Aline Cristina Fioravanti Lui Alionis1,2; Adamo Lui Netto3; Tatiana Adarli Fioravanti Lui Netto3; Milton Ruiz Alves1
DOI: 10.17545/eOftalmo/2020.0011
ABSTRACT
OBJECTIVE: Compared to standard spectacle lenses (non-blue-blocking), do blue-blocking lenses reduce symptoms of asthenopia induced by computer?
METHODS: A prospective clinical study was carried out with 49 volunteers who spent more than 4 hours a day using a computer (age, 29.07±5.50; male: female=18:31). Digital asthenopia was assessed using a questionnaire. All participants completed the questionnaire with standard spectacles non blue-blocking (baseline) and after 4 weeks with a blue-blocking lens (Crizal® Prevencia™) wearing. The normality of data was assessed using the Shapiro-Wilk test. Changes in measured values were compared using the non-parametric Wilcoxon test and p-values less than 0.05 were considered statistically significant.
RESULTS: Compared to standard spectacle lenses (standard spectacle lenses (non-blue-blocking), blue-blocking lenses wearing reduced the total asthenopia score from 17.61±5.51 to 13.78±7.51 (p<0.001).
CONCLUSIONS: Digital asthenopia baseline induced by computer was significantly reduced by blue-light blocking spectacle lenses blue wearing.
Keywords: Computer syndrome vision; Asthenopia; Risk-factors; Occupational diseases; Occupational medicine.
RESUMO
OBJETIVO: Comparadas com lentes oftálmicas que não filtram a luz azul, as lentes com filtro azul reduzem os sintomas de astenopia induzida por computador?
MÉTODOS: Foi realizado em estudo clínico prospectivo com 49 voluntários que passavam mais de 4 h diárias utilizando computador (idade, 29,07±5,50; masculino: feminino=18:31). A astenopia digital foi avaliada com questionário. Os participantes responderam ao questionário no uso de lentes oftálmicas sem filtro azul (baseline) e após 4 semanas de uso das lentes com filtro azul (Crizal® Prevencia™). A normalidade dos dados foi avaliada usando o teste Shapiro-Wilk. Alterações nos escores dos sintomas de astenopia foram comparadas usando o teste não paramétrico de Wilcoxon e valores de p inferiores a 0,05 foram considerados estatisticamente significativos.
RESULTADOS: Comparadas com lentes oftálmicas que não filtram a luz azul (baseline), o uso das lentes com filtro azul reduziu o escore total de astenopia digital de 17,61±5,51 para 13,78±7,51 (p<0,001).
CONCLUSÕES: A astenopia digital baseline induzida pelo computador foi significativamente reduzida no uso de lentes que filtram a luz azul.
Palavras-chave: Síndrome visual do computador; Astenopia; Fatores de risco; Doenças ocupacionais; Medicina ocupacional.
INTRODUCTION
The number of computer users is rising exponentially worldwide; however, working at a computer terminal is not free from health hazards to eyes as it puts significant stress on visual functions1. Workers that spend more than 4 hours daily working on video display terminals (VDTs) can report visual fatigue and discomfort2 derived from insufficient visual capabilities to perform the computer task comfortably - digital asthenopia (DA)3. The most common symptoms associated with DA are tired eye, sore/aching eye, irritated eye, watery eye, dryness, eye strain, hot/burning eye, blurred vision, difficulty in focusing, and visual discomfort4. It is estimated that approximately 65% of American citizens suffer from DA to some degree5. It has become a significant public health problem6.
Blue light emitted by digital devices has also been implicated as a cause of DA7. Isono et al.8 reported reduced ocular subjective complaints in young adults when reading from a sepia background (reduced blue light contribution) compared with the conventional white background of a modern tablet device. Cheng et al.9 showed in dry eye (DE) a reduction in ocular complaint scores with all blue filter levels tested. Ide et al.10 reported that the group submitted to a high blockage of blue light reported fewer eye symptoms post-task compared with other groups.
Blue-blocking (BB) spectacle lenses that attenuate short-wavelength light are being marketed to alleviate eye strain and discomfort when using digital devices, improve sleep quality, and potentially confer protection from retinal phototoxicity11. The purpose of the present study was to evaluate the effects of BB spectacle lenses on computer-induced asthenopia.
METHODS
This prospective clinical study followed the tenets of the Declaration of Helsinki and was approved by the Research Ethics Committee of Faculty of Medicine, University of São Paulo, São Paulo, Brazil (87584318.1.3001.0065; 10/16/2018). Written informed consent was obtained from participants before their enrollment. The inclusion criteria were: (i) healthy adults aged 20-40 years who spend more than 4h daily working on VDTs, and (ii) refractive errors with spherical components between ±4D and cylindrical between ±2.00D corrected with updated glasses without BB blocking. The exclusion criteria were: (i) active condition of an allergic, inflammatory or infectious nature, on the ocular surface; (ii) users of medications that influence the vision and/or muscle function; (iii) contact lens wearers; (iv) strabismus and/or amblyopia; and (v) anisometropia greater than 1.50 D. Forty-nine eligible volunteers were recruited.
