Juliano De Marchi Silveira1; Bruna Oliveira Vitor2; Kellen Cristiane do Vale Lucio3
DOI: 10.17545/eoftalmo/2019.0009
ABSTRACT
Ophthalmic herpes zoster (OHZ) is the reactivation of varicella-zoster virus (VZV) in the ophthalmic branch of the trigeminal nerve. This condition occurs more frequently in elderly individuals and immunocompromised patients. Optic neuritis, an extremely rare sequela of HZ, occurs either simultaneously with the acute vesicular rash or, more frequently, as a postherpetic complication. Here we report the case of a 62-years-old woman who developed optic neuritis approximately 15 days after the rash, while being treated with a subtherapeutic dose of acyclovir. Nonetheless, with appropriate treatment, her visual acuity recovered. Thus, complete ophthalmological examination and adequate treatment to prevent irreversible sequelae are considered of utmost importance.
Keywords: Acyclovir; Herpes Zoster Ophthalmicus; Optic Neuritis.
RESUMO
O Herpes Zoster Oftálmico (HZO) é a reativação do vírus varicela-zoster (VZ) no ramo oftálmico do nervo trigêmeo, patologia que acomete mais idosos e pacientes imunocomprometidos. Neurite óptica, sequela muito rara de HZ, pode ocorrer simultaneamente à erupção cutânea vesicular aguda ou, mais frequentemente, como complicação pós-herpética. Este é o relato do caso de uma mulher de 62 anos que desenvolveu a neurite óptica cerca de 15 dias após a erupção cutânea em vigência de tratamento com subdose de aciclovir. Apesar disso, com o tratamento correto teve recuperação da acuidade visual. Considera-se importante valorizar o exame oftalmológico completo e o tratamento adequado para evitar sequelas irreversíveis.
Palavras-chave: Aciclovir; Herpes Zoster Oftálmico; Neurite Óptica.
RESUMEN
El Herpe Zoster Oftálmico (HZO) es la reactivación del virus varicela-zoster (VZ) en la rama oftálmica del nervio trigémino, patología que acomete más a adultos mayores y a pacientes inmunocomprometidos. La neuritis óptica, secuela muy rara de Hz, puede ocurrir simultáneamente a la erupción cutánea vesicular aguda o, más frecuentemente, como complicación post-herpética. Éste es el relato del caso de una mujer de 62 años que desarrolló la neuritis óptica cerca de 15 días tras la erupción cutánea en vigencia de tratamiento con subdosis de aciclovir. Sin embargo, con el tratamiento correcto, tuvo recuperación de su acuidad visual. Se considera importante valorar el examen oftalmológico completo y el tratamiento adecuado para evitar secuelas irreversibles.
Palabras-clave: Aciclovir; Herpes Zóster Oftálmico; Neuritis Óptica.
INTRODUCTION
Ophthalmic herpes zoster (OHZ) is an acute illness characterized by a reactivation of latent varicella-zoster virus (VZV) in the ophthalmic branch of the trigeminal nerve1. The disease occurs through the inflammation of the Gasser (trigeminal) ganglion, from where it spreads through the ophthalmic branch of the trigeminal nerve. Its prodromal phase starts with malaise, headache, fever, and nausea, followed in most cases by pain (varying in severity and type) in the dermatome where later a rash will appear. Pain is experienced 1–10 days before the appearance of rash. The affected area exhibits either paresthesia or hyperesthesia, and it is extremely sensitive to touch. In rare cases, the pain starts simultaneously with the appearance of the rash or may never occur. The vesicular rash is normally unilateral, limited by the median line. Once the disease is established, the headache and malaise are rarely noted, and other systemic symptoms are extremely rare5.
The disease occurs more frequently in elderly individuals and immunocompromised patients, and it can cause several ocular complications, such as epithelial, stromal, and nummular keratitis, glaucoma, iris atrophy, posterior synechia, scleritis, motor disorders, optic neuritis, retinitis, necrosis of the anterior segment, phthisis bulbi, and severe postherpetic neuralgia.
Optic neuritis in such cases is well documented in the literature, but rarely reported as a disease2-4. It frequently manifests as a gradual loss of vision within 1–2 weeks of the appearance of the rash; however, it may occur simultaneously with the vesicular rash. In most cases, an afferent pupillary defect occurs, and on ophthalmological examination, the optic disc may appear normal or exhibit edema and hyperemia. The visual prognosis is usually poor in these patients6.
OBJECTIVE
To report a case of optic neuritis caused by the VZV as a rare complication of a previous picture of OHZ, in an immunocompetent patient who fully recovered her visual acuity.
