Mariana Amaranto de Souza Damásio; Izabela Camargos de Figueirêdo Neves; Henrique Dal Fior Figueiredo; Bruno Freitas Lage; Daniel Barreto Andrade; Jacques Ramos Houly
DOI: 10.17545/eoftalmo/2018.0028
ABSTRACT
This study aim to report a challenging therapeutic approach in a case of circumscribed choroidal hemangioma (CCH). A 48-year-old female patient presented a slow and progressive vision reduction of the left-eye. She was diagnosed with CCH, which is characterized by the presence of a reddish-orange, solitary, subretinal mass in the left eye located along the lower temporal arcade and affecting the macula. The CCH diagnosis was confirmed by B-mode ultrasonography, fluorescein angiography, and optical coherence tomography. The patient had a history of therapeutic failure with transpupillary thermotherapy. Anti-angiogenic treatment was attempted but there was no clinical response. Besides being a benign tumor, CCH may cause significant visual morbidity and has a limited response to anti-angiogenic therapy.
Keywords: Ophthalmology; Hemangioma; Drug Therapy.
RESUMO
Este manuscrito tem como objetivo relatar o desafio terapêutico em um caso de hemangioma circunscrito da coroide. Trata-se de paciente de 48 anos, gênero feminino, que apresentou redução lenta e progressiva da visão do olho esquerdo. Recebeu diagnóstico de hemangioma circunscrito da coroide (HCC) por apresentar à oftalmoscopia binocular indireta do olho esquerdo (OE) massa solitária vermelho-alaranjada, localizada ao longo da arcada temporal inferior, acometendo mácula. A hipótese de HCC foi confirmada por meio de ecografia ocular modo B, angiofluorceinografia (AGF) e tomografia de coerência óptica (OCT). História prévia de falha terapêutica com termoterapia transpupilar (TTT). Indicado tratamento com antiangiogênico, sem nenhuma resposta clínica. O hemangioma circunscrito da coroide, apesar de ser um tumor benigno pode ocasionar significativa morbidade visual com resposta limitada à terapia anti-angiogênica.
Palavras-chave: Oftalmologia; Hemangioma; Tratamento Farmacológico.
RESUMEN
El presente manuscrito tiene como objetivo relatar el desafío terapéutico en un caso de hemangioma circunscrito de la coroide. Se trata de un paciente de 48 años, género femenino, que presentó reducción lenta y progresiva de la visión del ojo izquierdo. Recibió el diagnóstico de hemangioma circunscrito de la coroide (HCC) por presentar en la oftalmoscopia binocular indirecta del ojo izquierdo (OE) una densidad solitaria rojo-anaranjada, localizada a lo largo de la arcada temporal inferior, acometiendo mácula. La hipótesis de HCC se confirmó por medio de ecografía ocular modo B, angiofluorceinografía (AGF) y tomografía de coherencia óptica (OCT). Tenía histórico anterior de falla terapéutica con termoterapia transpupilar (TTT). Indicada terapia con antiangiogénico, sin ninguna respuesta clínica. El hemangioma circunscrito de la coroide, aunque sea un tumor benigno, puede resultar significativa morbidez visual con respuesta limitada a la terapia antiangiogénica.
Palabras-clave: Oftalmología; Hemangioma; Tratamiento Farmacológico.
INTRODUCTION
Choroidal hemangioma is a relatively rare benign tumor, which has two forms of presentation: circumscribed and diffused. The circumscribed form is not associated with systemic disease and may be quiescent for many years, whereas the diffused form affects patients with Sturge-Weber syndrome ipsilateral to the nevus flammeus. Circumscribed choroidal hemangioma (CCH) predominantly affects Caucasians, without gender predilection. It is a congenital lesion although the diagnosis is usually made late in life (25–50 years) because of its insidious presentation1.
Some therapeutic options are available for treating CCH, including transpupillary thermotherapy (TTT), photodynamic therapy (PDT), laser photocoagulation and intravitreous antivascular endothelial growth factor (VEGF) injection. Intravitreous anti-VEGF injection does not satisfactorily improve visual acuity (VA) because it does not promote reabsorption of subretinal fluid of the macular edema associated with CCH2. However, previous studies have reported that anti-VEGF therapy is satisfactory when administered alone and when associated with other therapeutic approaches in order to reach better visual prognosis3.
