Paulo de Souza Segundo1; Gleyse Karina Lopes de Oliveira Pinheiro1; Eduardo Pereira de Azevedo1; Fausto Guzen Pierdoná1; Irami Araújo Filho1; Amália Cinthia Meneses Rêgo1; Ítalo Medeiros de Azevedo2; Francisco Irochima Pinheiro1
DOI: 10.17545/eOftalmo/2019.0029
ABSTRACT
PURPOSE: Evaluate the knowledge regarding the theoretical calculation of refractometry among professionals who prescribe eyeglass lenses and develop a new simulator application to assist them in this task.
METHODS: A questionnaire was developed and answered by 51 randomly selected professionals with the purpose of evaluating their level of knowledge about the theoretical calculation of refractometry, where they were divided into five groups according to their ages. The results regarding the performance of each group were analyzed and a simulator application (App) named HELPER KERATOCONUS, was developed, tested and made available at the online Apple store.
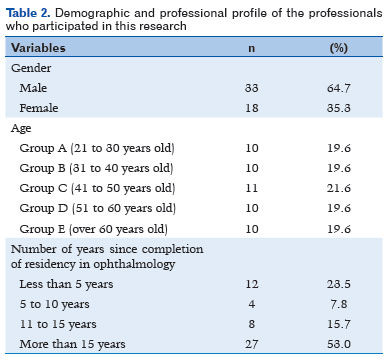
RESULTS: 18 professionals were female (35.3%) and 33 (64.7%) were male. 27 (53%) had completed their residency in ophthalmology for more than 15 years and only 4 (7.8%) had completed for 5 to 10 years. The software was then developed and after 30 days of blind and randomly performed simulations involving volunteer specialists, only two faults were detected and promptly corrected.
CONCLUSION: A need for improvement in the knowledge of professionals who prescribe eyeglass lenses regarding the theoretical calculation of refractometry was evidenced. Therefore, a new application software was developed and made available at full functionality to assist them in this task.
Keywords: Keratoconus; Refractive errors; Simulation; Mobile applications; Medical informatics.
RESUMO
OBJETIVO: Avaliar o conhecimento sobre o cálculo teórico da refratometria entre profissionais que prescrevem lentes de óculos e desenvolver um novo aplicativo simulador para auxiliá-los nessa tarefa.
MÉTODOS: Um questionário foi desenvolvido e respondido por 51 profissionais selecionados aleatoriamente com o objetivo de avaliar seu nível de conhecimento sobre o cálculo teórico da refratometria, onde foram divididos em cinco grupos de acordo com suas idades. Os resultados referentes ao desempenho de cada grupo foram analisados e um aplicativo simulador (App) denominada HELPER KERATOCONUS, foi desenvolvido, testado e disponibilizado na loja online da Apple.
RESULTADOS: 18 profissionais eram do sexo feminino (35,3%) e 33 (64,7%) do sexo masculino. 27 (53%) completaram a residência em oftalmologia por mais de 15 anos e apenas 4 (7,8%) completaram por 5 a 10 anos. O software foi então desenvolvido e após 30 dias de simulações cegas e aleatórias realizadas envolvendo especialistas voluntários, apenas duas falhas foram detectadas e prontamente corrigidas.
CONCLUSÃO: Evidenciou-se a necessidade de aprimoramento do conhecimento dos profissionais que prescrevem lentes de óculos quanto ao cálculo teórico da refratometria. Portanto, um novo software aplicativo foi desenvolvido e disponibilizado com funcionalidade total para auxiliá-los nessa tarefa.
Palavras-chave: Ceratocone; Erros refrativos; Simulação; Aplicações móveis; Informática médica.
INTRODUCTION
Keratoconus involves non-inflammatory corneal ectasia, which results in a gradual and bilateral increase in curvature and asymmetrical thinning of the stroma(1,2). Its prevalence is variable, reaching 5.2% in some countries, including India(3,4). In general, it occurs in childhood or puberty, and patients may show progressive presentation until the third or fourth decade of their life, possibly associated with atopy and eye allergies(1,4-7).
