Lais Bomediano de Souza1; Larissa Ferreira Vay1; Osias Francisco de Souza2
DOI: 10.17545/eOftalmo/2021.0027
ABSTRACT
Rhegmatogenous retinal detachment is the most common form of retinal detachments. The best approach to repair rhegmatogenous retinal detachment includes pars plana vitrectomy and one of its most important tools is the use of perfluorocarbon liquid. However, perfluorocarbon liquid is not totally safe. Inadvertent subretinal perfluorocarbon liquid retention should be avoided due to its potential side effect on the macular structure and function: perfluorocarbon liquid is directly toxic to ARPE-19 cells. We report a case of sub retinal perfluorocarbon liquid consequence of a surgical incident. During the injection of perfluorocarbon liquid, the initial jet stream caused a micro perforation of the retina and a volume of the material migrated to the sub retinal space. By the 30th post-operative day, fluorescein angiography and optical coherence tomography showed retinal atrophy in the same area. In conclusion, perfluorocarbon liquid must be used with caution: during the surgery infusion most be turned off and as softness of the globe is obtained, the injection should be done slowly, and the jet stream directed away from the macula. All residual perfluorocarbon liquid should be removed, and the entire vitreous cavity should be checked.
Keywords: Pars plana vitrectomy; Perfluorocarbon liquid; PFCL; Subretinal PFCL.
RESUMO
O descolamento regmatogênico da retina (DRR) é a forma mais comum de descolamento de retina. A melhor abordagem para corrigir o descolamento regmatogênico de retina inclui vitrectomia via pars plana e, uma de suas ferramentas mais importantes é o uso de perfluorocarbono líquido (PFCL). No entanto, o perfluorocarbono líquido não é totalmente seguro. A retenção inadvertida do perfluorocarbono líquido sub-retiniano deve ser evitada devido ao seu potencial efeito colateral na estrutura macular e na função porque o perfluorocarbono líquido age, de forma tóxica, diretamente nas células ARPE-19. Relatamos um caso de perfluorocarbono líquido sub-retiniano, consequência de um incidente cirúrgico. Durante a injeção de perfluorocarbono líquido, o jato inicial causou uma microperfuração na retina e o perfluorocarbono líquido migrou para o espaço sub-retiniano. No 30º dia do período pós-operatório, a angiografia com fluoresceína e a tomografia de coerência óptica mostraram atrofia retiniana na mesma área. Em conclusão, o perfluorocarbono líquido deve ser usado com cautela. Durante a cirurgia, a infusão deve ser desligada e à medida que a hipotonia do globo é obtida, a injeção deve ser feita lentamente e o jato direcionado para longe da mácula. Todo o perfluorocarbono líquido residual deve ser removido e toda a cavidade vítrea deve ser verificada.
Palavras-chave: Vitrectomia via pars plana; Perfluorocarbono líquido; Perfluorocarbono líquido sub-retiniano.
INTRODUCTION
Rhegmatogenous retinal detachments (RRD) are the most common form of retinal detachment (RD). Despite excellent skill and growing technology, up to 10% of cases require additional interventions to ultimately repair recurrent detachments caused mainly by proliferative vitreoretinopathy (PVR)1.
New technologies are introduced each year and one of the most important is the application of perfluorocarbon liquid (PFCL) in RRD, diabetic retinal traction detachment, severe PVR giant retinal detachment, posterior dislocated crystalline and intraocular lenses, and intraocular foreign bodies. The beginning was in 1987, after in vivo and in vitro studies of safety and efficiency in intraoperative applications, Chang et al. used PFCL during vitreous surgeries for retinal detachment patients with severe PVRs2.
PFCL helps retinal repair surgery because the density of PFCL in use is about two times greater than the perfusion solution´s, when injected into the vitreous cavity during vitrectomy, it generates a downward force against the interface. Upon detachment, the injected PFCL relocates and immobilizes the detached posterior retina. While PFCL is gradually injected into the vitreous cavity, the subretinal fluid is pushed anteriorly and thus into the vitreous cavity through the retinal breaks, which often allows avoiding posterior retinotomy for drainage. In some cases, this process can provide information about the location of unidentified peripheral breaks if subretinal fluid drainage is observed through breaks other than the first identified3.
