Gustavo Henrique de Lima Melillo; Bianca Figueiredo Barczewski; Aline Mota Freitas Matos; Luiza Ribeiro de Lima Brandão
DOI: 10.17545/eOftalmo/2019.0026
ABSTRACT
Complicated pterygium recurrence: a case report reinforcing conjunctival autograft as the technique of choice for the first intervention. Pterygium is a highly prevalent condition of the ocular surface and it is surgically resolved. Historically, several techniques have been used for excision, some of them strongly associated with recurrences and complications. Simple excision, without conjunctival covering, makes the eye susceptible to anomalous healing with the formation of symblepharon. This article reports the case of a patient who underwent multiple pterygium excisions in the left eye without conjunctival covering and developed significant symblepharon. In addition to presenting the limitation of abduction, to the point of causing diplopia in the primary position, the fibrous adhesion reached the lower lacrimal punctum, creating severe epiphora. The patient underwent symblepharon surgery with fornix reconstruction and conjunctival autograft and achieved satisfactory postoperative results. Conjunctival autograft is considered the gold-standard technique for pterygium excision.
Keywords: Pterygium; Conjunctiva; Diplopia.
RESUMO
O pterígio é uma condição da superfície ocular altamente prevalente cuja resolução é cirúrgica. Historicamente, diversas técnicas já foram empregadas para a excisão, algumas delas altamente relacionadas a recidivas e complicações. A excisão simples, sem recobrimento conjuntival, deixa o olho susceptível à cicatrização anômala com formação de simbléfaro. Este trabalho reporta o caso de uma paciente submetida a múltiplas excisões de pterígio no olho esquerdo sem recobrimento conjuntival que evoluiu com a formação de importante simbléfaro. Além de apresentar restrição da abdução a ponto de causar diplopia em posição primária, a trave fibrosa incluía o ponto lacrimal inferior, gerando importante epífora. A paciente foi submetida a simblefaroplastia com reconstrução de fórnices e enxerto de conjuntiva autóloga, apresentando resultado pós-operatório satisfatório. O transplante autólogo de conjuntiva é considerado a técnica padrão-ouro para a excisão do pterígio.
Palavras-chave: Pterígio; Conjuntiva; Diplopia.
RESUMEN
El pterigio es una condición de la superficie ocular altamente prevalente que se soluciona por medio de cirugía. Históricamente, ya se han empleado diversas técnicas para la escisión, algunas de las cuales altamente relacionadas a recidivas y complicaciones. La escisión sencilla, sin el recubrimiento conjuntival, deja el ojo sujeto a la cicatrización anómala con formación de simbléfaro. Este trabajo relata el caso de una paciente sometida a múltiples escisiones de pterigio en el ojo izquierdo sin el recubrimiento conjuntival, que evolucionó con la formación de un importante simbléfaro. Además de presentar restricción de la abducción a punto de causar diplopía en posición primaria, el arco fibroso incluía el punto lacrimal inferior, generando importante epífora. Se sometió la paciente a simblefaroplastía con reconstrucción de fórnices e injerto de conjuntiva autóloga, presentando resultado posoperatorio satisfactorio. El trasplante autólogo de conjuntiva se considera la técnica estándar-oro para la escisión del pterigio.
Palabras-clave: Pterigion; Conjuntiva; Diplopía.
INTRODUCTION
Pterygium is a highly prevalent condition of the ocular surface. Its etiology is multifactorial, and its complete resolution is possible only via surgical removal1-10. It is classified based on the extent of corneal involvement11. Several excision techniques have been described12, some of which are strongly associated with recurrences and complications. Despite being considered a faster and simpler removal method with minimal surgical intervention, simple excision without conjunctival covering makes the eye susceptible to anomalous healing with the formation of a symblepharon12-14. In addition, adjuvant techniques are frequently used to reduce the high risk of recurrence associated with this technique, including conjunctival patch or autograft, intraoperative topical mitomycin C, and beta radiation12.
This study aimed to report the case of multiple recurrences of pterygium following simple excisions, with symblepharon formation, limited abduction, and ectopic lower lacrimal punctum, in which we obtained a satisfactory result using conjunctival autograft. Here, we discuss this technique as the gold standard14-21 for the excision of pterygia.
