Adriana Geremias Toni1,2; Nathalia Perussi Garcia1,2; Fernanda Gomes Goncalves Chaer1,2; Guilherme Novoa Colombo Barboza1,2; Marcello Novoa Colombo Barboza1,2; Marta Fabiane Gouvea Barioni1,2
DOI: 10.17545/eOftalmo/2021.0025
ABSTRACT
Spondyloarthropathies correspond to a group of systemic inflammatory diseases with chronic and progressive characteristics and may present several clinical manifestations. The objective of this study was to present five cases wherein ophthalmic findings were the first indicator of systemic disease. Ocular signs may be key for the diagnosis of a systemic rheumatological condition. Clinical follow-up and multidisciplinary evaluation are essential since the ophthalmologist is often the first specialist to be approached.
Keywords: Spondyloarthropathies; Uveitis; Anterior uveitis.
RESUMO
As espondiloartropatias correspondem a um grupo de doenças inflamatórias sistêmicas de característica crônica e progressiva, podendo apresentar diversas manifestações clínicas. O objetivo do presente estudo foi apresentar cinco casos de pacientes que tiveram achados oftalmológicos como primeiro indicador de doença sistêmica. O sinal ocular pode ser a chave para o diagnóstico de uma condição reumatológica sistêmica. É fundamental seguimento clínico e avalição multidisciplinar, uma vez que o oftalmologista é frequentemente o primeiro especialista a ser procurado.
Palavras-chave: Espondiloartropatias; Uveíte; Uveíte anterior.
INTRODUCTION
Spondyloarthritis corresponds to a group of inflammatory diseases that have similar clinical characteristics, immunogenetics, and radiological signs. This group includes ankylosing spondylitis, reactive arthritis, psoriatic arthritis, spondyloarthritis related to inflammatory bowel disease, and undifferentiated spondyloarthritis1.
According to a study by the Assessment of Spondyloarthritis International Society (ASAS), since 2009, the term “spondyloarthritis” has been used for spondyloarthropathies. This group of diseases can be divided into axial spondyloarthritis, which presents predominantly axial involvement represented by ankylosing spondylitis with or without sacroiliitis, and peripheral spondyloarthritis with a predominance of peripheral arthritis, enthesitis, and dactylitis. Peripheral spondyloarthritis includes psoriatic arthritis, reactive arthritis, and spondyloarthritis related to inflammatory bowel disease2,3.
Ankylosing spondylitis (AS) is a chronic and progressive inflammatory disease that affects the sacroiliac joints, spine, and peripheral joints. Less frequently, it may occur with extra-articular manifestations affecting the eye, skin, and cardiovascular system1–3. Ocular involvement is present in 20%-30% of patients with AS. The most common form of ocular manifestation of AS is anterior uveitis, which occurs in about 20%–30% of patients with AS2–5. It usually begins in the second or third decade of life, affecting mainly men1,6. Its pathogenesis remains unknown, but studies have shown a direct relationship with the human leukocyte antigen (HLA)-B27 being present in 80%–98% of spondylitis patients7,8. Antigen-related uveitis is characterized as a unilateral iridocyclitis of sudden and recurrent onsets with the presence of cells in the anterior chamber and frequently occurring with intense hyperemia, flare, posterior synechiae, possibly fibrin, hypopyon, and a pupillary inflammatory membrane1.
Reactive arthritis is represented by a classic triad of arthritis, urethritis, and conjunctivitis9,10. Conjunctivitis is the most prevalent ocular symptom (30%-60%) followed by nongranulomatous, synechial, bilateral, and asymmetric anterior uveitis, which mainly affects young males10,11. However, for definitive diagnosis, clinical and epidemiological findings should be correlated. In addition to ocular symptoms, patients may present joint pain, oral ulcers, chronic diarrhea, and urethritis12,13. As with AS, there is a direct relationship with the presence of the HLA-B27 antigen as seen in 60%-90% cases of reactive arthritis10,14.
This study aimed to present five cases of patients with spondyloarthritis having ophthalmic findings as a common factor that preceded the onset of joint manifestations.
CASE REPORTS
Case 1
The first case includes a 36-year-old male white patient who was a supervisor and an athlete by profession. He complained of pain, hyperemia, and low visual acuity in the right eye [oculus dexter (OD)] for the past 15 days. Regarding personal history, he reported low back pain for years and underwent lumbar surgery, associated with arthralgia in the shoulders, ankles, and knees. No previous ocular symptoms were reported.