However, PFCL is not completely innocuous. A prominent complication of intraoperative PFCL application is inadvertent subretinal PFCL retention. Subfoveal PFCL, even in small amounts, receives much attention due to its potential side effect
on the macular structure and function4. This is associated with poor visual outcomes because of its potential directly toxic effects on the retinal pigment epithelium (RPE) and photoreceptor cells5,6. Many studies agree that sub-retinal PFCL has to be removed6-8.
Liquid perfluorocarbon is directly toxic to ARPE-19 cells when exposure exceeds seven days. On the other hand, it seems that retinal ganglion cells (RGCs) suffer time-dependent damage rather by mechanical, other than toxic effects of PFCL9.
We present an unusual case of sub retinal PFCL, in which the perfluorocarbon surpasses to sub retinal space due to a surgical incident.
CASE REPORT
A 36-year-old man with decreased visual acuity (20/25 - Snellen Chart) and an inferior visual field defect in his left eye referred to our hospital. Fundoscopy and B-scan ultrasonography showed a macula-on superior RRD with a large superior retinal break, less than 90º in size. Pars plana vitrectomy (25 gauge) was performed with fluid-air exchange, endolaser photocoagulation around the retinal tear and gas tamponade (C3F8, 12%). The patient was instructed to maintain a supine position for 3 consecutive postoperative days and 27 more days avoiding dorsal horizontal decubitus.
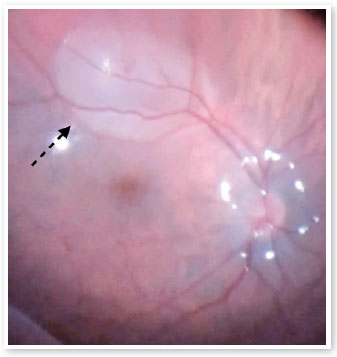
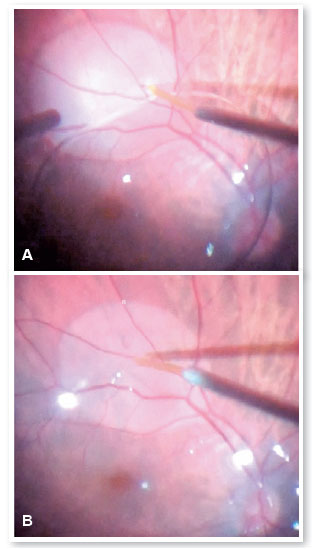
However, during the injection of PFCL to downwardly position the retina, the initial jet stream caused a retinal micro perforation and a volume of PFCL surpassed the retina and formed a bubble just below the inferior arcade (Figure 1). The decision was to remove the PFCL and using a 38-gauge cannula and active aspiration, the PFCL bubble was removed and the surgery was concluded, as described above (Figures 2 A,B).
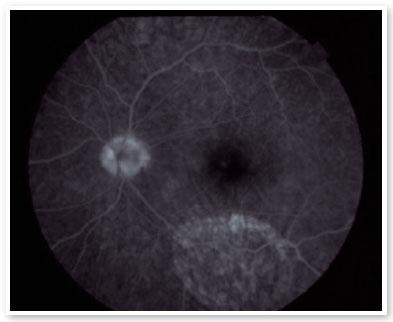
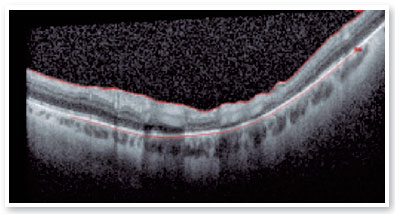
Within thirty days, a fluorescein angiography (FA) and an optical coherence tomography (OCT) showed an area of retinal and RPE atrophy corresponding to the area of incident subretinal PFCL bubble (Figures 3 and 4).
DISCUSSION
The present report is about a patient who had an extensive retinal tear with management similar to a giant retinal tear (GRT). GRT is a full-thickness neurosensorial retinal break that extends circumferentially around the retina for three or more clock hours, in the presence of a posteriorly detached vitreous. Its incidence in large population-based studies has been estimated as 1.5% of rhegmatogenous retinal detachments, with a significant male preponderance, bilaterality in 12.8% of cases. Most GRTs are idiopathic, but trauma, hereditary vitreoretinopathies and high myopia are each also causative, in decreasing frequencies. The vast majority of GRTs are currently managed with pars plana vitrectomy. Primary and final retinal reattachment rates are achieved in 88% and 95% of patients, respectively. Even when the retina remains attached, however, visual recovery may be limited10. The increasing efficiency in attaching the retina is due to numerous factors, including better technologies and the growth of surgical techniques. The use of PFCL has a fundamental role in cases of detachments caused by giant ruptures.
