Caroline dos Reis; Mariana Amaranto de Souza Damásio; Sarah Pereira de Freitas Cenachi; André Vasconcellos Diniz; Jacques Ramos Houly
DOI: 10.17545/eOftalmo/2021.0019
ABSTRACT
Malattia leventinese or Doyne macular dystrophy is a rare autosomal dominant disease caused by a mutation in EFEMP1. It is characterized by the presence of numerous drusen with radial distribution at the posterior pole. Herein we present the case of a 39-year-old patient who underwent ophthalmological consultation and complained of low visual acuity in the left eye since approximately 2 years before. The diagnostic hypothesis of malattia leventinese with choroid neovascularization in the left eye was suggested after clinical evaluation and complementary investigation.
Keywords: Doyne macular dystrophy; Malattia leventinese; Retinal drusen.
RESUMO
A malattia leventinese ou distrofia macular de Doyne é uma doença autossômica dominante rara, causada por uma mutação no gene EFEMP1, caracterizada pela presença de inúmeras drusas com distribuição radial no polo posterior. Trata-se de uma paciente de 39 anos de idade que apresentou, à consulta oftalmológica, queixa de baixa acuidade visual no olho esquerdo (OE) percebida há aproximadamente dois anos. Foi aventada a hipótese diagnóstica de malattia leventinese com neovascularização de coroide no olho esquerdo, após avaliação clínica e propedêutica complementar.
Palavras-chave: Distrofia macular de Doyne; Malattia Leventinese; Drusas retinianas.
INTRODUCTION
Malattia leventinese (ML) is a rare autosomal dominant retinal dystrophy that was first described in Switzerland in 19251. It is a macular disease characterized by the presence of amorphous deposits, known as drusen, between the retinal pigment epithelium (RPE) and Bruch’s membrane. Drusen can appear in a mosaic pattern, which is why the disease is also named honeycomb dystrophy or Doyne dystrophy2,3.
The great importance of this disease is related to the fact that the main clinical alteration, i.e., drusen, is also a striking characteristic of other retinal dystrophies and age-related macular degeneration (ARMD)4,5.
The formation of subretinal neovascular membrane (SRNVM) is an unusual but threatening complication of ML, as it can result in irreversible visual damage and legal blindness in young adults6,7. The treatment of complications associated with SRNVM should be carefully analyzed, as a conservative approach is invariably associated with a worse prognosis7,8.
CASE REPORT
A 39-year-old female patient underwent an ophthalmological consultation owing to the complaint of low visual acuity (LVA) in her left eye (OS).
She reported regular treatment for hypothyroidism, but denied any family history of blindness or LVA.
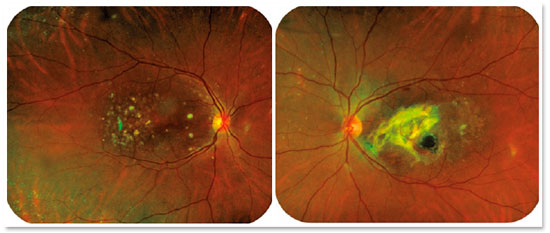
On ophthalmological examination, best corrected visual acuity of 20/25 in the right eye (OD) and finger counting at 20 cm in the OS were observed. Biomicroscopic examination of the anterior segment and Goldmann applanation tonometry revealed normal findings in both eyes (OU). Indirect binocular ophthalmoscopy of the OD revealed multiple yellowish-white lesions of varying sizes, consistent with macular drusen, particularly in the temporal direction from the fovea; in the OS, in addition to the presence of diffuse drusen, there was retinal thickening secondary to scar tissue formation, possibly due to SRNVM formation (Figure 1).
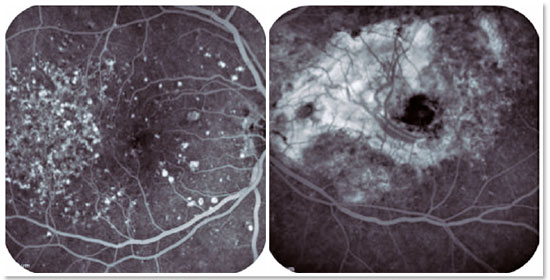
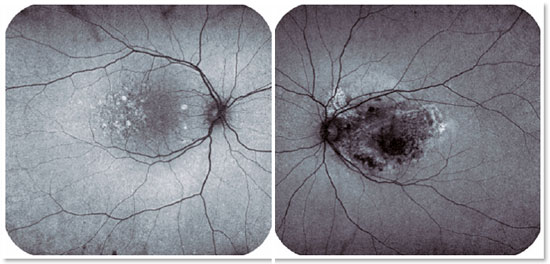
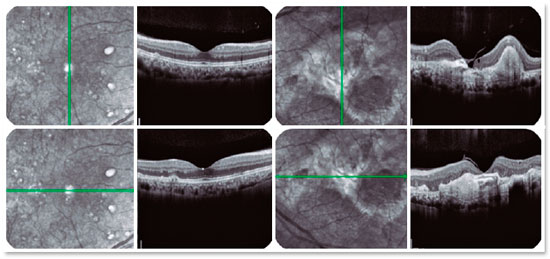
In view of the clinical findings, she underwent a complementary diagnostic investigation for better evaluation. Fluorescein angiography revealed several hyperfluorescent spots affecting the entire macular region of the OD due to contrast impregnation in the drusen, and an extensive area of hyperfluorescence with contrast tissue impregnation in the macular region of the OS, consistent with a disc-shaped scar secondary to SRNVM (Figure 2). Autofluorescence examination revealed hyperautofluorescent spots in the macular region of the OD and a hypoautofluorescent area indicating retinal atrophy in the macular region of the OS (Figure 3). Full-field electroretinogram was inconclusive, and electro-oculogram presented macular and cone functional impairment in OU. Optical coherence tomography (OCT) revealed focal, hyper-reflective, subepithelial lesions suggestive of drusen in the macular region of the OD. In the OS, OCT revealed an extensive hyper-reflective area associated with disorganization of the retinal layer microarchitecture, suggestive of fibrotic scar tissue (Figure 4). Further, OCT showed no changes in the optic disc.