Ophthalmological examination showed a corrected visual acuity (CVA) of 20/200 and 20/20; intraocular pressure (IOP) was 6 and 11 mmHg; and biomicroscopy showed opacity in the nasal cornea, fine keratic precipitates, cells in the anterior chamber (3+/4+), presence of fibrin, posterior synechiae, and lens opacity. The left eye [oculus sinister (OS)] showed no changes. Retinal mapping (RM) was impossible in OD due to the opacity of the medium; OE without changes. Topical prednisolone acetate (1%) and tropicamide (1%) were prescribed; tests and evaluation by a rheumatologist were requested.
The tests ruled out infectious causes, but the patient was positive for HLA-B27 and a 7-mm tuberculin [purified protein derivative (PPD)] test.
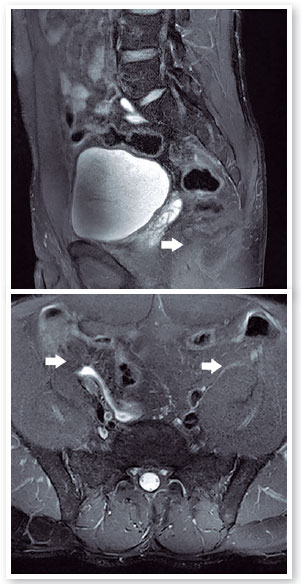
In the rheumatological evaluation, the patient presented low back pain with an inflammatory rhythm, and physical examinations showed a bilateral positive Fabere test, arthritis in the knees, and calcaneal enthesitis. Magnetic resonance imaging (MRI) of the sacroiliac joints showed bilateral sacroiliitis (Figure 1). With Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score of 4.5, a diagnostic hypothesis of nonradiographic axial spondyloarthritis was made. Sulfasalazine 2 g/day and a nonsteroidal anti-inflammatory drug (NSAID) were initially prescribed. The patient took this medication for 3 months without any clinical response. Prophylaxis for latent tuberculosis with isoniazid (300 mg/day) was initiated and maintained for 6 months. One month later, 5 mg/kg of infliximab, an immunobiological agent, was initiated (attack doses at 0, 2, and 6 weeks followed by every 8 weeks).
The patient returned after 3 months (while in use of infliximab) with no articular symptoms, CVA 20/20 in both eyes [oculus uterque (OU)], biomicroscopy showed no anterior chamber reaction in OU, and RM showed no changes in OU. No surgical procedures were carried out and only clinical treatment was continued for inflammation control; the patient progressed with a good therapeutic response (BASDAI score: 2).
Caso 2
The patient was a 33-year-old white female and an accountant by profession. She was referred to us by her rheumatologist, complaining of redness in OS for 3 days, and she reported being under rheumatological follow-up due to recurrent attacks of uveitis, with HLA-B27 positive for 3 years, but with no radiological signs or articular manifestations of the disease. She was taking 1 mg/kg/day prednisone, 2 g/day sulfasalazine, and 1 mg/mL topical dexamethasone.
The ophthalmological examination showed CVA of 20/20 and 20/40; IOP was 12 mmHg in OU; and biomicroscopy showed no changes in OD, whereas in OS, there were traces of cells in the anterior chamber, slight lens opacity, and iris pigments on the anterior lens capsule. RM showed no changes in OU. Subsequently, spondyloarthritis was hypothesized, and the patient was referred to the rheumatology department for systemic medication advice. The patient returned after 8 days with no signs of ocular inflammation.
Case 3
This included a 37-year-old white female patient who was a social worker by profession. She complained of redness and irritation in OS for the past 10 days. Regarding personal history, the patient reported two previous uveitis attacks and sequelae of poliomyelitis on the right side.
The ophthalmological examination presented a partial CVA of 20/20 in OU; IOP was 12 mmHg in OU; biomicroscopy of the OD showed no changes, whereas that of OS showed no keratic precipitates, but there were cells in the anterior chamber (1+/4+). RM showed no changes in OU. Topical prednisolone acetate (1%) in a regressive regimen and tropicamide (1%) were prescribed. Infectious causes were ruled out in the investigation. MRI of the sacroiliac joints showed slight subchondral bone edema on the iliac face of the left sacroiliac joint (Figure 2). The patient was positive for HLA-B27 and a 9-mm tuberculin PPD test.