In cases of greater complexity, the use of PFCL always plays an important role, however, the possible related complications to the use of PFCL should be considered and avoided in all steps of the procedure. Perfluorocarbon under the retina could be toxic and cause permanent RPE damage.
Reports on the toxicity of PFCL present deleterious effects to the ARPE-19, a spontaneously arising human RPE cell line after seven days of exposure, and PFCL- generated damage through the mechanical force imparted to retinal ganglion cells9-11. In addition, PFCL-related ocular inflammation is also observed in clinical settings, especially in cases of subretinal retainment12. In the present report, PFCL was immediately removed during surgery, however maybe a minimally residual amount could explain the external retina and RPE damage observed on OCT and FA thirty days later.
In order to prevent and avoid such accidents, some precautions must be taken: the infusion must be turned off in anticipation and as the softness of the globe is obtained, the injection should be slowly done with a dual-bore cannula or one with similar mechanism, to prevent retinal trauma and avoid IOP elevations. The PFCL must be injected as a single bubble to prevent fish egg-like bubbles and dispersion to the posterior retina, a most common complication in small gauge needle techniques. Furthermore, the jet stream should be directed away from the macula and posterior pole, as well as the light pipe could be positioned in front of the jet to minimize its initial force. As a final precaution, by the end of the surgery, the entire vitreous cavity should be checked and all PFCL bubbles and microbubbles should be removed.
PFCL is to be used with caution during the injecting technique and must be carefully and completely removed by the end of the procedure to avoid serious damage to the retina and RPE.
REFERENCES
1. Adelman RA, Parnes AJ, Ducournau D; European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of uncomplicated retinal detachments: the European vitreo-retinal society retinal detachment study report 1. Ophthalmology. 2013;120(9):1804-8.
2. Chang S, Ozmert E, Zimmerman NJ. Intraoperative perfluorocarbon liquids in the management of proliferative vitreoretinopathy. Am J Ophthalmol. 1988;106(6):668-74.
3. Liu W, Gao M, Liang X. Management of Subfoveal Perfluorocarbon Liquid: A Review. Ophthalmologica. 2018;240(1):1-7.
4. Yu Q, Liu K, Su L, Xia X, Xu X. Perfluorocarbon liquid: its application in vitreoretinal surgery and related ocular inflammation. Biomed Res Int. 2014;2014:250323.
5. Berglin L, Ren J, Algvere PV. Retinal detachment and degeneration in response to subretinal perfluorodecalin in rabbit eyes. Graefes Arch Clin Exp Ophthalmol.1993;231(4):233-7.
6. Lee GA, Finnegan SJ, Bourke RD. Subretinal perfluorodecalin toxicity. Aust N Z J Ophthalmol. 1998;26(1):57-60.
7. Lai JC, Postel EA, McCuen BW 2nd. Recovery of visual function after removal of chronic subfoveal perfluorocarbon liquid. Retina. 2003;23(6):868-70.
8. Lesnoni G, Rossi T, Gelso A. Subfoveal liquid perfluorocarbon. Retina. 2004;24(1):172-6.
9. Inoue M, Iriyama A, Kadonosono K, Tamaki Y, Yanagi Y. Effects of perfluorocarbon liquids and silicone oil on human retinal pigment epithelial cells and retinal ganglion cells. Retina. 2009;29(5):677-81.
10. Shunmugam M, Ang GS, Lois N. Giant retinal tears. Surv Ophthalmol. 2014;59(2):192-216.
11. Osterholz J, Winter M, Winkler J, Pfister G, Kovacs G, Dresp J, et al. [Retinal damage by perfluorocarbon liquids - a question of specific gravity? Intraocular pressure peaks and shearing forces]. Klin Monbl Augenheilkd. 2009;226(1):38-47. German.
12. Lesnoni G, Rossi T, Gelso A. Subfoveal liquid perfluorocarbon. Retina. 2004;24(1):172-6.
AUTHOR’S INFORMATION
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
June 24, 2021.
Accepted on:
July 16, 2021.