Ophthalmic screening test for participants included slit-lamp microscopy, cover and cover-uncover tests, non-contact intraocular pressure measurement, accommodation amplitude, and near the point of convergence measurements, ocular refraction under cycloplegia, corrected distance visual acuity and indirect fundoscopy.
After passing the screening test, all subjects were designated to receive a new blue-light blocking spectacle lens (Crizal® Prevencia™) fitted in a similar frame with the same optical corrections. Asthenopia was evaluated by using a modified questionnaire proposed by Ames et al.4 These questionnaires consisted of 10 questions related to asthenopia that needed to be responded to using a scale of 0-6, with zero defined as none and six as most severe. Most severe asthenopia corresponded to a score of 60. All subjects completed the questionnaire with standard spectacle lenses (non-BB) and after four weeks with BB lenses wearing. Statistical analyses were performed using R Studio Program ver. 1.2.5001 (RStudio, Boston, MA, USA). Since the assumption of normality was rejected (Shapiro-Wilk test), comparisons of both glasses regarding asthenopia scores were made with the non-parametric Wilcoxon test and p-values less than 0.05 were considered statistically significant.
RESULTS
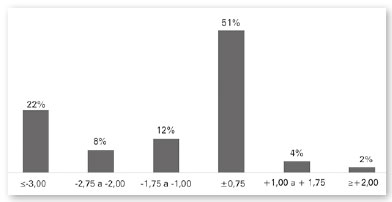
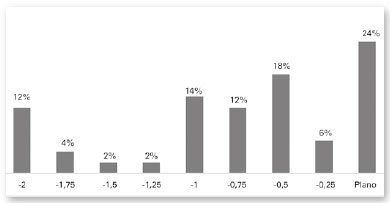
The age of the participants was 29.07±5,50 years (20-39 years), is 31 (63%) females, and 18 (37%) males. Concerning the educational level, 45 (92%) were college or above. Thirty-six (73%) participants reported three or more digital devices viewed simultaneously in daily life, while 42 (86%) reported everyday computer use for more than 6 hours. Ametropia distribution by the mean sphere of the right eye is shown in figure 1. The cylinder distribution of the right eye is shown in figure 2.
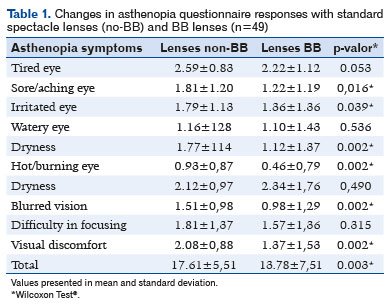
The means of the AA and PPC measurements were 11.88±1.50D and 6.82±3.50cm, respectively. Total asthenopia score with standard spectacle lenses (no- BB) was 17.61±5.51 (maximum possible total asthenopia score was 60). Tired eye, sore/aching eye, and visual discomfort mean scores were above 2.0. After four weeks with spectacle lenses, BB the ratings for six items (tired eye, dryness, eye strain, hot/burning eye, blurred vision, and visual discomfort) were significantly decreased and the total asthenopia score reduced to 13.78±7,51 (p<0.001) (Table 1).
DISCUSSION
In the present study, the computer screen watching was shown to significantly affect subjective asthenopia symptoms accessed by the questionnaire (Table 1). Total asthenopia score in the standard spectacle lenses (non-BB) wearing was 17.61±5.51. After four weeks of spectacle lenses BB wearing, the scores for six symptoms were significantly decreased, and the total asthenopia score has been reduced to 13,78±7,51; p<0.001.
However, DA is a multifactorial condition with several potential contributory causes, such as uncorrected refractive error, oculomotor diseases, tear abnormalities, and/or musculoskeletal problems12. The subjects recruited for the study had their refractive errors properly corrected and did not present oculomotor diseases or accommodative or converge problems. AA and PPC measurements were considered individually within normal limits.
Sheedy et al.13 described two distinct mechanisms and sets of symptoms related to DA. External symptoms of tired, sore/aching, irritated, watery, hot/burning, and dryness were noted to be closely related to DE, while internal symptoms of blurred vision, difficulty in focusing, and visual discomfort were linked to accommodative and/or binocular vision stress. In the study, the most symptoms mean scores related to the DE decrease with spectacle lenses BB wearing.
