Andrea Pulchinelli Ferrari1; Marcelo Fernandes da Costa2
DOI: 10.17545/eOftalmo/2019.0028
ABSTRACT
This article seeks to start the determination of paw normative values the oculomotor behavior in disjunctive movements of convergence and divergence near and far in trying to guide the clinical activities of orthoptics and ophthalmology.
Keywords: Orthoptics; Astenopia; Ocular convergence; Binocular vision.
RESUMO
Esse artigo busca iniciar a determinação de valores normativos para o comportamento oculomotor nos movimentos disjuntivos de convergência e divergência, para perto e para longe, na tentativa de nortear a avaliação ortóptica e os exercícios ortópticos.
Palavras-chave: Ortóptica; Astenopia; Convergência ocular; Visão binocular.
INTRODUCTION
The reference values of the fusional amplitudes to evaluate extrinsic ocular motility have become a topic of discussion in recent years owing to the lack of updated scientific research. Most studies in which normality values have been presented were conducted in the 1980s when visual demand, mainly for the near range, was much lower than the current one(1-2).
It is empirically observed that visual stimuli, especially that of near vision, occur earlier in recent generations owing to the use of computers, video games, and mobile phones, along with the literacy process initiating earlier. Based on empirical observations, we question whether the reference values of vergence amplitude used by orthoptic consultants would require updates. Additionally, we noted that even the regularly used values do not have updated studies conducted on them.
Vergential movements, or vergences, are binocular, coordinated, and disjunctive eye movements in the same path but opposite directions, which seek to adapt their relative parallel position to allow images located at different distances of the individual to stimulate binocularly corresponding retinal areas, making sensorial fusion of the image possible.
Eye movements for fusional convergence are the broadest, wherein values of ≥30Δ are commonly found. Conversely, eye movements of fusional divergence are smaller, reaching values of up to 8Δ(3). These eye movements can relatively vary among people, but through orthoptic exercises, they can be modified with respect to their amplitude and stability(4).
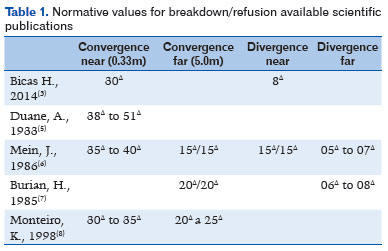
Duane(5) measured the amplitude of vergential movements in a group of normal subjects aged 16–40 years. In 60% subjects, fusional amplitude of convergence ranged between 38Δ (minimum) and 51Δ (maximum). However, there is lack of information on the measurement characteristics. Thus, based on the values presented in this classic study(5), the most likely hypothesis is that these were measurements performed for near visual fixation. The authors also concluded that age has little effect on the fusional amplitude and that frequent eye activity through orthoptic exercises is the most important factor.
Joyce Mein(6) considers normality values of 15Δ/15Δ for distant convergence amplitudes (fusional and refusional breaking values) and 35Δ–40Δ for near convergence. Values for distant divergence were 5Δ–7Δ and those for near divergence were 15Δ–15Δ; the authors did not describe the evaluation method used. Burian(7) only referred to distant amplitudes, considering 20Δ/20Δ for convergence and 6Δ–8Δ for divergence, without mentioning the method applied.
The authors of Monteiro’s chapter(8), the study with a more complete description of convergence amplitudes, found distant values of 20Δ–25Δ and near ones of 30Δ–35Δ, as evaluated using the prism bar.
These values are presented in table 1, in which the first and second values cannot be mistaken with breaking/refusion because there is no clarity in the description of the methods used.
The discrepancy of normative values found in the literature(5-7), along with the lack of recent studies with appropriate description of the equipment and procedures used, always hindered the classification of vergential, normal, and reduced amplitudes as well as the diagnosis of patients with disturbed binocular vision or convergence insufficiency. Moreover, changes in current visual behaviors requiring a greater demand for binocular movements from an early age have motivated the present study.
Thus, we aimed to determine normative values for the oculomotor behavior of the fusional amplitudes of convergence and divergence for activities conducted at a distance (5m) and near (33cm) in subjects living in the city of São Paulo, Brazil.