CASE REPORT
A 48-year-old female patient was admitted at Hilton Rocha Foundation eye care service because of a slow and progressive impairment in her left-eye vision over the past 3 years. Previous examinations had revealed CCH. Her treatment history included TTT, but there was no therapeutic response.
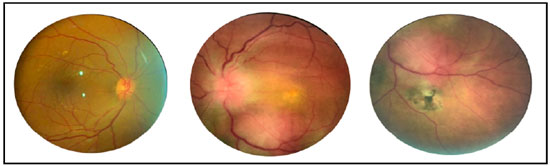
Ophthalmologic examination indicated best-corrected VA of 20/30 and counting fingers at 3 m in the right eye (RE) and left eye (LE), respectively. Biomicroscopic examination of the anterior segment and Goldmann applanation tonometry results were normal in both eyes. Indirect binocular ophthalmoscopy of LE revealed an optic disc with imprecise limits and reddish-orange, solitary, subretinal mass located along the inferior temporal arcade and affecting macular region (Figure 1). Retinography results of RE were unremarkable.
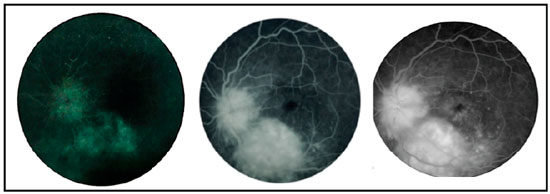
Fluorescein angiography revealed early hyperfluorescence of the lesion with progressive contrast extravasation. Impregnation in the later phases in addition to hyperfluorescence in a petaloid pattern in the central region of the macula was also noted (Figure 2).
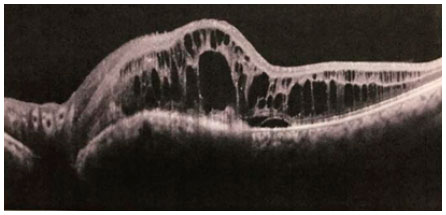
On B-mode ultrasonography, the lesion appeared as a high solid mass, with high internal reflectivity but without acoustic shadow or signs of choroidal excavation. Optical coherence tomography (OCT; Heidelberg® Engineering, Germany) revealed increased retinal thickness, multiple hyporeflective “cystoid” cavitations and subretinal fluid in the foveal region.
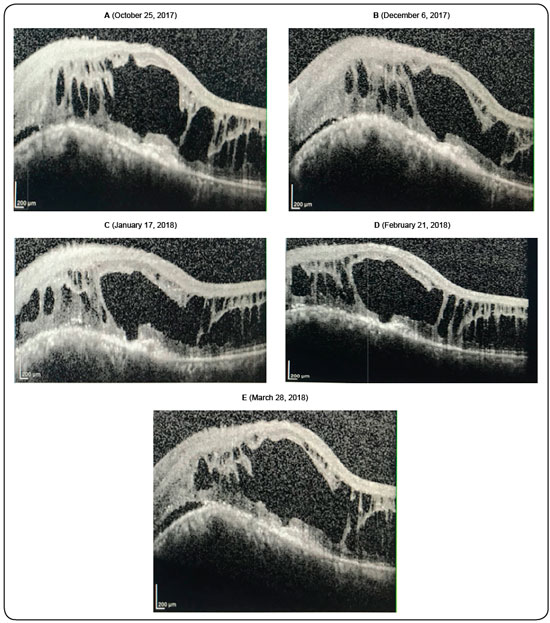
Anti-VEGF therapy was indicated as an attempt to reduce tumor vascular permeability and promote intra- and subretinal fluid reabsorption. The treatment consisted of a sequential intravitreous injections of anti-VEGF in LE (five vials of ranibizumab). Nonetheless, there was no symptomatic improvement or cystoid macular edema regression (Figure 3), as shown on sequential tomographic scans after the injections (Figure 4).
DISCUSSION
There are several therapeutic modalities for CCH, including clinical observation in cases of asymptomatic CCH, TTT, PDT, radiation, photocoagulation, and intravitreous injections of anti-VEGF. All attempts in treating symptomatic CCH are usually towards tumor regression, reduction of subretinal fluid exudation and improvement of VA4,5,6.
