Carlos E. Veloso1; Sarah P. F. Cenachi1,2; Jacques R. Houly2; Arthur G. Reis3; Márcio B. Nehemy1
DOI: 10.17545/eOftalmo/2021.0008
ABSTRACT
To describe the potential complications of cryotherapy and the good response to intravitreal aflibercept in a patient diagnosed with peripheral exudative hemorrhagic corioretinopathy. An 83-year-old female with geographic atrophy in the posterior pole developed an exudative lesion in the temporal periphery of both eyes. Her best-corrected visual acuity was 20/80 in the right eye and 20/60 in the left eye. Fluorescein angiography, optical coherence tomography and B-scan ultrasonography were performed and the diagnosis of peripheral exudative hemorrhagic corioretinopathy was made. Reexamination 3 months later showed worsening of visual acuity in the right eye to count fingers due to sub-retinal fluid extension into the macula. She was initially submitted to cryotherapy. The patient showed sub-retinal hemorrhage in the first day after cryotherapy. She was then submitted to three monthly intravitreal injections of aflibercept with excellent results. Optical coherence tomography showed complete resolution of subretinal fluid and visual acuity returned to 20/80 in the right eye one month after the third intravitreal injection. No active exudative lesion was observed in the following three months. Cryotherapy may be a possible trigger for sub-retinal hemorrhage in cases of peripheral exudative hemorrhagic corioretinopathy and intravitreal injections of aflibercept showed to be an effective treatment.
Keywords: Cryotherapy; Age-related macular degeneration; Intravitreal injection; Peripheral exudative hemorrhagic corioretinopathy; Polypoidal choroidal vasculopathy.
RESUMO
O objetivo é descrever as complicações potenciais da crioterapia e a boa resposta ao aflibercepte intravítreo em uma paciente com diagnóstico de coriorretinopatia hemorrágica exsudativa periférica. Uma mulher de 83 anos com atrofia geográfica no polo posterior desenvolveu uma lesão exsudativa na periferia temporal de ambos os olhos. Sua melhor acuidade visual corrigida era de 20/80 no olho direito e 20/60 no esquerdo. Foram realizadas angiofluoresceinografia, tomografia de coerência óptica (OCT) e ultrassonografia modo B, e foi feito o diagnóstico de coriorretinopatia hemorrágica exsudativa periférica. Um novo exame 3 meses depois mostrou piora da acuidade visual para conta dedos no olho direito, devido à infiltração de líquido sub-retiniano na mácula. Inicialmente, a paciente submeteu-se à crioterapia, mas no dia seguinte ao tratamento, apresentou hemorragia sub-retiniana. Recebeu então três injeções intravítreas mensais de aflibercepte, com excelentes resultados. Uma nova OCT mostrou resolução completa do líquido sub-retiniano e a acuidade visual voltou a 20/80 no olho direito um mês após a terceira injeção intravítrea. Não se observou nenhuma lesão exsudativa em atividade nos três meses seguintes. A crioterapia pode ser um possível “gatilho” para hemorragia sub-retiniana em casos de coriorretinopatia hemorrágica exsudativa periférica e injeções intravítreas de aflibercepte mostraram ser um tratamento eficaz.
Palavras-chave: Crioterapia; Degeneração macular relacionada à idade; Injeções intravitreais; Corioretinopatia hemorrágica Periférica; Vasculopatia da coroide polipoidal.