Computer use affects blink patterns, ocular surface homeostasis, and tear film function14-16. In normal healthy subjects, the results show an average 5-fold drop in blink rate during VDU17,18. Reduced blink rate and a higher proportion of incomplete blinks with computer use leads to a greater evaporative loss of tears19, reduction of mucin production20, increase of inflammatory markers, and tear osmolarity21, causing increased of external symptoms19.
Regarding changes in optical quality and due to tear film dynamics, most studies have focused on the changes in corneal or ocular higher-order aberrations between blinks using corneal topographers or Shack-Hartmann wavefront sensors22-24. However, Kaido et al.25 focused on a possible relationship between tear stability and visual function in blue light exposure. The shorter wavelengths of visible white light, such as blue light emitted by digital screens, are more strongly scattered than the longer wavelengths as they pass through the intraocular structures to reach the retina. Spectacle lenses BB placed in front of the eye blocks the passage and intraocular dispersion of blue light, improving visual efficiency25. Kobashi et al.26 had suggested that the increase of intraocular scattering could have a considerable impact on the deterioration of visual performance and may also aggravate DE symptoms, including eye fatigue, leading to headaches and physical and mental fatigue caused by long exposure to VDTs or other electronic screen-based devices.
BB spectacle lenses (Crizal® Prevencia™) used in this study, reduce the quantity of blue-violet light (415nm to 455nm) reaching the eye by 20% and allow beneficial light to pass through (visible light, including blue-turquoise)27. BB spectacle lenses with more than 70% of blue-light transmission do not significantly affect contrast sensitivity, color vision, and visual performance28. The calculation indicates that BB spectacle lenses theoretically reduced by 10.6% to 23.6% of the potential phototoxicity by blocking the hazardous radiation between 400 to 500nm28. Crizal® Prevencia™ lens effectiveness has been demonstrated using the same A2E-loaded RPE tissue culture model used to discover the sub-band of blue-violet light that causes RPE apoptosis29. When A2E-containing-RPE cells were exposed to the white light that mimicked the solar spectrum, placing this BB lens between the light source and the cells reduced cell apoptosis by 25% compared to no light filtering at all30. As this BB lens allows 80% of the visible spectrum to enter the eye at a normal level, the eye’s necessary visual and non-visual functions can be maintained while exposure to hazardous wavelengths is reduced28. The non-visual functions depend on photosensitive retinal ganglion cells (ipRGCs), which contain melanopsin and form a photoreceptive network broadly across the inner retina31. The ipRGC response to light in the chronobiological band (at about 480nmr) regulates many non-visual physiologic functions in the human body, including circadian entrainment, melatonin regulation, pupillary light reflex, cognitive performance, mood, locomotor activity, memory, and body temperature32-34.
On digital screens, the characters are getting smaller and more pixelated, and the eyes are constantly more exposed to the bright light35. Spectacle blue-light filtering lenses reduce screen brightness27,28, blocks harmful blue light29.30, and do not significantly affect visual performance28. This investigation showed that in comparison to standard (non-BB) spectacle lenses, BB lenses reduced symptoms of asthenopia digital significantly. However, one limitation of this study was the evaluation of DA using a questionnaire since the responses are somewhat subjective and can be affected by responders’ daily physical and mental conditions36.
REFERENCES
1. Filon FL, Drusian A, Ronchese F, Negro C. Video Display Operator Complaints: A 10-Year Follow-Up of Visual Fatigue and Refractive Disorders. Int J Environ Res Public Health 2019;16(14):2501.
2. Hayes JR, Sheedy JE, Stelmack JA, et al. Computer use, symptoms, and quality of life. Optom. Vis Sci 2007;84(8):738-744.
3. Vaz FT, Henriques PS, Silva DS, et al. Asthenopia: Portuguese Group of Ergophthalmology Survey. Acta Med Port 2019;32(4):260-265.
4. Ames SL, Wolffsohn JS, McBrien NA. The development of a symptom questionnaire for assessing virtual reality viewing using a head-mounted display. Optom Vis Sci 2005;82(3):168-176.
5. Zhao HL, Jiang J, Yu J, Xu HM. Role of short-wavelength filtering lenses in delaying myopia progression and amelioration of asthenopia in juveniles. Int J Ophthalmol. 2017;10(8):1261-1267.
6. Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol 2005;50(3):253-262.
7. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement, and amelioration. BMJ Open Ophthalmology 2018;3:e000146.
8. Isono H, Kumar A, Kamimura T, et al. The effect of blue light on visual fatigue when reading on LED-backlit tablet LCDs. Proceedings of International Display Workshops 2013.
9. Cheng H-M, Chen S-T, Hsiang-Jui L, et al. Does blue light filter improve computer vision syndrome in patients with dry eye? Life Science Journal 2014;11:612-5.
10. Ide T, Toda I, Miki E, et al. Effect of blue light-reducing eyeglasses on critical flicker frequency. Asia Pac J Ophthalmol 2015;4:80-5.]
11. Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health, and the sleep-wake cycle: a systematic review of the literature. Ophthalmic and Physiological Optics, 2017;37:644-54.
12. Gowrisankatan S, Sheedy JE. Computer vision syndrome: a review. Work 2015; 52:303-314.
13. Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optom Vis Sci 2003;80:732-9.
14. Freudenthaler N, Neuf H, Kadner G, et al. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol 2003; 241:914-20.
15. Koslowe KC, Waissman H, Biner-Kaplan M. The blink frequency relationship between reading from a computer screen and reading from a printed page. Optom Vis Develop 2011; 42:168.
16. Rosenfield M, Jahan S, Nunez M et al. Cognitive demand, digital screens, and blink rate. Comput Human Behav 2015; 51:403-406.
17. Patel S, Henderson R, Bradley L, et al. Effect of visual display unit use on blink rate and tear stability. Optometry and Vision Science 1991;68(11):888-892.
18. Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med 1993; 328(8):584.
19. Belmonte C, Nichols JJ, Cox SM, et al. TFOS DEWS II pain and sensation report. Ocul Surf 2017; 15(3):404-437.
20. Uchino Y, Uchino M, Yokoi N, et al. Alteration of tear mucin 5AC in office workers using visual display terminals: The Osaka Study. JAMA Ophthalmol 2014; 132(8):985-992.
21. Fenga C, Aragona P, Di Nola C et al. Comparison of ocular surface disease index and tear osmolarity as markers of ocular surface dysfunction in video terminal display workers. Am J Ophthalmol 2014; 158(1):41-48.
22. Montés-Micó R, Cáliz A, Alió JL (2004) Wavefront analysis of higher-order aberrations in dry eye patients. J Refract Surg 20(3): 243-247.
23. Koh S, Maeda N, Kuroda T, Hori Y, Watanabe H, et al. (2006) Serial measurements of higher-order aberrations after blinking in normal subjects. Invest Ophthalmol Vis Sci 47(8):3318-3324.
24. Koh S, Maeda N, Hirohara Y, Mihashi T, Bessho K, et al. (2008) Serial measurements of higher-order aberrations after blinking in patients with dry eye. Invest Ophthalmol Vis Sci 49(1):133-138.
25. Kaido M, Toda I, Obayashi T, et al. Reducing Short-Wavelength Blue Light in Dry Eye Patients with Unstable Tear Film Improves Performance on Tests of Visual Acuity. PLoS One 2016; 11:e0152936.
26. Kobashi H, Kamiya K, Yanome K, et al. Longitudinal assessment of optical quality and intraocular scattering using the double-pass instrument in normal eyes and eyes with short tear breakup time. PLoS One. 2013; 8:e82427.
27. Geller M. Everything to Know About Blue Light and Crizal Prevencia. Available: https://covalentcareers.com/resources/everything-to-know-about-blue-light-crizal-preventia/.
28. Leung TW, Li RW-Hong, Kee C-S. Blue-Light Filtering Spectacle Lenses: Optical and Clinical Performances. PLoS One 2017;12: e0169114.
29. Arnauld E, Barrau C, Nanteau C et al. Characterization of the blue light toxicity spectrum on A2E-loaded RPE cells in sunlight normalized conditions. IOVS 2013;.54: 6101.
30. Arnault E, Barreau C, Nanteau C, et al. Phototoxic action spectrum on a retinal pigment epithelium model of age-related macular degeneration exposed to sunlight normalized conditions. PLoS One. 2013;8(8):e71398.
31. Berson DM. Phototransduction in ganglion-cell photoreceptors. Pflugers Arch Eur J Physiol. 2007;454: 849-855.
32. Gamlin PD, McDougal DH, Pokorny J, et al. Human and macaque pupil responses driven by melanopsin-containing retinal ganglion cells. Vision Res. 2007;47(7):946-54.
33. Viénot F, Bailacq S, Rohellec JL. The effect of controlled photopigment excitations on pupil aperture. Ophthalmic Physiol Opt. 2010;30(5):484-91.
34. Mure LS, Cornut PL, Rieux C, et al. Melanopsin bistability: a fly eye’s technology in the human retina. PLoS ONE. 2009;4(6):e5991.
35. Benoît C, Jarrousse M. New ophthalmic lenses for a connected life: Eyezen for ametropes and emmetropes, and Varilux Digitime for presbyopes. Points de Vue - International Review of Ophthalmic Optics Special edition - Collection of articles from 2005-2017:107-21.
36. Kim DJ, Lim C, Gu N et al. Visual fatigue induced by viewing a tablet computer with a high-resolution display. Korean J Ophthal 2017;31:388-393.
AUTHOR’S INFORMATION


Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
May 25, 2020.
Accepted on:
July 21, 2020.