CASE REPORT
A 62-years-old woman visited the emergency room of the Faculty of Medicine Clinics Hospital with complaints of loss of visual acuity (VA) that persisted for three days in oculus dexter (OD); she was experiencing significant pain and multiple vesicles and crusts in right frontal region in the previous 2 weeks (Figure 1). The patient had been taking an oral subtherapeutic dose of acyclovir (200 mg every 4 hours) for 1 week for herpes zoster.
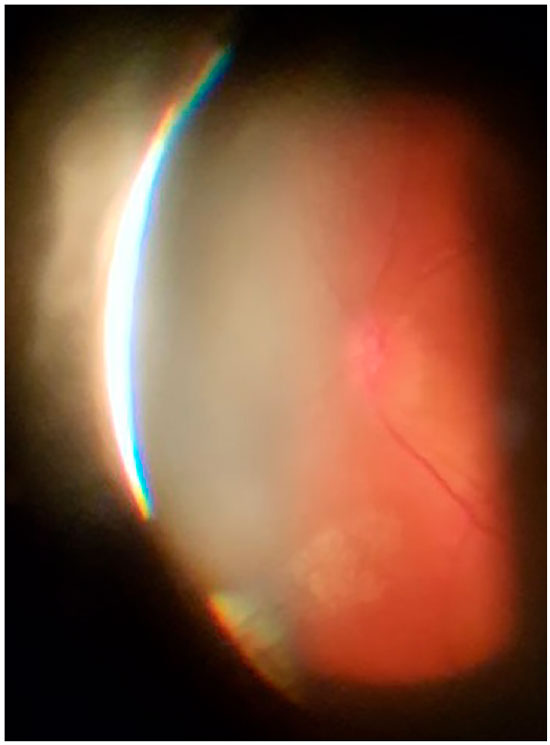
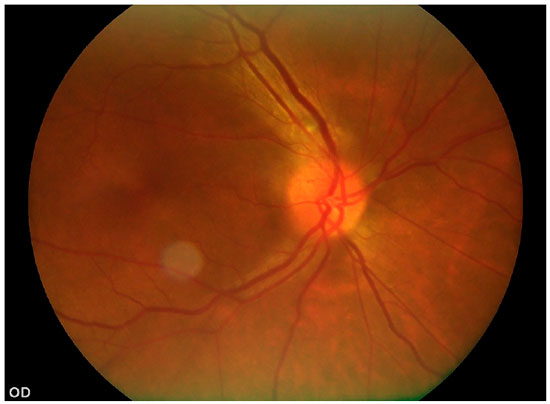
Ophthalmological examination revealed the following: VA 0.3/0.7 (with the stenopeic slit), preserved external ocular motility and direct and consensual pupillary reflexes, and no relative afferent pupillary defect. Biomicroscopy showed fluorescein-stained linear de-epithelialization in the temporal sector and diffuse corneal punctate lesions in OD. Intraocular pressure was not altered. OD fundoscopy revealed an optic disc with poorly defined borders and elevated in the temporal sector, with no other changes (Figure 2). Based on the clinical history and ophthalmological examination, optic neuritis caused by VZV and OHZ was diagnosed.
The patient was hospitalized and administered a course of intravenous acyclovir (10 mg/kg) and prednisone (1 mg/kg) for 7 days. Due to the clinical picture, a clinical investigation was conducted, including an investigation of immunocompetence, in collaboration with the hospital’s neurology and infectiology departments; however, no other disease was found, except diabetes mellitus type 2. After treatment, the patient had a complete regression of the skin lesions, VA of 0.7/0.8 (with the stenopeic slit), and fundus without optic disc elevation, with poorly defined borders only in the superior temporal sector (Figure 3). Fluorescein angiography still demonstrated optic disc hyperfluorescence (Figure 4). The patient is undergoing follow-up by a team of neuro-ophthalmologists and is undergoing pain therapy (due to postherpetic neuralgia).
CONCLUSION
OHZ results from the reactivation of latent VZV in the trigeminal ganglion. Reduced cellular immunity is probably the main cause of VZV reactivation, as most patients have their humoral immunity intact at the reactivation7. Ocular manifestations occur in approximately 17% of OHZ cases8 and they present a varied spectrum of manifestations, including external ocular disease (vesicular rash), anterior segment involvement (interstitial or disciform keratitis, punctate or dendritic epithelial erosion, reduced ocular sensitivity, scleritis, uveitis, and elevated ocular pressure), and posterior segment involvement (retinal vasculitis, choroiditis, and acute retinal necrosis).
Optic nerve involvement is a rare sequela in OHZ and may manifest as papillitis, retrobulbar neuritis, or optic nerve infarction4. The visual prognosis is usually poor in OHZ neuropathy.