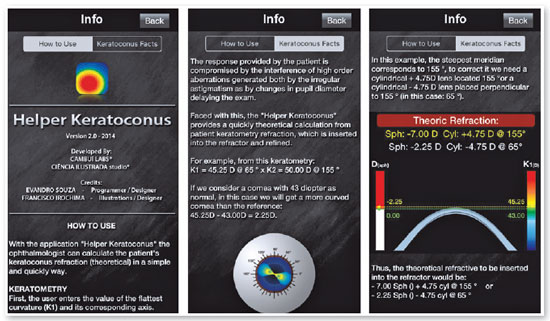
The optical effect resulting from keratoconus progression leads to impairment of visual acuity due to the emergence of irregular astigmatism(1,8). Thus, the presence of this deformity also makes it difficult to calculate the patient’s refraction, either through retinoscopy (skiascopy) or using an autorefractor(9-11). Therefore, in some cases, it is difficult to obtain refraction values rapidly and reliably during ophthalmological practice. In addition, in such patients, the results are compromised and inaccurate due to the interference of high-order aberrations generated both by irregular astigmatism and altered pupil diameter and keratoconus location, which further delay refractometric examinations(5,9-12).
Theoretical and practical knowledge of the examiner is a primary factor in achieving rapid and accurate refractometric data of patients with keratoconus for whom objective refractometric resources are inaccurate(5,9,10). However, not all professionals who prescribe glasses or lenses have accumulated enough experience during the years of clinical practice. Therefore, the use of technologies that help the newly specialized professionals and allow the experienced ones to remain up-to-date is a great advance in ensuring the accuracy of refraction calculation in patients with keratoconus(13-17).
In this context, development of a simulator, which can serve as a rapid and practical tool for the theoretical measurement of refraction based on a patient’s keratometry results and which can be inserted in the refractor and refined later by the examiner, will optimize the refractometric examinations of patients with keratoconus.
METHODS
The project was developed in partnership with the company Ciência Illustrada studio® housed in the INOVA metropolis of the Instituto Metrópole Digital of the Federal University of Rio Grande do Norte (IMD-UFRN), following a schedule that was divided into three stages. The first stage included the assessment of knowledge on theoretical calculation of refraction based on patients’ keratometry results among professionals who prescribe glasses in Brazil. The second stage included graphic development and programming of a simulator application to assist professionals caring for patients with keratoconus, those in whom skiascopy is difficult, and those with erroneous measurements of refraction using an autorefractor. Finally, the third stage included testing the simulator application to detect possible application failures.
Evaluation of knowledge on the theoretical calculation of refraction
Fifty-one Brazilian professionals who prescribe glasses or lenses were randomly selected to answer a questionnaire with five unprecedented multiple choice questions, each with five possible answers, to explore their knowledge on the theoretical calculation of refraction in patients with keratoconus. The inclusion criterion was being a practicing ophthalmologist, and the exclusion criterion was lack of this credential. The questionnaire was sent to several groups of a communication network. The study was double-blind. The professionals were instructed to answer the questions without the assistance of external consultation. The questionnaire also explored data such as age, sex, and year of completion of specialization. According to the time of specialization completion, the professionals were separated into four groups: <5 years, 5-10 years, 11-15 years, and >15 years of specialization. The professionals were again divided into five groups (A, B, C, D, and E) according to their age group. Group A comprised professionals aged 21-30 years, group B comprised professionals aged 31-40 years, group C comprised professionals aged 41-50 years, group D comprised professionals aged 51-60 years, and group E comprised professionals aged >60 years.
A value of 2 points was assigned for each question, making a total value of 10 points as the maximum performance score. At the end, the results were compiled and analyzed. A score was assigned according to the correct responses of each professional, and means with standard deviation, medians, and 2nd and 3rd quartiles were calculated for each group.
Qualitative variables were expressed as absolute and percentage values. Data on continuous quantitative variables were expressed as mean±standard deviation or median and 2nd and 3rd quartiles. The qualitative variables were presented as absolute and relative frequencies.
Initially, the normality assumption was assessed using the Shapiro-Wilk and Kolmogorov-Smirnov tests. For the variable “number of correct answers,” the non-parametric Kruskal-Wallis and Mann-Whitney tests were used to verify the existence of a statistically significant difference between different times of completion of the specialization and sexes, respectively. The statistical package SPSS® 21 was used. The significance level adopted was 5%.