METHODS
We selected 35 subjects, 24 females and 11 males, aged 4–39 years (mean 15.2 years; SD=9.9; median=11 years). The sample size was determined by considering mean values from the literature for a sample power of 0.80 and a significance level of 0.05.
The inclusion criteria were as follows: asymptomatic individuals(9), distant visual acuity of recognition (optotypes) of 1.0 (Snellen decimal) or better in both eyes, near visual acuity of recognition J1 (Jaeger) measured at 0.37m in both eyes, always with the best refraction optical correction (considered to be emmetropia if up to 1.50 SPH and/or 1.00 CYL); orthophoria or low phoria (near exophoria up to 4Δ and distant up to 3Δ; near esophoria up to 2Δ and distant up to 1Δ); no hyper or hypofunctions of the ocular extrinsic muscles; near point of convergence (NPC) of ≤6.0cm, considered normal in this way(10); stereoscopic acuity of 40’’ of arc measured with a Titmus Stereo Fly.
We excluded patients with any history of eye surgery; reference to episodes of paretic, paralytic, or restrictive oculomotor alteration, or constant or intermittent eye deviations (heterotropies) in any look positions.
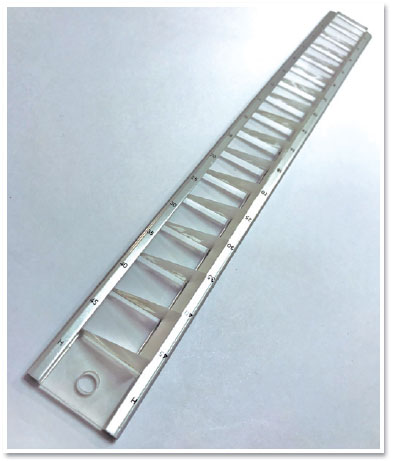
The prism bar (Gulden Ophthalmics, Elkins Park, PA, USA) used features of 15 prisms made of PMMA (acrylic) ranging from 2Δ to 45Δ (Figure 1), scaled as 2Δ, 4Δ, 6Δ, 8Δ, 10Δ, 12Δ, 14Δ, 16Δ, 18Δ, 20Δ, 25Δ, 30Δ, 35Δ , 40Δ, and 45Δ .
The subjects were individually checked in an examination room equipped to perform an orthoptic evaluation after ophthalmic evaluation and prescription of spectacles if necessary, in the following order of examination:
1. Anamnese;
2. Distant and near visual acuity;
3. Verification of binocular positioning in the primary eye position, with measurements using cover test and prisms;
4. Binocular rotations;
5. Verification of the binocular positioning in all diagnostic positions with cover test and prisms;
6. NPC with properly positioned millimeter ruler and aiming with accommodative figure stimulus;
7. Stereotopic acuity with Titmus Stereo Fly.
Fusional amplitude measurements were obtained at a distance (5m) and near (33cm) of convergence and divergence using the prism bar, intentionally with an interposed sequence of convergence and divergence and never exceeding the maximum values previously established, as follows: distant convergence of 25Δ and near convergence of 45Δ as well as distant divergence of 8Δ and near divergence of 14Δ. In the measurements, 2 values were considered, the first being recorded as fusion break and the second as fusion restored and without additional stimuli, such as blinking or looking at a lower position, considering that stimuli (encouragement by the examiner) may overestimate convergence(11,12); there is also the possibility of not breaking the fusion, indicated as without breaking (NBF).
In the measurements, we followed the following 4 sequences, interspersing convergence and divergence:
a) Distant Nasal (DN), distant temporal (DT), near nasal (NN), and near temporal (NT), with 11 patients in this group
b) NT, DN, DT, and NN, with 6 patients in this group
c) NN, NT, DN, and DT, with 11 patients
d) DT, NN, NT, and DN, with 7 patients in this group
It is important to note that a prism placed in front of one eye projects a second image shifted to the side of the base of this prism, causing diplopia. Thus, a nasal-based prism projects a second image nasally, forcing the patient to diverge to obtain a fusion of the images; hence, the divergence fusional amplitude is determined at the maximum prismatic value at which the patient was able to merge the diplopic images. Alternatively, a temporal-based prim projects a second image, temporally forcing the patient to converge to obtain a fusion of the diplopic images, resulting in the fusional amplitude of convergence.
