Leonel Telles de Menezes Morais1; Alberto Basile Neto2; Laís Soares de Carvalho3; Jonas Rufino Silva Neto4; Mario Henrique Camargos de Lima5
DOI: 10.17545/eoftalmo/2019.0010
ABSTRACT
INTRODUCTION: Peripheral hypertrophic subepithelial corneal degeneration was first described in 2003. Although its etiology is unknown, it is histologically characterized as a fibrovascular proliferation between the epithelium and Bowman’s layer, with the absence of a clear corneal interval.
CASE REPORT: Here, we present the phenotypical description of a 70-year-old female patient complaining of chronic nonspecific ocular discomfort and presenting with bilateral raised fibrotic subepithelial corneal lesions.
DISCUSSION: The patient in question meets the following five key diagnostic criteria: perilimbal subepithelial fibrosis with a thickened cornea, neovascularization, 2 D or more of astigmatism with regular or irregular topography, pruritus, and bilateral fibrosis.
CONCLUSION: This case report is essential for the phenotypical description of a rare disease. The patient meets all the diagnostic criteria, and therefore, helps to define a disease that is still scarcely reported in the literature.
Keywords: Cornea; Corneal Topography; Corneal Diseases; Corneal Injuries; Corneal Opacity.
RESUMO
INTRODUÇÃO: A Degeneração subepitelial hipertrófica periférica foi descrita inicialmente em 2003 e apresenta etiologia desconhecida e histologicamente caracteriza-se como uma proliferação fibrovascular entre o epitélio e a camada de Bowman, com a ausência de intervalo de córnea clara.
RELATO DE CASO: Descrito o fenótipo de uma paciente do sexo feminino, 70 anos, apresentando queixa de desconforto ocular inespecífico crônico e lesões corneais subepiteliais bilaterais fibróticas e sobrelevadas.
DISCUSSÃO: A paciente em análise preenche os cinco critérios chave para degeneração subepitelial hipertrófica periférica: fibrose subepitelial perilimbar, espessamento da córnea, neovascularização, 2D ou mais de astigmatismo regular ou irregular, prurido, fibrose bilateral.
CONCLUI-SE: O relato de caso é essencial para a descrição fenotípica de uma doença rara. A paciente preenche todos os critérios e auxilia na definição de uma patologia ainda escassa na literatura.
Palavras-chave: Córnea; Topografia da Córnea; Doenças da Córnea; Lesões da Córnea; Opacidade da Córnea.
RESUMEN
INTRODUCCIÓN: La Degeneración subepitelial hipertrófica periférica fue descrita inicialmente en el año 2003 y presenta etiología desconocida e histológicamente se caracteriza como una proliferación fibrovascular entre el epitelio y la membrana de Bowman, con la ausencia de intervalo de córnea clara.
RELATO DE CASO: Descrito el fenotipo de una paciente del sexo femenino, 70 años, que presenta quejas de incomodidad ocular inespecífica crónica y lesiones corneales subepiteliales bilaterales fibróticas y sobrelevadas.
DISCUSIÓN: La paciente en análisis rellena los cinco criterios llave para degeneración subepitelial hipertrófica periférica: fibrosis subepitelial perilimbar, engrosamiento de la córnea, neovascularización, 2D o más de astigmatismo regular o irregular, eczema, fibrosis bilateral.
SE CONCLUYE: El relato de caso es esencial para la descripción fenotípica de una enfermedad rara. La paciente rellena todos los criterios y auxilia en la definición de una patología aún escasa en la literatura.
Palabras-clave: Córnea; Topografía de la Córnea; Enfermedades de la Córnea; Lesiones de la Cornea; Opacidad de la Córnea.
INTRODUCTION
Peripheral hypertrophic subepithelial corneal degeneration (PHSD) is a rare disorder of the perilimbal region of the eye. It is usually bilateral, slowly progressive, and occurs predominantly in females1-4. The disease was first described in 2003 and the literature includes series of cases and scarce histological studies describing it2.