CASE REPORT
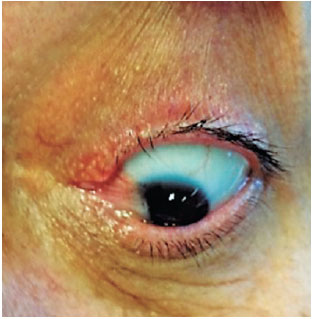
A 52-year-old female patient visited the doctor with complaints of persistent redness in her left eye (OS), binocular diplopia at the slightest attempt of levoversion, and epiphora after multiple surgical interventions for pterygium on the nasal cornea of the OS. The patient reported a total of four previous surgeries of simple excision (bare sclera) followed by rapid recurrence (ranging from weeks to a few months after the procedures). Biomicroscopy showed a slightly hyperemic OS nasal conjunctiva, symblepharon with adherence of the medial corner of both upper and lower eyelids to a recurrent grade-III nasal pterygium, and ectopic lower lacrimal punctum. Fibrosis and adhesions caused total limitation of OS abduction (Figures 1 and 2). The patient underwent surgery for pterygium excision and symblepharon correction with an extensive upper temporal conjunctival transplant from the same eye. The graft was rotated to better cover the bare sclera; it was sutured with simple 10-0 nylon stitches on almost the entire margin and simple 8-0 Vicryl stitches in areas that were more difficult to reach, to be removed later. Local fornices were reconstructed using 6-0 Prolene, and the lower lacrimal punctum was repositioned (Figure 3). Adaptation to a scleral lens for symblepharon was postoperatively attempted; however, the patient presented significant intolerance to it. She was prescribed slow weaning from topical corticosteroids, followed by a long cycle of topical nonsteroidal anti-inflammatory drugs. After 5 months of follow-up, we observed partial retraction of the conjunctival graft and initial revascularization of the nasal corneo-conjunctival area, which caused a slight increase in the abduction limitation compared with that in the immediate postoperative period (Figure 4). Nevertheless, the patient only presented diplopia on extreme levoversion of the OS and did not complain of epiphora.



DISCUSSION
Pterygium is a disorder of the ocular surface, characterized by the neoformation of a triangular-shaped mass of fibrovascular tissue extending from the bulbar conjunctiva to the cornea. In addition to being unaesthetic, it can cause tear film instability, foreign body sensation, burning, irritation, astigmatism, and visual axis obscuration. It has a multifactorial etiology, chiefly related to ultraviolet light exposure1,2. Its prevalence has increased in individuals residing in the equatorial regions and among those who work outdoors3-5.
The mechanisms of pterygium formation remain to be completely understood. Chronic exposure to ultraviolet light is believed to cause oxidative stress to the limbal and conjunctival cells, resulting in damage to the genetic material and stimulation of the inflammatory pathways, thereby inducing a hyperproliferative state6. Moreover, viral infections7, family history8, and deregulation of extracellular matrix modulators9 and growth factors10 also seem to be associated with the development of this condition.
Pterygia can be classified into three types11. Type I is characterized by covering <2mm of the cornea, whereas type II covers between 2 and 4mm. Type III pterygium, as observed in our patient, covers >4mm of the cornea, which can cause reduced visual acuity and lead to limited extiraocular movements and diplopia if combined with extensive subconjunctival fibrosis11.
Regarding treatment, the surgical approach is indicated in case of symptoms of discomfort, astigmatism induction, limited ocular movements, and aesthetic changes12,14. There are several different surgical procedures to treat pterygium, of which we highlight simple excision (with the sclera exposed after surgery), conjunctival autograft, and amniotic membrane transplantation12,13.
For a long time, simple excision was the standard procedure. Although it is considered the fastest and simplest method for the surgical removal of pterygia, scleral exposure followed by conjunctivalization owing to secondary intention is highly associated with recurrence, which may exceed 80%12,14. To decrease the recurrence rate, pterygium excision is often combined with adjuvant techniques such as conjunctival autograft12. In our patient, in addition to recurrences after simple excisions, the exacerbated inflammatory process in the conjunctiva promoted the formation of a significant symblepharon, followed by ocular movement limitation and epiphora.
In conjunctival autograft, the sclera is covered by a conjunctival graft. Positioning the limbal region of the graft over the limbus in the receiving area is recommended, as this would promote the reorganization of a cell barrier that is crucial to prevent relapses15. The donor site is healed by secondary intention, which is not free from potential complications, such as fibrous scarring and even the formation of a local symblepharon16.
