases to center the ablation profiles on or near the visual axis to reduce high-order aberrations14.
The objective of these cases is to compare and discuss the different ways to centralize refractive surgery in hyperopia. The best technique to be used has not yet been defined, however, most excimer lasers focus on the pupillary center, which can lead to unsatisfactory final results, as we will see below1.
CASE REPORTS
Case 1
A 26 years old male patient, referred to the cornea service to evaluate refractive surgery for hyperopia. The patient’s data examination is shown in Table 1A. The patient presented ocular motility and Titmus test within normal limits. Since the preoperative exam was considered normal (Figures 1 and 2), wavefront-guided Femto-LASIK procedure (pupil-centered) was the treatment option. The Scheimpflug tomography showed a kappa angle of 0.34 mm in OD and 0.40 mm in OS in this case. The excimer laser used was VISX 4 (Johnson & Johnson, New Brunswick, New Jersey, USA)) with the IFS 150 femtosecond laser (Johnson & Johnson, New Brunswick, New Jersey, USA) and the iDesign aberrometer (Johnson & Johnson, New Brunswick, New Jersey, USA). This aberrometer uses Hartmann-Shack technology and centers the treatment on the pupil center, with an iris registration eye tracker device. The patient presented normal high order aberrations (HOA) values pre-operatively (Figure 2). One month after the procedure, the patient had uncorrected visual acuity (UCVA) of 20 / 40p in both eyes and corrected visual acuity (CDVA) of 20 / 20p in both eyes, but complaining of nighttime difficulty. Upon returning, the patient maintained the complaint and presented static refraction of +1.00 S -1,00 C 90º in OD with 20/20 visual acuity and +1.00 S -1.00 C 170º in OS with VA of 20/40. The topography was slightly off-center (Figure 3), with an increase in HOA (Figure 4). The vision complaints could be explained by both HOA and residual refractive error.
In the follow-up, retreatment guided by total aberrometry was performed, 3 months after the first surgery, the ablation profile suggested by Idesign (Figure 5) was in accordance with the changes we evidenced in topography.
We opted for re-lifting the flap and perform a new wavefront-guided treatment, centered in the pupil as well.
After 1 month the patient had flat refraction in both eyes and UCVA of 20/20 in both eyes. At this moment, the patient has no complaints, with a decrease in HOA (Figure 6), especially in coma. The corneal profile improved after surgery (Figure 7), the keratometric values stabilized (as seen in Table 2A) 3 months after surgery.
Case 2
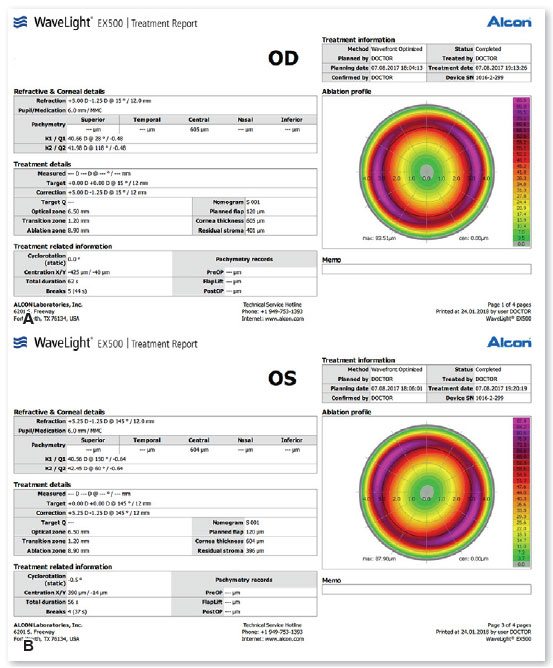
A 30 years old male patient, referred to the cornea service to evaluate refractive surgery for hyperopia. The patient’s data examination is shown in Table 1B. The patient presented ocular motility and Titmus test within normal limits. Since the preoperative exam was considered normal (Figures 8 and 9), optimized Femto-LASIK (centered on corneal apex) was performed using the FS200 laser (Alcon, Fort Worth, TX, USA). The excimer laser was the EX500 Wavelight laser (Alcon, Fort Worth, TX, USA). The kappa angle was 0.96 mm (Figure 9) measured by the Allegro Topolyzer Vario device (Alcon, Fort Worth, TX, USA), so it was decided to center halfway between the corneal apex and the pupillary center. The ablation profile and treatment planning can be seen in Figure 10. After the procedure, the patient had UCVA of 20/20 in both eyes with static refraction in OD: plane -0.25 C 050 and OE: plane -1.25 C 180, with no nocturnal complaints and normal corneal topography (Figure 11).