Some authors believe that the histological changes found in PHSD are variants of those found in Salzmann’s nodular degeneration or those in the previously described familial pterygoid corneal degeneration3,5.
The etiology of the disease is still unknown. It is histologically characterized as a fibrovascular proliferation between the epithelium and Bowman’s layer, with the absence of a clear corneal interval, and is preferentially located in an exposed interpalpebral area1-4.
The most commonly described symptoms are nonspecific ocular discomfort and a reduction in visual acuity induced by astigmatism, which may be regular or irregular2-4.
Biomicroscopic examination reveals nodular lesions with a whitish aspect, located either in the periphery or in the middle periphery of the cornea3-5.
Although one of the criteria for defining the disease is the absence of chronic ocular inflammation, immunohistochemical studies reveal some mild inflammation leading to low TGFβ1 concentrations4.
The primary differential diagnosis would be with Salzmann’s nodular degeneration. Salzmann’s nodules are white subepithelial corneal opacities with a peripheral circular pattern. Salzmann’s nodular degeneration is predominantly unilateral, occurs more commonly in females, and has a controversial physiopathology. Some authors believe that chronic ocular irritation and inflammation are prerequisite conditions for the disease to develop1-5.
CASE REPORT
A 70-year-old female patient, Caucasian, born and residing in São Paulo, was referred to the Ophthalmological Service of our hospital complex, complaining of chronic nonspecific ocular discomfort and progressive low visual acuity (BAV) in both eyes (OU) since approximately 4 years before..
Corrected visual acuity of 20/40 (logMAR 0.3) OU, using lenses for:
Right eye: +7.75 spherical diopters, −2.00 cylindrical diopters at 90°.
Left eye: +8.00 spherical diopters, −2.00 cylindrical diopters at 90°.
Red reflex and direct and consensual pupillary reflexes with no changes were observed.
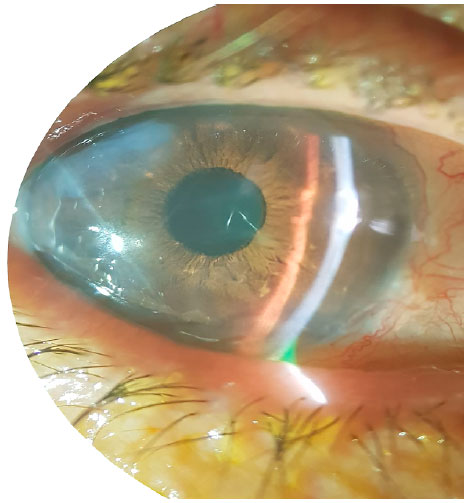
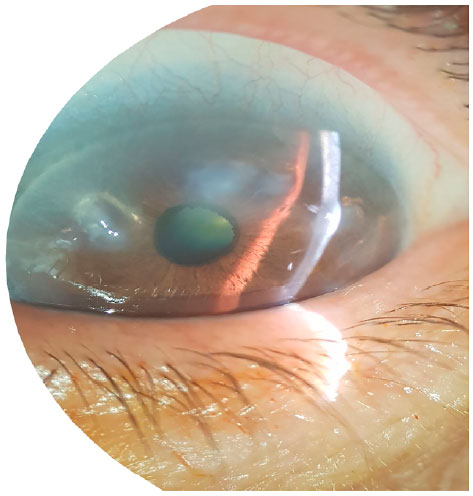
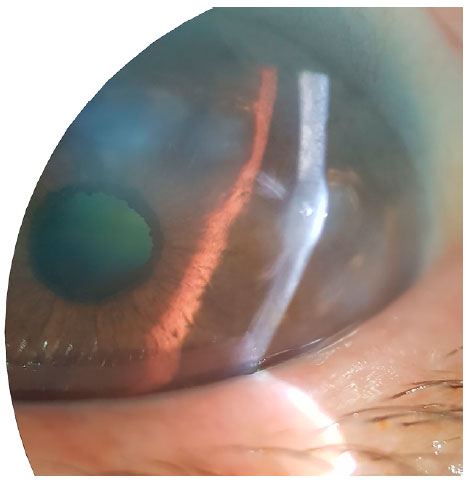
Biomicroscopy: Threads eyelashes, clear conjunctiva, cornea with peripheral, white, raised, circular, nodular lesions with a cicatricial aspect OU (Figures 1–3), Broad anterior chamber, trophic irises, lens opacification from nuclear cataracts 1+/4+ OU.