Although recurrence rates vary among clinical studies17-21, conjunctival autograft is often considered the most effective method to treat pterygium. A retrospective observational study with a series of 310 pterygia cases that were surgically treated showed a recurrence rate of 5.2% during a mean follow-up period of 20.1±8.6 months15. Moreover, it has been observed that the relapse rate of operated pterygia that were recurrent themselves (12.9%) is higher than that of operated primary pterygia (3.2%)15.
In accordance with the findings of this study, we were unable to prevent the relapse of pterygium in our patient. This corroborates what we routinely observe in our institution, that many patients are referred with complications after bare-sclera pterygium excision.
A long-term study identified similar relapse rates between grafts from the upper and lower bulbar conjunctivae22. Although it concluded that surgery using lower conjunctival grafts has a less painful postoperative period and maintains the upper conjunctiva intact for other ophthalmologic needs (such as glaucoma surgeries)22, most surgeons prefer grafts from the upper region because they are easier to access intraoperatively and can be larger, as noted in our patient.
The amniotic membrane and buccal mucosa, among others, are viable alternatives to cover the recipient site when the bulbar conjunctiva is inaccessible or insufficient23. The graft is usually fixed to the scleral bed using sutures, as performed in our patient, or fibrin glue24.
The literature has shown that rotating the graft for better tissue utilization in covering the recipient site has good results25, which is consistent with what we observed in the present case.
Several adjuvant therapies have been studied to prevent pterygium recurrence in patients undergoing surgery with tissue transplantation. The use of mitomycin C, 5-fluorouracil, beta radiation, ciclosporin, and bevacizumab is not only associated with reduced recurrence rates but also with undesirable side effects23,26.
Mitomycin C is a drug that can inhibit DNA synthesis and fibroblast proliferation in the episclera region, which explains its ability to reduce pterygium recurrence27. A meta-analysis has shown that the combination of conjunctival autograft with ciclosporin 0.05% was more effective in reducing pterygium recurrence than the use of conjunctival graft alone28.
We did not prescribe our patient any of the above mentioned drugs; however, we employed a long cycle of topical steroids and nonsteroidal anti-inflammatory drugs to reduce the tendency of inflammation.
Thus, it can be observed that the technique without conjunctival covering and a short postoperative topical anti-inflammatory treatment are determining factors for recurrences. The fact that, although the pterygium has relapsed in the postoperative follow-up, there were no associated complications, is attributed to the autograft technique.
CONCLUSION
The case reported and publications reviewed reinforce the conjunctival autograft technique as the method of choice for the primary surgical approach for pterygium as it reduces the occurrence of relapses and postoperative complications that are difficult to treat and control in the long term.
REFERENCES
1. Yam JC, Kwok AK. Ultraviolet light and ocular diseases. Int Ophthalmol. 2014 Apr;34(2):383-400.
2. Delic NC, Lyons JG, Di Girolamo N, Halliday GM. Damaging effects of ultraviolet radiation on the cornea. Photochem Photobiol. 2017 Jul;93(4):920-929.
3. Cameron ME. Pterygium throughout the world. Springfield: Charles C. Thomas; 1965.
4. Rezvan F, et al. Prevalence and risk factors of pterygium: a systematic review and meta-analysis. Surv Ophthalmol. 2018 Sep/Oct;63(5):719-735.
5. Mackenzie FD, Hirst LW, Battistutta D, Green A. Risk analysis in the development of pterygia. Ophthalmology. 1992 Jul;99(7):1056-61.
6. Di Girolamo N, Chui J, Coroneo MT, Wakefield D. Pathogenesis of pterygia: role of cytokines, growth factors, and matrix metalloproteinases. Prog Retin Eye Res. 2004 Mar;23(2):195-228.
7. Otlu B, Emre S, Turkcuoglu P, Doganay S, Durmaz R. Investigation of human papillomavirus and Epstein-Barr virus DNAs in pterygium tissue. Eur J Ophthalmol. 2009 Mar/Apr;19(2):175-179.
8. Anguria P, Kitinya J, Ntuli S, Carmichael T. The role of heredity in pterygium development. Int J Ophthalmol. 2014;7(3):563-573.