Based on these clinical and laboratory findings, a diagnosis of spondyloarthritis was made, and the rheumatologist prescribed sulfasalazine treatment (2 g/day). The patient returned after 3 months with CVA of 20/20 AO; biomicroscopy showed no changes in OD, and no keratic precipitates or hyperemia was seen in OS.
Case 4
The patient was a 41-year-old white male who was a salesman by profession. He reported eye redness for the past 7 days. Regarding personal history, the patient reported systemic arterial hypertension, attacks of eye hyperemia and photophobia for 6 years, and the self-medication of oral prednisone (20 mg/day) during the attacks. Regarding family history, the patient reported that his mother had rheumatoid arthritis.
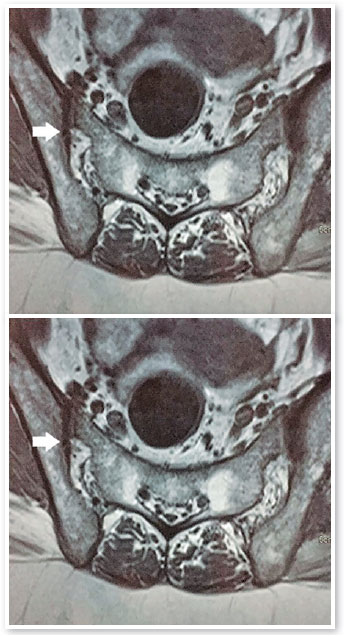
The ophthalmological examination showed CVA of 20/20 in OU; IOP was 16 and 12 mmHg; and biomicroscopy showed pigments in the anterior capsule of OD and cells in the anterior chamber (2+/4+) and iris pigments in the anterior capsule of OS. RM showed no changes in OU. Topical prednisolone acetate (1%) was prescribed, and rheumatological evaluation and laboratory tests were requested. Infectious causes were ruled out. The laboratory tests were positive for HLA-B27 and a 14-mm PPD test, whereas MRI showed ankylosis of the lower sacroiliac joint. A diagnosis of AS was made, and sulfasalazine (2g/day) was initiated under follow-up by a rheumatologist. The patient showed no subsequent ocular and systemic inflammatory signs.
Case 5
This included a 44-year-old white female patient who worked as an administrative civil servant. She complained of hyperemia, lacrimation, and photophobia in OD for the previous 10 days. Regarding personal history, the patient reported joint pain in her knees and elbows after physical exercise, low back pain, oral ulcers, and colitis diagnosed by a normal colonoscopy examination. Regarding family history, she reported that her father had rheumatoid arthritis.
The ophthalmological examination showed CVA of 20/40 and 20/20; IOP was 6 and 8 mmHg; and biomicroscopy showed conjunctival hyperemia (3+/4+), fine keratic precipitates, cells in the anterior chamber (2+/4+), and ruptured posterior synechiae in OD, and no changes were seen in OS. RM showed OD with a slight cotton-wool exudate in the superior temporal arcade with normal vitreous humor and OS without changes. Topical atropine (1%) and prednisolone acetate (1%) were prescribed, and laboratory tests and rheumatological evaluation were requested.
The patient returned after 20 days with her eye condition improved. The ophthalmological examination revealed CVA of 20/20 in OU and biomicroscopy showed OD without conjunctival hyperemia, fine keratic precipitates, ruptured posterior synechiae, and no anterior chamber reaction and OS without alterations. RM showed OD with decreased cotton-wool exudate in the superior temporal arcade. The patient had a positive HLA-B27 test result and negative results for infection tests. A diagnostic hypothesis of reactive arthritis was made due to the clinical findings of conjunctivitis, anterior uveitis, joint pain in the knees and elbows, colitis, recurrent aphthae, and positive HLA-B27. Sulfasalazine (2 g/day) was prescribed under rheumatological follow-up and possible treatment with immunobiological agents, due to the recurrence of symptoms and progressive radiological signs. The patient chose not to maintain the prescribed drug treatment, undergoing ophthalmological follow-up only during crises.