CASE REPORT
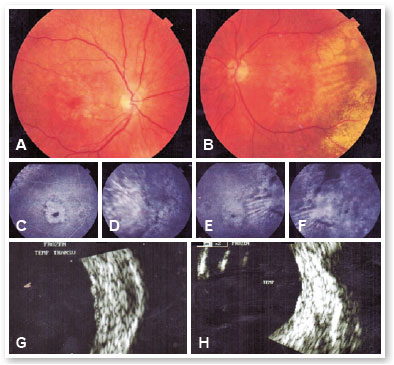
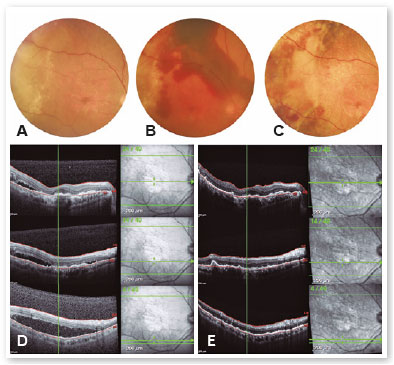
An 83-year-old female with systemic arterial hypertension and type 2 diabetes was referred with a history of loss of central visual acuity for the past 5 years. Her best-corrected visual acuity (BCVA) was 20/80 in the right eye (OD) and 20/60 in the left eye (OS). She was pseudophakic and her intraocular pressure was 10mmHg in both eyes. Ophthalmoscopy revealed geographic atrophy in the posterior pole and an exudative lesion in the temporal periphery of both eyes (Figure 1A,B). Fluorescein angiography (FA) showed hyperfluorescence due to a window defect in the perifoveal region and a late and irregular hyperfluorescence (leakage) in the temporal periphery of both eyes (Figure 1C-F). B-scan ultrasonography (US) showed a discrete and irregular retinochoroidal thickening in the temporal sector of both eyes with the following lesion dimensions in the right eye: 7.5 x 7.5 x 1.6mm (vertical x horizontal x height) (Figure 1G,H). The diagnosis of peripheral exudative hemorrhagic chorioretinopathy (PEHCR) was made and we decided just to observe this patient due to the lack of macular involvement. She came back 3 months later, complaining of worsening of visual acuity in the right eye. Her BCVA was count fingers in the OD and remained 20/60 in the OS. Ophthalmoscopy revealed increase of the temporal lesion in the right eye (Figure 2A). US confirmed the increase of lesion dimensions, 11,4 x 9,7 x 1,6mm (vertical x horizontal x height) and optical coherence tomography (OCT) showed sub-retinal fluid reaching the macula (Figure 2D). Treatment options and their potential benefits and complications were discussed with the patient that initially refused to be submitted to an intraocular procedure. She was then initially treated with cryotherapy, in which, after a peribulbar anesthesia, the surgeon gently pressed the probe on the conjunctiva while the retina was examined with an indirect ophthalmoscope; the pressure from the probe could be seen as an indentation in the affected retina. When the probe was in the correct position, the footswitch was pressed and the retina could be seen to whiten as it freezed. The footswitch was then released and the procedure was repeated on other sites of the peripheral lesion. However, an important sub-retinal hemorrhage and a mild vitreous hemorrhage were observed in the following day (Figure 2B). Due to this adverse result and the absence of improvement in the next three weeks, she accepted to be submitted to intravitreal injections of an anti-VEGF agent. She was then submitted to three monthly intravitreal injections of aflibercept with excellent functional and anatomical results. BCVA returned to 20/80 in the right eye one month after the third intravitreal injection. Ophthalmoscopy revealed hemorrhage absortion (Figure 2C) and OCT showed complete resolution of the subretinal fluid (Figure 2E). No new active exudative lesion was observed in the following three months.
DISCUSSION
PEHCR is an unusual disease of the retina. Reese and Jones first described it in 19621 and, historically, there were several terminologies for this disorder until 1982 when this condition was named as PEHCR2.
The pathophysiological process underlying PEHCR remains incompletely identified. Macular changes consistent with nonneovascular, atrophic, and neovascular manifestations of age-related macular degeneration were reported3,4. PEHCR has also been suggested to share a common etiology with polypoidal choroidal vasculopathy (PCV). Indocyanine green angiography has been used to demonstrate polypoidal lesions and choroidal neovascular networks similar those seen in PCV underlying PEHCR lesions5,6. Favorable anatomical and functional response to intravitreal therapy with anti-vascular endothelial growth factor (anti-VEGF) agents such as ranibizumab, bevacizumab and more recently aflibercept has been demonstrated7. Choroidal melanoma is an important differential diagnosis of PEHCR and the possibility of malignancy should be ruled out3,4.
