Sarah P. D. Maia; Eduardo N. L. Sousa; Pedro V. Franco
DOI: 10.17545/eOftalmo/2020.0013
ABSTRACT
This report describes a clinical case of relapsing polychondritis in a 51-year-old female patient with an ocular history of recurrent scleritis, characteristic of the patient’s systemic disease. Considering the rarity of the condition, we aimed to describe the case of a patient with relapsing polychondritis and ocular involvement, which reinforces the need for greater attention to differential diagnoses for better patient conduct.
Keywords: Relapsing polychondritis; Scleritis; Episcleritis.
RESUMO
Caso clínico de policondrite recidivante é descrito em paciente de 51 anos, do sexo feminino. Apresentando história oftalmológica pregressa de esclerite de repetição, característico do quadro sistêmico da paciente. Tendo em vista a raridade da doença, objetivou-se descrever caso de paciente portadora de policondrite recidivante com acometimento oftalmológico, o que reforça a necessidade de maior atenção aos diagnósticos diferenciais para melhor conduta dos pacientes.
Palavras-chave: Policondrite recidivante; Esclerite; Episclerite.
INTRODUCTION
Relapsing polychondritis is a rare and severe idiopathic condition of an immunological nature. It is characterized by an inflammatory process in the cartilaginous structures throughout the body that contain type II collagen, resulting in tissue damage and destruction. Nasal and auricular cartilages are affected the most; however, other proteoglycan-rich structures, such as peripheral joints, eyes, blood vessels, upper airways, heart, and kidneys, may also be affected1-3.
Heredity does not contribute to the onset of the disease, and both men and women are equally affected. The disease is uncommon in childhood or adolescence, and occurs between the ages 20 and 40 years, with a peak incidence in the fourth decade of life1,4.
The most common findings of relapsing polychondritis are auricular chondritis and polyarthritis, present in >80% of the patients. Recurrent episodes of cartilage inflammation may progress to nasal and auricle deformities, as well as collapse of the cartilaginous tracheal support and hypoacusis5,6. Nonetheless, the most common symptoms are usually absent in the early stages; therefore, the condition may mimic any other rheumatological disease involving joint, ocular, cutaneous, or vestibular dysfunction, which causes delayed diagnosis3. The most common forms of ocular involvement are scleritis and episcleritis, in addition to the equally important uveitis5,6.
As there is no specific test for screening of the disease, the diagnosis is based on the clinical manifestations. The diagnostic criteria were described by McAdam et al. and modified by Damiani and Levine4,5,7: (1) recurrent chondritis of both the auricles; (2) non-erosive inflammatory arthritis; (3) chondritis of the nasal cartilage; (4) inflammation of the ocular structures, including conjunctivitis, keratitis, scleritis/episcleritis, and/or uveitis; (5) chondritis of the larynx and/or trachea; and (6) vestibular and/or cochlear lesion manifested by sensorineural hearing loss, tinnitus, and/or vertigo. The diagnosis requires the presence of three or more of these characteristics and is confirmed by a biopsy, which shows the presence of mononuclear and, occasionally, polymorphonuclear cells, with fibrosis at the fibrochondral junction. Laboratory changes are nonspecific and usually reflect an inflammatory state. The erythrocyte sedimentation rate is often elevated4,5,7.
CASE REPORT
The patient was a 51-year-old female with recurrent pain and inflammation in both eyes.
Her history included a clinical diagnosis of relapsing polychondritis. The diagnosis was made in a medical unit and was based on the presence of classical signs of the disease, such as saddle nose, reduced auditory acuity, dysphonia, dysphagia, and ocular manifestations; hence, she was referred to our service.
She complained of recurrent symptoms of pain and hyperemia in both eyes, at an average of four episodes yearly, for the last five years. Upon the slit lamp examination, she presented dilated conjunctival vessels, sectoral hyperemia, and pain on eye movement. A test was performed with the instillation of 2.5% phenylephrine eye drops, with a negative result, suggestive of non-necrotizing anterior scleritis.
Associated with recurrent scleritis, her ocular history included severe and chronic dry eye, progressing to corneal decompensation in the left eye. Due to the corneal decompensation with eminent perforation, she underwent corneal transplantation of this eye in 2017, which progressed to failure.
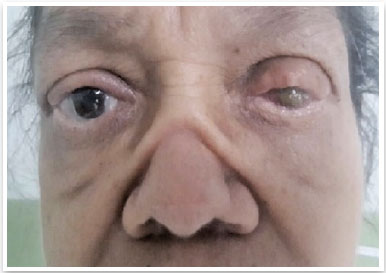
Upon examination, she presented a 20/20 visual acuity in the right eye and no light perception in the left eye. She also presented corneal button opacity in the left eye (Figure 1), for which fundoscopy could not be performed. The right eye fundus was normal.