DISCUSSION
There is a discussion whether you should center your refractive surgery in the Purkinje reflex or the pupil center, but most of the literature recommends that centralization be performed first on the Purkinje reflex or at the apex of the cornea, using the value of the kappa angle measured by the tomography or topography. It can also be centered on the distance between the center of the pupil and the corneal reflex, especially in patients with a large kappa angle. The reports above demonstrate an important variation in centralization1.
Literature results about centralization
Nepomuceno et al carried out a study with hypermetropic patients. He performed LASIK, focusing on the coaxial reflex, in 61 patients with spherical equivalent +2.73 ± 1.41 D, using the LadarVision laser (Alcon, Fort Worth, TX, USA), and found 81.5% with UCVA greater than or equal to logMAR 0.2, and 44.4% greater or equal to logMAR 0. And he found no loss of corrected lines of sight2. Chang et al compared hyperopia treatment using LadarVision (+ 2.17 ± 0.93) centering on Purkinje with good final results: (logMAR): 0.22 ± 0.173.
Chan et al. performed surgeries comparing centralization in Purkinje or Pupil, in hyperopia patients, with a mean of +1.875 D, using VISX (Johnson & Johnson, New Brunswick, New Jersey, USA) and found better results in patients centralized in Purkinje4.
Kermani et al also performed hyperopia treatment with + 2.57 ± 1.56 D, using NIDEK (NIDEK, Maehama, Japan) comparing centralization in Purkinje and pupil and found better results when centralized in Purkinje5.
De Ortueta et al. in hyperopia patients (+ 2.76 ± 0.90 D) centered on Purkinje and found a postoperative refractive result of + 0.09 ± 0.32 D, with 94% with less than 0.50 D, using Esiris laser (Schwind, Klenoistheim, Germany)6.
Soler et al. in hypermetropic patients (+ 2.69 ± 0.91 D) compared centralization in Purkinje and pupil using Allegretto 200 Hz (Alcon, Fort Worth, TX, USA) and found similar refractive results7.
Reinstein et al. in hypermetropic patients found similar results in hypermetropic patients (+ 3.85 ± 0.98 D), using MEL 80 (Zeiss, Oberkochen, Germany)8.
Centralization issues
Most treatments guided by the total ocular aberrometry (TOA) center in the pupillary center, in this first case we imagine that the final result would be satisfactory, however, we needed a new treatment to correct the high order induced aberrations. The surgery was carried out guided by TOA and with a precise eye tracker mechanism, we were left with the hypothesis of wrong centering of the device or consequence of the Excimer laser centralization in the pupil, which may have caused coma and worsening the patient’s visual quality. In retreatment, the aberrometer accurately captured the induced coma, so treatment with excimer laser should correct the induced aberration Therefore, we opted for a new treatment guided by TOA, since the device correctly captured this decentralization and proposed an appropriate treatment. It is difficult to say that this would occur in all cases of high hyperopia with an increased kappa angle, and larger studies should be carried out to verify whether it was an isolated case9,10.
In the second case, with an unusual extremely high kappa angle, we were afraid to center directly on the corneal apex, so we thought to center in half of the distance between the pupil center and corneal apex, as described by some authors9,10.
We show 2 cases with increased kappa angle, the second case with an unusual pattern. Even so, it is difficult, with only 2 cases to compare them, not only because of the kappa angle differences, but also different platforms, centering on different points, and different ablation profiles: one case optimized and the other wavefront-guided. In the first case, since the kappa angle was moderated, we thought that centering the treatment in the pupil center and performing a waveguided treatment should not be a problem, but we had an unusual result that required retreatment. We cannot state that pupil-centered treatments should not be performed in patients with a kappa angle similar to that of patient one, since retreatment had good results. What we suggest is to check if the ablation profile is similar to what you want, in cases of personalized treatments.