Graphic development and software programming
The HELPER KERATOCONUS software was developed by the company Ciência Illustrada studio®. Drawings used to illustrate the application were created in CorelDRAW® X8 (Corel Corporation, Ottawa, Canada) by one of the authors (Pinheiro, FI), who is an ophthalmologist and illustrator; coding was performed by an experienced programmer using XCode 4.6.2 (Apple® Computer, Inc. Cupertino, CA, USA). The application was created for tablets and smartphones on the IOS platform (iPhone OS®), with a home screen containing two basic areas: an upper area and a lower area. The upper area contains boxes for inserting the keratometry values on the left and a frontal schematic eye for the simulation of the corneal normalized theoretical topography on the right. The lower area presents both theoretical refraction values and graphical representation of a standard cornea in the sagittal view (Figure 1).
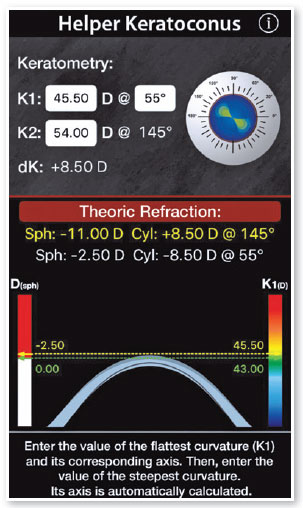
Keratometry readings are entered in two boxes and can range from 30.00 diopters (D) to 70.00 D, with increases of 0.01 D. The first box, K1, represents the smallest value or the flattest keratometry reading, which must be accompanied by the value of its axis in degrees. The values entered in the axis box can vary from 0° to 180°, with increases of 1°. When entering the value of K2 in the second box, the second axis is automatically calculated considering a difference of 90° (perpendicular axes). After entering the values of K1 and K2, the user can remove individual values of the boxes using the “Clear” key or remove all values using the “Clear All” key. The “Next” key directs the user to the next box to enter the next value. The “Done” key ends the insertion of the values for K1, K2, and their respective axes. After this is done, representation of the dK appears below the K2 box, which represents the difference between the K2 and K1 values (K2 − K1), and representation of the simulated topography of the cornea appears in the schematic eye (Figure 2). Theoretical refraction values using positive and negative cylinder format are shown at the bottom of the screen, and comparison with the virtual cornea resulting from the keratometry values of a spherical standard cornea with K1 and K2 of 43 D appears further below. In this comparison, two columns are shown joined by a dotted line: one on the right [D (sph)] and one on the left [K1 (D)]. Column D (sph) indicates by how many D the K1 (flattest keratometry reading) is more curved or flatter than the standard cornea, while column K1 (D) represents the actual value of K1 (Figure 2).
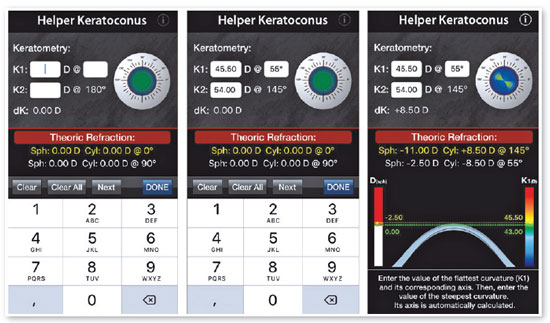
In the upper corner there is an “i” symbol for the INFO on the application and on where to find the “How to Use” and “Keratoconus Facts” with a brief explanation of how they work (Figure 3).
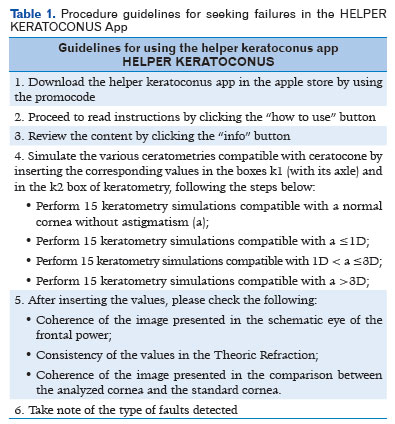
Simulated tests for error detection
After its development, the HELPER KERATOCONUS application was tested in a blind and random manner by four experienced ophthalmologists who received the designations I, II, III and IV. For 90 days, the four ophthalmologists followed a specific script (Table 1) to detect possible errors through simulations. Once errors were identified, the program was corrected and retested by the same ophthalmologists that had detected the errors to confirm that they were corrected.