RESULTS
The mean near fusional convergence was 45Δ; however, 52.77% patients did not present fusion break (NBF) up to this value, and the remaining obtained mean refusion at 43.13Δ (SD=2.4, median=45.0). The mean near fusional divergence was 14Δ; however, 66.66% patients did not present fusion break (NBF) up to this value, and the remaining obtained mean refusion at 13.64Δ (SD=0.8, median=14.0). The mean distant fusional convergence was 24.8Δ (SD=0.8, median=25.0), with 44.44% patients without fusion break (NBF) up to this value, and the remaining with mean refusion at 21.6Δ (SD=2.3, median=20.0). The mean distant fusional divergence was 7.9Δ (SD=0.3, median=8.0), and the remaining patients obtained mean refusion at 6.3Δ (SD=0.7, median=6.0). Table 2 shows the values obtained in the evaluations.
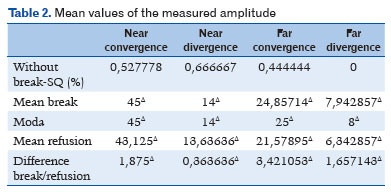
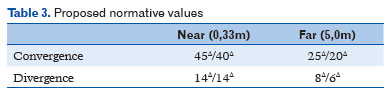
There were no significant effects of age (p>0.05) or the sequence used (p>0.05). No significant correlations between age and fusional amplitude were found. Thus, as a first approach, normal fusional amplitudes measured with the prism bar are arranged in table 3.
DISCUSSION
A distant convergence ranging between 20Δ and 25Δ, a near convergence ranging from 35Δ to 45Δ, a distant divergence from 8Δ to 6Δ, and a near divergence of 14Δ are considered clinically normal if evaluated with a prism bar in most orthoptic clinics in Brazil. These values were determined through a quick and informal interview with Brazilian orthoptists and research data were not properly recorded, a fact that stimulated interest in determining normative values. Our study establishes normative values for convergence and divergence, both for breakage and refusion. With the establishment of these values and their respective uses, the diagnosis of amplitude and fusional stability may be more effective in clinical practice based on current scientific evidence.
Asthenopic symptoms, associated with binocular vision, may be associated with a reduction in the fusional amplitude, even before the appearance of other clinical signs such as a reduction of the near point convergence or difficult-to-control heterophoria or intermittent heterotropy. The normality values that we have established will be of great diagnostic and therapeutic support for these visual symptomatological conditions, which are increasingly frequent because of the use of electronic devices for near vision.
It is important to consider methodological differences related to fusional vergence measurements. Empirically, it is known that higher values of vergential amplitudes are also found when using the synoptophore because it allows a more gradual and slow modification between convergence and divergence values, even with the greatest natural dissociation caused by the artificiality of the stimuli used. Similarly, lower values are found when using isolated prisms and in intermediate uses with the prism bar because the removal and placement of prisms require extra oculomotor effort that negatively impacts amplitude measurements.
We chose the prism bar for our measurements because it has the advantage of greater portability than the synoptophore and is more practical to handle than a box of isolated prisms, besides avoiding extra efforts that imply increased variability in the measure owing to additional wear. By choice and limitation of the instrument used, it was decided not to verify the limits of the amplitudes, that is, not to go beyond the maximum values of the equipment, a fact that led us to consider the possibility of finding higher values than those found in this study. However, only considering the values we suggest as references present adherence to those used for years in practice by examining orthoptists, emphasizing that we must consider that the methodological limitation may have underestimated the values found by having previously established a ceiling for the measures.
According to the literature data for near convergence fusional amplitudes, measured with prism bar, Scheiman(11) found 19Δ in children aged 6 years and 23Δ in those aged 7–12 years, Chen(13) found 19.4Δ in children aged 7–12 years, Wesson(14) reported 19Δ in children aged 7–12 years, and Jimenez(15) found 18Δ in children aged 6–12 years. The values found in the current study do not follow these data. The near divergence fusional amplitude values found in this study are corroborated by the literature mentioned because Scheiman(11) found 12Δ in children aged 6 years and those aged 7–12 years. Chen(13) did not report corresponding values; Wesson (14) reported 13Δ in children aged 7–12 years-old; and Jimenez(15) indicated 11Δ in children aged 6–12 years.