The ocular alterations that she presented were consistent with those expected in relapsing polychondritis. Combined with the exclusion of other systemic diseases through laboratory tests and clinical evaluation, we reinforced the possibility of this rare diagnosis. Scleritis was then treated with a topical corticoid (prednisolone acetate) and oral nonsteroidal anti-inflammatory drugs. After resolution of this condition, we prescribed lubricant eye drops that were to be used on a continuous basis. Due to poor visual prognosis in the left eye, with no indication for a new corneal transplantation, we opted for expectant management and regular ophthalmologic follow-up, in addition to maintaining systemic follow-up with the attending medical unit team.
DISCUSSION
Ocular involvement is frequently reported in the course of the disease and may precede the systemic clinical picture. Ocular manifestations are found in 50%-70% of the patients and are of great importance because they are correlated with the signs of disease activity1,5.
Scleritis, episcleritis, and iritis are the major ocular manifestations of the disease, with diffuse anterior scleritis being observed most frequently. Uveitis occurs in 35% of the cases and presents as anterior uveitis or sclerouveitis. Relapses and exacerbations are common. Additionally, ocular tissue can be affected by proptosis, corneal perforation, retinal vasculitis, and optic neuritis, which can cause blindness, as in the case of the patient in this report8,9.
Another important factor in the described picture was the severe dry eye. Both scleritis and dry eye were significant in this case, impacting the patient’s quality of life and visual prognosis.
The treatment was customized according to the severity and location of the disease. Mild forms of relapsing polychondritis are treated with anti-inflammatory and antineutrophilic agents. Advanced cases, including those involving acute airway obstruction, multiple relapses, and cardiovascular diseases, may require high doses of prednisone (1mg/kg per day) or even pulse therapy with intravenous methylprednisolone. Although plasmapheresis, azathioprine, chlorambucil, and cyclosporine may be beneficial, some patients do not respond to any of them6,9. Clinical cases with ocular involvement are treated with topical steroids and low doses of oral prednisolone or oral nonsteroidal anti-inflammatory drugs, usually with the control of episcleritis and/or uveitis attacks, as described in this clinical case.
Given the rarity of this disease, we aimed to describe the case of a patient with this condition presenting ocular involvement with recurrent scleritis and severe dry eye. This reinforces the need for greater attention to differential diagnoses for better patient conduct.
REFERENCES
1. Guimarães VC, Nery GV, Araújo FGM, Barbosa MA, Ferreira JB. Manifestações clínicas na Policondrite Recidivante: relato de caso. Rev Eletr Enf. 2008;10(3):823-7.
2. Longo L, Greco A, Rea A, Lo Vasco VR, De Virgilio A, De Vincentiis M. Relapsing polychondritis: A clinical update. Autoimmun Rev. 2016;15:539-43.
3. Hasanreisoğlu M, Özdemir HB, Yaylacıoğlu F, Ertop M, Aktaş Z. Bilateral Anterior Uveitis Revealing Relapsing Polychondritis. Turk J Ophthalmol. 2019;49(2):99-101. doi:10.4274/tjo.galenos. 2018.28909
4. Leite DRC, Junior RRT, Freire EAM. Asma brônquica como manifestação clínica de Policondrite Recidivante: relato de caso e revisão de literatura . Paraíba: Universidade Federal da Paraíba. 2013.
5. Bradley JC, Schwab IR. Blue ear sign in relapsing polychondritis. Rheumatology (Oxford). 2011;50(2):427. doi: 10.1093/rheumatology/keq390. Epub 2010 Nov 28.
6. Cavalcanti A, Barbosa CMPL, Len CA, Terreri MTRA, Hilário MOE. Policondrite recidivante na infância: relato de caso e revisão da literatura. Rev Bras Reumatol. 2007;47(3):223-7.
7. Rodrigues EM, Silveira RCN, Leite N, Tepedino MM. Policondrite recidivante: relato de caso. Rev. Bras. Otorrinolaringol. [online]. 2003;69(1):128-30.
8. Sallam A, Islam T, Parmar DN. Keratouveitis as a first presentation of relapsing polychondritis. Case Rep Med. 2010;2010:176514. doi: 10.1155/2010/176514. Epub 2010 Oct 28.
9. Leroux G, Costedoat-Chalumeau N, Brihaye B, Cohen-Bittan J, Amoura Z, Haroche J, et al. Treatment of relapsing polychondritis with rituximab: a retrospective study of nine patients. Arthritis Rheum. 2009;61(5):577-82.
AUTHOR’S INFORMATION
Funding: The authors declare that there was no funding
Conflicts of interest: The authors declare that there is no conflict of interest
Received on:
March 9, 2020.
Accepted on:
June 17, 2020.