RESULTS
The collected data showed that among the 51 professionals who answered the questionnaire, 18 (35.3%) were women and 33 (64.7%) were men. Groups A, B, D, and E each had 10 individuals (19.6%), while group C had 11 individuals (21.6%). Twelve individuals (23.5%) had <5 years of specialization, four (7.8%) had 5-10 years of specialization, eight (15.7%) had 11-15 years of specialization, and 27 (53.0%) >15 years of specialization (Table 2).
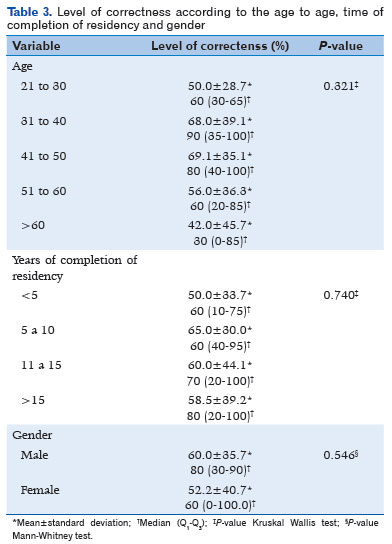
Analysis of answers to questions related to the theoretical calculation of refraction showed the following means and standard deviations of “number of correct answers” according to age group: group A (21-30 years)=5.0 (50.0%±28.7%) points; group B (31-40 years)=6.8 (68.0%±39.1%) points; and group C (41-50 years)=6.9 (69.1%±35.1%) points; group D (51-60 years)=5.6 (56.0%±36.3%) points; and group=4.2 (42.0%±45.7%) points. When the time of specialization was taken into account, the results were as follows: <5 years=50.0%±33.7%; 5-10 years=65.0%±30.0%; 11-15 years=60.0%±44.1%, and >15 years=58.5%±39.2%. Considering all professionals involved in the study, the overall mean was 57.3%±37.3%.
There was no significant difference (p>0.05) between the number of correct answers of the interviewees among groups by age, time of specialization, or sex (Tables 2 and 3).
Regarding development of the new teaching tool, after 3 months of specialized testing, an error was reported in the simulation of topography by ophthalmologist I and another error was detected by ophthalmologist III during the comparison with the standard cornea. The program was corrected and retested by the same ophthalmologists who detected the respective errors. After the retest and confirmation of the corrections, the application was made available in the Apple® store for download via the link: https://itunes.apple.com/br/app/helperkeratoconus/id559759718?mt=8.
DISCUSSION
Need for continuing education and regular updating of knowledge is justified by the proven decline in its retention over the years, as reported by Gomez-Perez and Ostrosky(18). Using several tests to evaluate executive and memory functions in adult individuals, these researchers found that the ability to remember is sensitive to age, while attention and executive functions are sensitive to years of educational training(19). Similarly, Carriere et al presented decline in cognitive performance with the advancement of age(19). In that study, which analyzed 638 individuals between 14 and 77 years of age, although the authors observed a better sustained attention to response task performance with advancing age, the speed of response declined linearly over the years(19).
During evaluation of the knowledge on theoretical calculation of refraction by professionals prescribing glasses in the present study, it was found that neither age nor the time elapsed since specialization affected the performance. Given these results, it is plausible to expect that professionals in the older age group and with more years of specialization, that is, more experienced, would have the best performance or a worse result according to premises of cognitive decline with age. However, according to the results, this would be a mistaken conclusion, because when the statistical tests were applied no significant differences were observed. However, the size and heterogeneity of the sample may have influenced the non-statistical difference obtained between the groups in terms of knowledge. However, because the overall mean of correct answers was 57.3%±37.3%, it is clear that this sample of individuals were in need of an improvement in knowledge regarding the theoretical calculation of refraction based on keratometry readings. However, this statement cannot be extrapolated to all professionals prescribing glasses in the country.