Recently, Fray(12) established values evaluated with the prism bar that were close to those determined in this study. Fray found maximum values of near convergence fusional amplitudes of 35Δ, of near divergence fusional amplitudes of 16Δ, of distant convergence fusional amplitudes of 26Δ, and distant divergence fusional amplitudes of 7Δ .
In the most recent publication, a systematic review, in 2019(16), studies involving healthy individuals have shown that vergential amplitudes vary as follows: near convergence, the most referenced in the literature among the vergences, varied from 19Δ to 57Δ; distant convergence ranged between 11Δ and 33Δ; near divergence ranged from 8Δ to 22Δ; and distant divergence from 5Δ to 10Δ. Hence, our values are close to those found in recent research.
We should also consider that establishing a random sequence of convergence and divergence, albeit interspersed, may have underestimated the values, especially those of divergence because we know that the divergence assessed after convergence may have been influenced by the absence of complete dissipation of the inervational tonic stimulus applied during convergence measurement.
We conclude our work with the construction of normality values for the amplitude of near- and distant fusional measures that can guide more efficient diagnoses and therapeutic conducts because they will be conducted based on scientific evidence. The normative values are also updated and cover the range of population that uses mobile devices the most and has presented greater asthenopic visual complaints.
REFERENCES
1. Boman DK, Kertesz AE. Fusional responses of strabismics to foveal and extrafoveal stimulation. Invest Ophthalmol Vis Sci. 1985;26(12):1731-9.
2. Wilson HR, Blake R, Pokorny J. Limits of binocular fusion in the short wave sensitive ("blue") cones. Vision Res. 1988;28(4):555-62.
3. Bicas HEA. Fisiologia da visão binocular (Physiology of binocular vision) Arq Bras Oftalmol. 2004;67(1):172-80.
4. Souza-Dias CR. Os estrabismos: teoria e casos comentados / Carlos R. Souza-Dias, Mauro Goldchmit. – Rio de Janeiro: Cultura Médica: Guanabara Koogan, 2011.
5. Duane A. Binocular Moviments. Arch Ophtal. 1933;9:579.
6. Mein J, Harcourt B. Diagnosis and management of ocular motility disorders. Blackwell Scientific Publications, Londres,1986.
7. Burian HM. Anomalies of the convergence and divergence functions and their treatment. Transactions of the New Orleans Academy of Ophthalmology. 1971;223-32.
8. Carlos Souza-Dias, Henderson Celestino de Almeida e Colaboradores - Ed. Roca - 1998 - Capítulo 11, Heteroforias, Keila Mirian Monteiro de Carvalho.
9. Convergence Insufficiency. AAPOS. http://www.aapos.org/terms/conditions/38 (acessado em 07/06/2019).
10. Scheiman MS. Treatment of symptomatic convergence insufficiency in children with a home-based computer orthoptic exercise program. J AAPOS. 2011;15(2):123-4. Doi: 10.1016/j.jaapos.2011.03.001.
11. Scheiman MS, Herzberg H, Frantz K, Margolies M. (1989) A normative study of step vergence in elementary schoolchildren. J Am Optom Assoc. 1989;60:276–80.
12. Fray KJ(2017): Fusional Amplitudes: Developing Testing Standards, Strabismus, DOI: 10.1080/09273972.2017.1349814.
13. Chen AH, Abidin AHZ. Vergence and accommodation system in Malay primary school children. Malaysian J Med Sci. 2002;9:9–15.
14. Wesson MD. Normalization of prism bar vergences. Am J Optom Physiol Opt. 1982;59:628–33
15. Jimenez R, Perez MA, Garcia JA, Gonzalez MD. Statistical normal values of visual parameters that caracterize binocular function in children. Ophthal Physiol Opt. 2004;24:528-42.
16. Lança CC, Rowe FJ. (2019): Measurement of fusional vergence: a systematic review, Strabismus, DOI: 10.1080/09273972.2019.1583675
AUTHOR'S INFORMATION


Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
February 18, 2019.
Accepted on:
October 21, 2019.