Goldmann tonometry: 10 mmHg OU at 09:30.
Fundoscopy: No changes.
Corneal topography: Displayed irregular astigmatism induced by peripheral flattening. It was possible to observe that light capture was impaired by the corneal irregularity (Figures 4–7).
DISCUSSION
The patient is female and Caucasian, as in the initial studies on PHSD, in which female patients predominated2. Moreover, Gore et al. 2013 presented a series of 22 cases, all of which were Caucasian and only 2 were males.
The age of the patient in the current case report is 70 years, which is 10 years more than the mean age reported in other studies3,4.
In addition, the patient meets the following diagnostic criteria proposed by Järventausta et al. 2014:
1. Confluent perilimbal subepithelial fibrosis with a thickened cornea, which may or may not extend to the middle periphery of the cornea, but not to the central cornea;
2. Superficial corneal neovascularization, which does not extend beyond the base of the fibrous tissue and does not feature deep stromal vessels;
3. 2 D or more of astigmatism, with regular or irregular topography;
4. Mild pruritus or burning sensation and superficial ocular irritation due to irregular corneal surface;
5. a) Bilateral fibrosis located in a superior region, particularly the superior nasal region;
b) Female gender.
Moreover, the patient does not have a history of chronic inflammation (suggestive of Salzmann’s nodular degeneration) and presents bilateral lesions (suggestive of PHSD).
The symptoms of chronic superficial ocular irritation exhibited by the patient agree with the initial description of the disease, in which all the six patients studied presented with irritation symptoms1. In other studies, 45%–64% of the participants complained of superficial discomfort3,4.
The biomicroscopic changes found in the patient agree with the characteristics and diagnostic criteria for PHSD.
CONCLUSION
Because PHSD is a rare disease only recently described in the medical literature (2003), case reports are essential to define its diagnostic criteria and to discuss possible etiologies and treatments.
REFERENCES
1. Jeng BH, Millstein ME. Reduction of hyperopia and astigmatism after superficial keratectomy of peripheral hypertrophic subepithelial corneal degeneration. Eye Contact Lens. 2006; 32:153-156.
2. Maust HA, Raber IM. Peripheral hypertrophic subepithelial corneal degeneration. Eye Contact Lens. 2003; 29:266-269.
3. Gore DM, Iovieno A, Connell BJ, Alexander R, Meligonis G, Dart JK. Peripheral hypertrophic subepithelial corneal degeneration: nomenclature, phenotypes, and long-term outcomes. Ophthalmology. 2013; 120(5):892-898.
4. Järventausta PJ, Tervo TMT, Kivelä T, Holopainen JM. Peripheral hypertrophic subepithelial corneal degeneration – clinicaland histopathological features. Copenhagen: Acta Ophthalmol. 2014; 92:774-782.
5. Schargus M, Kusserow C, Schlötzer-Schrehardt U, Hofmann-Rummelt C, Schlunck G, Geerling G. Peripheral hypertrophicsubepithelial corneal degeneration presenting with bilateralnasal and temporal corneal changes. Eye. 2015; 29:88-97.

Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: The authors have no potential conflicts of interest to disclose
Received on:
November 20, 2018.
Accepted on:
February 26, 2019.