Patients with moderate to high hyperopia are more likely to have an increased kappa angle. Most authors prefer to center these cases at the corneal apex or some point between the apex and pupillary center. Some authors believe that centering in the pupillary center, in cases with a kappa angle, can lead to an increase in HOA, especially coma1,2,7-10.
These two cases only brought the need for large and more detailed studies in hyperopic patients with moderate to large kappa angles to determine which centralization method should be the gold standard.
REFERENCES
1. Rios LC, Silva PGD, Canamary Junior AM, Rodrigues P, Regatieri CVS, Campos M, et al. Centration in refractive surgery. Arq Bras Oftalmol. 2020;83(1):76-81.
2. Nepomuceno RL, Boxer-Wachler BS, Kim JM, Scruggs R, Sato M. Laser in situ keratomileusis for hyperopia with the LADARVision 4000 with centration on the coaxially sighted corneal light reflex. J Cataract Refract Surg. 2004;30(6):1281-6.
3. Chang JSM, Law AKP, Ng JCM, Chan VKC. Comparison of refractive and visual outcomes with centration points 80% and 100% from pupil center toward the coaxially sighted corneal light reflex. J Cataract Ref Surg. 2016;42(3):412-9.
4. Chan CCK, Boxer-Wachler BS. Centration analysis of ablation over the coaxial corneal light reflex for hyperopic LASIK. J Refract Surg. 2006;22(5):467-71.
5. Kermani O, Oberheide U, Schmiedt K, Gerten G, Bains HS. Outcomes of hyperopic LASIK with the NIDEX NAVEX platform centered on the visual axis or line of sight. J Refract Surg. 2009;25(1 Suppl):S98-S103.
6. Ortueta D, Schreyger FD. Centration on the cornea vertex normal during hyperopic refractive photoablation using videokeratoscopy. J Refract Surg. 2007;23(2):198-200.
7. Soler V, Benito A, Soler P, Triozon C, Arné JL, Madariaga V, et al. A randomized comparison of pupil-centered versus vertex-centered ablation in LASIK correction of hyperopia. Am J Ophthalmol. 2011;152(4):591-9.e2.
8. Reinstein DZ, Gobbe M, Archer TJ. Coaxially sighted corneal light reflex versus entrance pupil center centration of moderate to high hyperopic corneal ablations in eyes with small and large angle kappa. J Refract Surg. 2013;29(8):518-25.
9. Mosquera SA, Ewring T. New asymmetric centration strategy combining pupil and corneal vertex information for ablation procedures in refractive surgery theoretical background. J Refract Surg. 2012;28(8):567-73.
10. Arba-Mosquera SA, Ortueta D. LASIK for hyperopia using an aberration-neutral profile with an asymmetric offset centration. J Refract Surg. 2016;32(2):78-83.
11. Hashemi H, Khabazkhoob M, Yazdani K, Mehravaran S, Jafarzadejpur E, Fotouhi A. Distribution of angle kappa measurements with Orbscan II in a population-based survey. J Refract Surg. 2010;26(12):966-71.
12. Basmak H, Sahin A, Yildirim N, Papakostas TD, Kanellopoulos JA. Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg. 2007;23(5):456-60.
13. Kermani O, Schmeidt K, Oberheide U, Gerten Gl. Hyperopic laser in situ keratomileusis with 5.5-, 6.5-, and 7.0-mm optical zones. J Refract Surg. 2005;21(1):52-8.
14. Reinstein DZ, Archer TJ, Gobbe M. Is Topography-guided ablation profile centered on the corneal vertex better than wavefront-guided ablation profile centered on the entrance pupil? J Refract Surg. 2012;28(2):139-43.
15. Yang Y, Thompson K, Burns SA. Pupil location under mesopic, photopic, and pharmacologically dilated conditions. Invest Ophthalmol Vis Sci. 2002;43(7):2508–12.
AUTHOR’S INFORMATION



Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
November 13, 2020.
Accepted on:
August 25, 2021.