In view of the clinical changes and complementary tests, the diagnostic hypothesis of ML was suggested. However, diagnostic confirmation via genetic testing has not yet been obtained.
DISCUSSION
ML is a rare, hereditary, degenerative macular disease characterized by the presence of drusen in a characteristic pattern, which may aid in the diagnostic suspicion of this disease9,10. ML has no pathognomonic characteristics, but its differentiation from other macular disorders is important because the exact diagnosis may have implications involving genetic counseling and therapeutic strategies.
Studies have identified EFEMP1 as the responsible gene4, which enables the diagnostic confirmation of ML via genetic testing. Despite the unavailability of genetic testing data in the presently reported case, the significant clinical changes evidenced in ophthalmoscopy and the emergence of multiple drusen at an early age and arranged in a peculiar pattern enabled the presumed diagnosis of ML.
The differential diagnosis of ML involves a heterogeneous group of retinal diseases in which macular drusen occur. These diseases are characterized by different modes of inheritance, age at onset, electrophysiological findings, and degree of visual disability5,6. One of these diseases is ARMD, a chronic and progressive retinal disease that may be associated with irreversible central vision impairment in the elderly population4. If ML results in extensive changes in the RPE, then geographic atrophy and SRNVM may be risk factors for legal blindness in the younger, economically active population6.
In the presently reported case, the patient already had a disc-shaped scar in the OS, possibly secondary to previous choroid neovascularization (with no signs of activity upon admission). Therefore, only conservative treatment was indicated.
REFERENCES
1. Vogt A. “Die Ophthalmoskopie im rotfreien licht.” Die Untersuchungsmethoden. Springer, Berlin, Heidelberg, 1925.
2. Marmorstein LY, Munier FL, Arsenijevic Y, Schorderet DF, McLaughlin P, Chung D, et al. Aberrant accumulation of EFEMP1 underlies drusen formation in Malattia Leventinese and age-related macular degeneration. Pro Natl Acad Sc U S A. 2002; 99(20):13067-72.
3. Doyne RW. Peculiar condition of choroiditis occurring in several members of the same family. Trans Ophthalmol Soc UK. 1899;19: 71.
4. Marmorstein LY. Association of EFEMP1 with malattia leventinese and age-related macular degeneration: a mini-review. Ophthalmic Genet. 2004;25(3):219-26.
5. Saksens NTM, Fleckenstein M, Schmitz-Valckenberg S, Holz FG, den Hollander AI, Keunen JEE, et al. Macular dystrophies mimicking age-related macular degeneration. Prog Retin Eye Res. 2014 Mar;39:23-57.
6. Marano F, Deutman AF, Leys A, Aandekerk AL. Hereditary retinal dystrophies and choroidal neovascularization. Graefes Arch Clin Exp Ophthalmol. 2000;238(9):760-4.
7. Sohn EH, Patel PJ, MacLaren RE, Adatia FA, Pal B, Webster AR, et al. Responsiveness of Choroidal Neovascular Membranes in Patients with R345W Mutation in Fibulin 3 (Doyne Honeycomb Retinal Dystrophy) to Anti-Vascular Endothelial Growth Factor Therapy. Arch Ophthalmol. 2011;129(12):1626-8.
8. Pager CK, Sarin LK, Federman JL, Eagle R, Hageman G, Rosenow J, et al. Malattia leventinese presenting with subretinal neovascular membrane and hemorrhage. Am J Ophthalmol. 2001;131(4):517-8.
9. Zweifel SA, Maygar I, Berger W, Rschuor P, Becker M, Michels S. Multimodal imaging of autosomal dominant drusen. Klin Monbl Augenheilkd. 2012;229(4):399-402.
10. Querques G, Guigui B, Leveziel N, Querquessss L, Bandello F, Souied EH. Multimodal morphological and functional characterization of Malattia Leventinese. Graefes Arch Clin Exp Ophthalmol.2013; 251(3):705-14.
AUTHOR’S INFORMATION



Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
May 7, 2020.
Accepted on:
December 15, 2020.