9. Riau AK, Wong TT, Lan W, et al. Aberrant DNA methylation of matrix remodeling and cell adhesion related genes in pterygium. PLoS One. 2011 Feb;6(2):e14687.
10. Kria L, Ohira A, Amemiya T. Immunohistochemical localization of basic fibroblast growth factor, platelet derived growth factor, transforming growth factor-beta and tumor necrosis factor-alpha in the pterygium. Acta Histochem. 1996 Apr;98(2):195-201.
11. Alves MR, Höfling-Lima AL, Nishiwaki-Dantas MC. Doenças Externas Oculares e Córnea. Série Oftalmologia Brasileira. Conselho Brasileiro de Oftalmologia (CBO). 3ª ed. Rio de Janeiro: Cultura Médica, Guanabara Koogan; 2013.
12. Hirst LW. The treatment of pterygium. Surv Ophthalmol. 2003 Mar/Apr;48(2):145-180.
13. Aminlari A, Singh R, Liang D. Management of Pterygium. EyeNet. 2010 Nov/Dec;37-38.
14. Tan DT, Chee SP, Dear KB, Lim AS. Effect of pterygium morphology on pterygium recurrence in a controlled trial comparing conjunctival autografting with bare sclera excision. Arch Ophthalmol. 1997 Oct;115(10):1235-40.
15. Aidenloo NS, Motarjemizadeh Q, Heidarpanah M. Risk factors for pterygium recurrence after limbal-conjunctival autografing: a retrospective, single-centre investigation. Jpn J Ophthalmol. 2018 May;62(3):349-356.
16. Starck T, Kenyon KR, Serrano F. Conjunctival autograft for primary and recurrent pterygia: surgical technique and problem management. Cornea. 1991 May;10(3):196-202.
17. Ozer A, Yildirim N, Erol N, Yurdakul S. Long-term results of bare sclera, limbal-conjunctival autograft and amniotic membrane graft techniques in primary pterygium excisions. Ophthalmologica. 2009;223(4):269-73.
18. Hirst LW. Recurrence and complications after 1000 surgeries using pterygium extended removal followed by extended conjunctival transplant. Ophthalmology. 2012 Nov;119(11):2205-10.
19. Hirst LW. Recurrent pterygium surgery using pterygium extended removal followed by extended conjuctival transplant: recurrence rate and cosmesis. Ophthalmology. 2009 Jul;116(7):1278-86.
20. Riordan-Eva P, Kielhorn I, Ficker LA, Steele AD, Kirkness CM. Conjunctival autografting in the surgical management of pterygium. Eye (Lond). 1993;7(Pt 5):634-8.
21. Han SB, Hyon JN, Hwang JM, Wee WR. Efficacy and safety of limbal-conjunctival autografting with limbal fixation sutures after pterygium excision. Ophthalmologica. 2012;227(4):210-4.
22. Zloto O, Rosen N, Leshno A, Rosner M. Very long term success of pterygium surgery with conjunctival graft. Cont Lens Anterior Eye. 2017 Aug;40(4):267-269.
23. Mai C, Bertelmann E. Oral mucosal grafts: old technique in new light. Ophthalmic Res. 2013;50(2):91-98.
24. Koranyi G, Seregard S, Kopp ED. Cut and paste: a no suture, small incision approach to pterygium surgery. Br J Ophthalmol. 2004 Jul;88(7):911-914.
25. Gargallo-Benedicto A, et al. Large pterygium surgery: When coverage of the scleral bed justifies graft rotation. Arch Soc Esp Oftalmol. 2016 Oct;91(10):469-74.
26. Hovanesian JA, Starr CE, Vroman DT, ASCRS Cornea Clinical Committee, et al. Surgical techniques and adjuvants for the management of primary and recurrent pterygia. J Cataract Refract Surg. 2017 Mar;43(3):405-419.
27. Martins TGS, Costa ALFA, Alves MR, Chammas R, Schor P. Mitomycin C in pterygium treatment. Int J Ophthalmol. 2016 Mar;9(3):465-468.
28. Fonseca EC, Rocha EM, Arruda GV. Comparison among adjuvant treatments for primary pterygium: a network meta-analysis. Br J Ophthalmol. 2018 Jun;102(6):748-756.



Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Received on:
April 4, 2019.
Accepted on:
August 30, 2019.