DISCUSSION
This article presents five cases of spondyloarthritis wherein the patients’ clinical ophthalmic findings were an important basis for the diagnosis of systemic disease. In the first case of nonradiographically diagnosed axial spondyloarthritis, the finding of anterior uveitis associated with epidemiological data and complaints were fundamental for the proper management of the patient. The classification criteria for spondyloarthropathies (Modified New York Criteria 1984 and ASAS 2013) were determined for use in population studies. According to these criteria, the diagnosis should not be ruled out if the criteria are not fulfilled9,15. The treatment aims to resolve the inflammatory process with consequent relief of pain and maintenance of the patient’s articular function. Standard treatment consists of the use of NSAIDs and physiotherapy2,16,17, corticosteroids, DMARDs, or immunobiological agents16–18. Immunobiological treatment has good prospects owing to the positive results demonstrated, especially in cases of uveitis, in promoting the patient’s complete visual recovery2. If nonradiographic axial spondyloarthritis is approached early and globally, it has a good prognosis, as in the case presented, wherein ophthalmological and rheumatological evaluations were essential to start the treatment, avoiding an unnecessary surgical approach.
The second and third cases also addressed the hypothesis of spondyloarthritis, in which the presence of the ocular condition and past history of uveitis led us to perform laboratory investigations, which showed positive HLA-B27 results in both cases. The difference between the second and third cases was the evidence of articular manifestations. The patients underwent treatment with sulfasalazine and later returned with improved ocular condition and probable remission of the systemic condition. It is common for these patients to undergo alternate periods of crisis and remission, and their condition may not be diagnosed at first. In the fourth case, the patient had attacks of eye hyperemia and photophobia for 6 years. It was only after clinical and radiological investigations and consulting a rheumatologist that it was possible to obtain the diagnosis of AS. After treatment with sulfasalazine, the patient progressed with an improvement of his condition without eye inflammatory signs. It is important to note that most people who are positive for HLA-B27 are healthy. Positivity of HLA-B27 increases the risk of AS by 50–100 times, but only 2% of these people develop the disease.
In the fifth case of reactive arthritis, epidemiological data were also contrary to the literature, which shows that this condition is more prevalent in young males5,6,12. The patient in this case was a woman in the fourth decade of life. However, the presence of the HLA-B27 antigen associated with the classic triad of conjunctivitis, arthritis, and urethritis were determinant to support the diagnosis of reactive arthritis. Treatment in the acute stages of the disease consists of NSAIDs at conventional doses12,14. Corticosteroids may be used in cases of oligoarthritis or enthesopathy that persist after treatment with NSAIDs. In chronic cases, sulfasalazine and methotrexate may be used, and the indication of immunobiological agents is not yet well elucidated. The use of antibiotics should also be considered if infection is present. In the fifth case, systemic treatment was not initiated due to patient’s refusal and a period of remission of the ocular inflammatory process.
All the five reported cases presented ocular manifestations as the first signs for the investigation of a rheumatological condition (Table 1). These patients often experience joint pain during their lifetime, but do not associate it with any systemic condition, especially in the case of young adult patients. Most often, they relate the pain to physical exercises or orthopedic diseases and do not undergo the necessary radiological investigations, remaining for long periods in either crisis or remission. None of the cases presented had hypopyon, which is considered a risk factor in patients diagnosed with spondyloarthritis19.
In conclusion, anterior uveitis may be the initial manifestation of spondyloarthritis. It is more usually correlated to AS, but it may also be present in reactive arthritis. Based on the presented data, the diagnosis, follow-up, and use of a multidisciplinary approach for these patients are considered essential. Clinical and laboratory investigations are necessary since the appropriate approach toward the underlying pathology can accurately infer the patient’s prognosis, thereby avoiding unnecessary interventions and prevent ocular and articular sequelae.
Ocular signs may be key for the diagnosis of a systemic rheumatological condition. Clinical follow-up and multidisciplinary evaluation are therefore essential since the ophthalmologist is often the first specialist to be sought.
REFERENCES
1. Gouveia EB, Elmann D, Morales MSA. Ankylosing spondylitis and uveitis: overview. Rev Bras Reumatol. 2012;52(5):749-56.
2. Rudwaleit M, Landewé R, van der Heijde D, Listing J, Brandt J, Braun J, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis. 2009;68(6):770-6.