As shown by Leitritz et al (2014), improvement during the teaching/learning process in ophthalmology when simulators are used is evident(20). Several other digital tools (software) also have advantages over conventional teaching methods(21,22). The EYE Exam Simulator (Kyoto Kagaku Co. Ltd., Kyoto, Japan®), the Eyesi direct ophthalmoscope (VRMagic, GmbH, Mannheim, Germany®), and the Eyesi indirect ophthalmoscope simulator (VRMagic, GmbH, Mannheim, Germany®) are the examples of simulators that assist in the teaching/learning process in ophthalmology by using mannequins and virtual or augmented reality, respectively(21-23).
Although several educational technologies in the form of multimedia software and simulators for medical training are already available to be used both during the teaching of ophthalmology and in the support of continuing education during the process of retraining professionals in clinical practice, few focus on refractometry(21-23). In addition, the ability to calculate the theoretical value of refraction from keratometric readings of a cornea requires knowledge of mathematics and spatial geometry, which is not a common skill among professionals who prescribe glasses. Therefore, the availability of a resource that facilitates the transmission of this knowledge represents an unprecedented innovation to consolidate teaching(14,24-27).
Few applications are available. Aniseikonia Inspector calculates the difference in image size (aniseikonia) induced by correction in patients with anisometropy, but there is no reference of any software that assists in the theoretical calculation of refraction from keratometry readings of patients with advanced keratoconus(28,29).
Given the need for practical and agile technological tools to help the teaching of refractometry for both the newly specialized and established professionals, the authors of this study developed a series of applications. In the article “A virtual simulator as a tool for teaching refractometry,” Pinheiro et al. describesd the development of the application (Eye Refraction) created for tablets that presents the various refractive errors (ametropias) of the optical system of the eye in a totally interactive way, with the possibility of correction with the most diverse combinations of lenses(30). As in the application Eye refraction, the graphic design of the application developed in the present study was the responsibility of one of the experienced authors, an ophthalmologist and scientific illustrator. This ensured that the difficulties in the process of assimilation of information were circumvented through an optimized graphical presentation(30).
Two corrections had to be performed in the application software after error detection. The bugs were fixed, and the application was made available in the Apple store. However, this procedure will not prevent future errors from occurring during the use of the application by users. For this reason, developers have provided a link in the application itself for users to point out future errors that require fixing after the application becomes available.
Because the application has been developed to run on tablets and smartphones, it can be easily used in offices and classrooms and even outside the teaching environment, with high accessibility and mobility because it does not require internet access. It is less expensive than other types of simulators available for teaching ophthalmology, and it is a tool accessible to all professionals because it has an easy and interactive application/user interface. One disadvantage is that it is only available on the IOS platform, although the prospect is to also develop the application for the Android platform.
Thus, the HELPER KERATOCONUS simulator represents the second in a series of applications developed by the authors with an aim to demystify the teaching of refractometry and contribute directly to the training of future professionals and, consequently, to the eye health of the population.
REFERENCES
1. Shetty R, Kaweri L, Pahuja N, et al. Current review and a simplified "five-point management algorithm" for keratoconus. Indian J Ophthalmol. 2015;63:46-53.
2. Vazirani J, Basu S. Keratoconus: Current perspectives. Clin Ophthalmol. 2013;7:2019-30.
3. Jonas JB, Nangia V, Matin A, et al. Prevalence and associations of keratoconus in rural maharashtra in central india: The central india eye and medical study. Am J Ophthalmol. 2009;148:760-5.
4. Pearson AR, Soneji B, Sarvananthan N, et al. Does ethnic origin influence the incidence or severity of keratoconus? Eye (Lond). 2000;14:625-8.
5. Mas-Tur V, MacGregor C, Jayaswal R, et al. A review of keratoconus: Diagnosis, pathophysiology and genetics. Surv Ophthalmol. 2017;62:770-83.
6. Merdler I, Hassidim A, Sorkin N, et al. Keratoconus and allergic diseases among israeli adolescents between 2005 and 2013. Cornea. 2015;34:525-9.