TTT uses a diode laser with a wavelength of 810 nm to cause sclerosis of the vascular channels of hemangiomatous lesions, leading to tumor regression and decreased of subretinal fluid production7,8,9. The initial treatment in this case was TTT (performed at another service), which despite having resulted in partial regression of the hemangiomatous lesion did not improve VA, probably due to the persistence of intraretinal fluid and a serous detachment of the retina. Therefore, other TTT sessions were aborted.
PDT is currently the treatment of choice for symptomatic CCH. It targets the tumor area, sparing the retina and overlying vessels using the photosensitive contrast verteporfin associated with a diode laser. PDT has been effective in reabsorbing the fluid produced by the tumor10 and stabilizing or even improving VA by reducing both the retinal fluid and tumor volume2. However, it could not be performed as it was unavailable at the time of diagnosis.
Symptomatic CCH associated with subretinal fluid can also be treated using intravitreous injections of anti-angiogenic agents. Some studies have shown that anti-VEGF (bevacizumab) therapy may reduce tumor-associated exudation, presumably, by depleting endothelial fenestrations and changing intercellular adhesion molecules. Based on these observations, Sagong et al. used anti-angiogenic therapy for treating patients with CCH associated with serous retinal detachment. One patient with a history of unsuccessful laser treatment received bevacizumab alone and achieved complete resolution of the subretinal fluid within 1 month, whereas the other two patients were treated with bevacizumab together with PDT and achieved satisfactory results. However, another study showed that the subretinal fluid persisted in a patient with CCH even after treatment with intravitreal injections of ranibizumab. The patient in this study received sequential intravitreal injections of ranibizumab after TTT; however, we observed no clinical response after five injections. Clinical examination indicated no improvement in VA, and sequential OCT revealed the persistence of retinal exudation with extensive disorganization of the microarchitecture of retinal layers. It is important to note that anti-VEGF therapy has been performed until the judicial release of PDT, which will be the next step in the treatment of this case of CCH.
CONCLUSION
Despite being a benign tumor, CCH represents a therapeutic challenge with limited response to anti-angiogenic therapy, as demonstrated in this case.
REFERENCES
1. Mashayekhi A, Shields CL. Circumscribed choroidal hemangioma. Curr Opin Ophthalmol. 2003;14(3):142-9.
2. Chan LW, Hsieh YT. Photodynamic therapy for choroidal hemangioma unresponsive to ranibizumab. Optom Vis Sci. 2014;91(9):e226-9.
3. Sagong M, Lee J, Chang W. Application of intravitreal bevacizumab for circumscribed choroidal hemangioma. Korean J Ophthalmol. 2009;23(2):127-31.
4. Karimi S, Nourinia R, Mashayekhi A. Circumscribed choroidal hemangioma. J Ophthalmic Vis Res. 2015;10(3):320-8.
5. Rodrigues LD, Serracarbassa LL, Nakashima Y, Serracarbassa PD. Tratamento do hemangioma de coróide e descolamento total da retina com vitrectomia posterior: relato de caso. Arq Bras Oftalmol. 2007;70(3):533-6.
6. Rodríguez CC, González YT, Martinez RR, Pérez MP. Modalidades de tratamiento para el hemangioma coroideo circunscrito. Rev Cubana Oftalmol. 2010;23(Suppl. 1):590-607.
7. Othmane IS, Shields CL, Shields JA, Gunduz K, Mercado G. Circumscribed choroidal hemangioma managed by transpupillary thermotherapy. Arch Ophthalmol. 1999;117(1):136-7.
8. Gündüz K. Transpupillary thermotherapy in the management of circumscribed choroidal hemangioma. Surv Ophthalmol. 2004;49(3):316-27.
9. Roizemblat J, Rosa AAM. Termoterapia transpupilar como opção terapêutica para hemangioma circunscrito de coróide: Relato de caso. Arq Bras Oftalmol. 2002;65(2):257-60.
10. Wang W, Dentler WL, Borchardt RT. VEGF increases BMEC monolayer permeability by affecting occludin expression and tight junction assembly. Am J Physiol Heart Circ Physiol. 2001;280(1):H434-40.


Funding: No specific financial support was available for this study
CEP Approval: Not applicable
Disclosure of potential conflicts of interes: None of the authors have any potential conflict of interest to disclose
Received on:
May 28, 2018.
Accepted on:
July 25, 2018.