3. Rudwaleit M, van der Heijde D, Landewé R, Listing J, Akkoc N, Brandt J, et al. The development of Assessment of Spondylo Arthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777-83.
4. Rademacher J, Poddubnyy D, Pleyer U. Uveitis in spondyloarthritis. Ther Adv Musculoskelet Dis. 2020;12:1759720X20951733. Published 2020 Sep 12.
5. Bacchiega ABS, Balbi GGM, Ochtrop MLG, de Andrade FA, Levy RA, Baraliakos X. Ocular involvement in patients with spondyloarthritis. Rheumatology (Oxford). 2017;56(12):2060-7.
6. Sampaio-Barros PD. Epidemiology of spondyloarthritis in Brazil. Am J Med Sci. 2011;341(4):287-8.
7. Rosenbaum JT, Asquith M. The microbiome and HLA-B27-associated acute anterior uveitis. Nat Rev Rheumatol. 2018;14(12):704-13.
8. Kopplin LJ, Mount G, Suhler EB. Review for Disease of the Year: Epidemiology of HLA-B27 Associated Ocular Disorders. Ocul Immunol Inflamm. 2016;24(4):470-5.
9. Ward MM, Deodhar A, Gensler LS, Dubreuil M, Yu D, Khan MA, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019;71(10):1285-99.
10. Palanisamy S. Suresh. Bilateral disciform keratitis in Reiter’s Syndrome. Indian J Ophthalmol. 2016;64(9):685-7.
11. Banares A, Hernandez-Garcia C, Fernandez-Gutierrez B, Jover JA. Eye involvement in the spondyloarthropathies. Rheum Dis Clin North Am. 1998 Nov; 24(4):771-84.
12. Kiss S, Letko E, Qamruddin S, Baltatzis S, Foster S. Long term progression, prognosis, and treatment of patients with recurrent ocular manifestations of Reiter’s syndrome. Ophthalmology. 2003;110(9):1764-9.
13. Lee DA, Barker SM, Su WP, Allen GL, Liesegang TJ, Ustrup DM. The clinical diagnosis of Reiter’s syndrome. Ophthalmic and non-ophthalmic aspects. Ophthalmology. 1986;93(3):350-6.
14. Bouzid N, Jamilloux Y, Chapurlat R, Pradat P, De Parisot A, Kodjikian L, et al. Impact of systemic treatments on the course of HLA-B27-associated uveitis: A retrospective study of 101 patients. PLoS One. 2020;15(3):e0230560.
15. Ward MM, Deodhar A, Akl EA, Lui A, Ermann J, Gensler LS, et al. American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network 2015 Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2016;68(2):282-98.
16. Mitulescu TC, Trandafir M, Dimăncescu MG, Ciuluvicetă RC, Popescu V, Predeteanu D, al. Advances in the treatment of uveitis in patients with spondyloarthritis - is it the time for biologic therapy? Rom J Ophthalmol. 2018;62(2):114-22.
17. Foster CS, Kothari S, Anesi SD, Vitale AT, Chu D, Metzinger JL, Cerón O. The Ocular Immunology and Uveitis Foundation preferred practice patterns of uveitis management. Surv Ophthalmol. 2016;61(1):1-17.
18. Dick AD, Rosenbaum JT, Al-Dhibi HA, Belfort R Jr, Brézin AP, Chee SP, Davis JL, Ramanan AV, Sonoda KH, Carreño E, Nascimento H, Salah S, Salek S, Siak J, Steeples L; Fundamentals of Care for Uveitis International Consensus Group. Guidance on Noncorticosteroid Systemic Immunomodulatory Therapy in Noninfectious Uveitis: Fundamentals of Care for UveitiS (FOCUS) Initiative. Ophthalmology. 2018;125(5):757-73.
19. Zaidi AA, Ying GS, Daniel E, Gangaputra S, Rosenbaum JT, Suhler EB, Thorne JE, Foster CS, Jabs DA, Levy-Clarke GA, Nussenblatt RB, Kempen JH, Systemic Immunosuppressive Therapy for Eye Diseases Cohort Study. Hypopyon in patients with uveitis. Ophthalmology. 2010;117(2):366-72.
AUTHOR’S INFORMATION





Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
July 21, 2020.
Accepted on:
December 15, 2020.