In the majority of cases, PEHCR is a self-limiting condition, but it may be vision threating because of the subretinal hemorrhage and fluid extention into the macula. In such cases, treatment may be recommended. Treatment options reported in the literature include anti-VEGF therapy, laser photocoagulation cryotherapy, photodynamic therapy (PDT) and vitrectomy7-10.
This case report describes an elderly white female patient with decreased visual acuity, geographic atrophy secondary to AMD and subretinal exudation located in the temporal quadrant of both eyes. Subretinal fluid extension into the macula of the right eye was noted during her follow-up. The diagnosis of PEHCR was made due to the presence of epidemiological and clinical characteristics of this disease. The lack of indocyanine green angiography in the current case prevents identification of polypoidal lesions. The first treatment instituted was cryotherapy since the patient initially refused to be submitted to an intraocular procedure. However, subretinal and mild vitreous hemorrhage occurred in the early postoperative period. There was a temporal relationship between cryotherapy and the reported hemorrhage but a causal relationship remains presumed since PEHCR may also evolve this adverse effect. In the sequence, the patient was submitted to three monthly intravitreal injections of aflibercept with excellent functional and anatomical results. Although cryotherapy is considered a possible treatment for PEHCR, no previous papers have showed its results or its possible complications for this condition. Besides showing these adverse effects of cryotherapy, our case reinforces the good response to intravitreal aflibercept that was recently demonstrated7. In the meantime, further research into this disease entity is required to more completely identify its underlying pathophysiology and treatment.
REFERENCES
1. Reese AB, Jones IS. Hematomas under the retinal pigment epithelium. Am J Ophthalmol. 1962 Jun;53:897-910.
2. Annesley WH Jr. Peripheral exudative hemorrhagic chorioretinopathy. Trans AM Ophthalmol Soc. 1980;78:321-64.
3. Shields CL, Salazar PF, Mashayekhi A, Shields JA. Peripheral exudative hemorrhagic chorioretinopathy simulating choroidal melanoma in 173 eyes. Ophthalmology. 2009;116(3):529-35.
4. Mantel I, Uffer S, Zografos L. Peripheral exudative hemorrhagic chorioretinopathy: a clinical, angiographic, and histologic study. Am J Ophthalmol. 2009;148(6):932-8.
5. Mantel I, Schalenbourg A, Zografos L. Peripheral exudative hemorrhagic chorioretinopathy: polypoidal vasculopathy and hemodynamic modifications. Am J Ophthalmol. 2012;153(5):910- 22.
6. Goldman D, Freund K, McCannel C, Sarraf D. Peripheral polypoidal choroidal vasculopathy as a cause of peripheral exudative hemorrhagic chorioretinopathy: a report of 10 eyes. Retina. 2013; 33(1):48-55.
7. Sax J, Karpa M, Reddie I. Response to intravitreal aflibercept in a patient with peripheral exudative hemorrhagic. Retin Cases Brief Rep. 2018; Aug 1. Doi: 10.1097/ICB.0000000000000787
8. Seibel I, Hagar A, Duncker T, Riechardt AL, Nürnberg D, Klein JP, et al. Anti-VEGF therapy in symptomatic peripheral exudative hemorrhagic chorioretinopathy (PEHCR) involving the macula. Graefe’s Archive Clin Exp Ophthalmol. 2016;254(4):653-9.
9. Cebeci Z, Dere Y, Bayraktar Ş, Tuncer S, Kir N. Clinical features and course of patients with peripheral exudative hemorrhagic chorioretinopathy. Turk J Ophthalmol. 2016:46(5):215-20.
10. Mashayekhi M, Shields C, Shields J. Peripheral exudative hemorrhagic chorioretinopathy: a variant of polypoidal choroidal vasculopathy? J Ophthalmic Vis Res. 2013;8(3):264-7.
AUTHOR’S INFORMATION
Funding: The authors declare that there was no funding
Conflicts of interest: The authors declare that there is no conflict of interest
Received on:
June 21, 2020.
Accepted on:
August 5, 2020.