7. Shajari M, Eberhardt E, Muller M, et al. Effects of atopic syndrome on keratoconus. Cornea. 2016;35:1416-20.
8. Jhanji V, Sharma N, Vajpayee RB. Management of keratoconus: Current scenario. Br J Ophthalmol. 2011;95:1044-50.
9. Asiedu K, Kyei S, Ampiah EE. Autorefraction, retinoscopy, javal's rule, and grosvenor's modified javal's rule: The best predictor of refractive astigmatism. J Ophthalmol. 2016;2016:1-6.
10. Goebels S, Kasmann-Kellner B, Eppig T, et al. Can retinoscopy keep up in keratoconus diagnosis? Cont Lens Anterior Eye. 2015;38:234-9.
11. Mahmoud AM, Nunez MX, Blanco C, et al. Expanding the cone location and magnitude index to include corneal thickness and posterior surface information for the detection of keratoconus. Am J Ophthalmol. 2013;156:1102-11.
12. Kinori M, Gomi CF, Ondeck CL, et al. Usefulness of refractive measurement of wavefront autorefraction in patients with difficult retinoscopy. J AAPOS. 2016;20:493-5.e1.
13. Albert DM, Bartley GB. A proposal to improve ophthalmic education in medical schools. Ophthalmology. 2014;121:1157-9.
14. Androwiki JE, Scravoni IA, Ricci LH, et al. Evaluation of a simulation tool in ophthalmology: Application in teaching funduscopy. Arq Bras Oftalmol. 2015;78:36-9.
15. Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: A systematic review and meta-analysis. JAMA. 2011;306:978-88.
16. Barsuk JH, Cohen ER, Wayne DB, et al. A comparison of approaches for mastery learning standard setting. Acad Med. 2018;93:1079-84.
17. Hilty DM, Turvey C, Hwang T. Lifelong learning for clinical practice: How to leverage technology for telebehavioral health care and digital continuing medical education. Curr Psychiatry Rep. 2018;20:15-25.
18. Gomez-Perez E, Ostrosky-Solis F. Attention and memory evaluation across the life span: Heterogeneous effects of age and education. J Clin Exp Neuropsychol. 2006;28(4):477-94.
19. Carriere JS, Cheyne JA, Solman GJ, Smilek D. Age trends for failures of sustained attention. Psychol Aging. 2010;25:569-74.
20. Leitritz MA, Ziemssen F, Suesskind D, et al. Critical evaluation of the usability of augmented reality ophthalmoscopy for the training of inexperienced examiners. Retina. 2014;34:785-91.
21. Hoeg TB, Sheth BP, Bragg DS, Kivlin JD. Evaluation of a tool to teach medical students direct ophthalmoscopy. WMJ. 2009; 108:24-6.
22. Schuppe O, Wagner C, Koch F, Manner R. EYESi ophthalmoscope - a simulator for indirect ophthalmoscopic examinations. Stud Health Technol Inform. 2009;142:295-300.
23. Akaishi Y, Otaki J, Takahashi O, et al. Validity of direct ophthalmoscopy skill evaluation with ocular fundus examination simulators. Can J Ophthalmol. 2014;49:377-81.
24. Ament CS, Henderson BA. Optimizing resident education in cataract surgery. Curr Opin Ophthalmol. 2011;22:64-7.
25. Baxter JM, Lee R, Sharp JA, Foss AJ, Intensive Cataract Training Study Group. Intensive cataract training: A novel approach. Eye (Lond). 2013;27:742-6.
26. Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37:1756-61.
27. Clarkson JG. Training in ophthalmology is critical for all physicians. Arch Ophthalmol. 2003;121:1327.
28. Antona B, Barra F, Barrio A, et al. Validity and repeatability of a new test for aniseikonia. Invest Ophthalmol Vis Sci. 2007;48:58-62.
29. Antona B, Barra F, Barrio A, et al. The validity and repeatability of the new aniseikonia test. Optom Vis Sci. 2006;83:903-9.
30. Pinheiro FI, Azevedo EP, Meneses AC, et al. A virtual simulator as a tool for teaching refractometry. GRANTHAALAYAH. 2017;5:23-33.
AUTHOR'S INFORMATION


Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Received on:
June 25, 2019.
Accepted on:
September 27, 2019.