The precise mechanism that underlies optic neuropathy in OHZ remains unknown. Optic nerve inflammation may result from direct infection of the nerve through the cavernous sinus9. A second possible mechanism involves a systemic or central nervous system infection with a reactive immune response, leading to optic disc edema. A clear distinction between these two proposed mechanisms is not always possible. A third possible mechanism involves inflammatory demyelination, a condition known as infectious optic neuritis, which can be unilateral or bilateral and develops 1–3 weeks after a viral infection.
Acyclovir is the drug of choice for the treatment of OHZ. The recommended dose is 5–10 mg/kg administered intravenously every 8 hours10, with treatment ideally being initiated in the first 72 hours. The simultaneous use of a corticosteroid and an antiviral drug, although not contraindicated in an immunocompetent patient, remains controversial considering the anti-inflammatory and neuroprotective benefits of the corticosteroid and, the greater risk of suppression of the host’s immunity7. In one study, such therapeutic regimens did not affect postherpetic neuralgia, but the resolution of acute neuritis was faster11.
In the present case, the patient was immunocompetent; however, treatment with a subtherapeutic dose of acyclovir may have been the factor that contributed to optic nerve involvement. In any case of OHZ, it is vital to perform a complete and thorough ophthalmological examination, considering the wide gamut of possible ocular manifestations, which may lead to irreversible visual impairment in some cases. Thus, after OHZ was diagnosed and adequate treatment with intravenous acyclovir and a corticosteroid was administered, the patient exhibited an improvement in the optic disc edema, accompanied with a significant improvement in her VA. It remains to be answered whether this improvement of the VA was related to the fact that the patient was immunocompetent or that the OHZ was promptly treated with a combination of intravenous acyclovir and a systemic corticosteroid, although there is no consensus in the literature regarding this treatment.
REFERENCES
1. Gilden DH, Kleinschmidt-DeMasters BK, LaGuardia JJ, Mahalingam R, Cohrs RJ. Neurologic Complications of the reactivation of varicella-zoster virus. N Engl J Med [Internet]. 2000 Mar 2 [cited 2018 Nov 10]; 342(9):635-645.
2. Marsh RJ, Cooper M. Ophthalmic herpes zoster. Eye [Internet]. 1993 May [cited 2018 Nov 10]; 7(3):350-370.
3. Lexa FJ, Galetta SL, Yousem DM, Farber M, Oberholtzer JC, Atlas SW. Herpes zoster ophthalmicus with orbital pseudotumor syndrome complicated by optic nerve infarction and cerebral granulomatous angiitis: MR-pathologic correlation. AJNR Am J Neuroradiol [Internet]. [cited 2018 Nov 10]; 14(1):185- 190.
4. Özdemir Ö, Ozdemir O. Bilateral retrobulbar neuritis following unilateral herpes zoster ophthalmicus. Ophthalmologica [Internet]. 1994 [cited 2018 Nov 10]; 208(2):61-64.
5. Ostler HB, Thygeson P. The ocular manifestations of herpes zoster, varicella, infectious mononucleosis, and cytomegalovirus disease. Surv Ophthalmol [Internet]. [cited 2018 Nov 10]; 21(2):148-159.
6. Wang AG, Liu JH, Hsu WM, Lee AF, Yen MY. Optic neuritis in herpes zoster ophthalmicus. Jpn J Ophthalmol [Internet]. [cited 2018 Nov 10]; 44(5):550- 554.
7. Weller TH. Varicella and Herpes Zoster. N Engl J Med [Internet]. 1983 Dec 8 [cited 2018 Nov 10]; 309(23):1434-1440.
8. Schmidt P. Herpes zoster ophthalmicus with retrobulbar neuritis. A case report. Acta Ophthalmol [Internet]. 1983 Jun [cited 2018 Nov 10]; 61(3):501- 509.
9. Monteiro MLR, Zangalli AL. Série oftalmologia brasileira: Neuro-oftalmologia, 1 ed. Guanabara Koogan; 2008.
10. Wood AJJ, Whitley RJ, Gnann JW. Acyclovir: a decade later. N Engl J Med [Internet]. 1992 Sep 10 [cited 2018 Nov 10]; 327(11):782-789.
11. Wood MJ, Johnson RW, McKendrick MW, Taylor J, Mandal BK, Crooks J. A randomized trial of acyclovir for 7 days or 21 days with and without prednisolone for treatment of acute herpes zoster. N Engl J Med [Internet]. 1994 Mar 31 [cited 2018 Nov 10]; 330(13):896-900.


Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: The authors have no potential conflicts of interest to disclose.
Received on:
November 12, 2018.
Accepted on:
February 21, 2019.